Partnership Working in Health and Social Care | Essay
| ✅ Paper Type: Free Essay | ✅ Subject: Social Work |
| ✅ Wordcount: 2970 words | ✅ Published: 14 Aug 2018 |
- Ololade Abasa
Summary of Report
This report looks at how partnership working is developed, the benefits and legislation governing partnership relationship in the UK. And how there is now a shift from professional to patient autonomy. Health and social care is a vast service sector undergoing rapid change, with new government initiatives giving it a higher profile than ever.
The report is a brief overview and not in depth focussing on the main points and benefits of collaborative working and the sharing of information with some focus on Stafford hospital following the Francis report.
A working or collaborative partnership or partnership in general could be defined as “two or more independent bodies working together or collectively to achieve more efficient outcomes than could be possible by working individually or separately” (Joint improvement team 2009). When two people come together to share risks and profits in a business for the good of others. (The concise English dictionary 1992).
The focus today in frontline health and social care is on giving service-users more independence, choice and control. These developments mean there’s greater demand for well-trained multi-agency and multi-skilled collaboration of team’s organizations and people across a range of services giving more opportunities and choice to service users. In this report will focus among other things, looking into working in partnership in the health and social sector in general and some philosophies, concepts, relationships, models and legislation of collaborative and working in partnership.
Different working practices exist across the health and social care sector, which will be part of what this report will also look into briefly with what may be perceived to be barriers to developing an effective partnership relationship within the health and social care sector and strategies that can be developed to improve or overcome these barriers.
Concepts of Partnership Working
For partnership in health and social sector to be successful in delivering services to service users there has to be co-ordination, co-operation and most importantly clear communication between partners for the partnership to survive.
This did not seem to be the case (in our case study) at the Mid Staffordshire NHS foundation trust Stafford hospital in 2007 which led to the public enquiry in 2010 by Robert Francis QC. (The Francis Report).
Some of the philosophies and concepts of working in partnership that will be discussed are:
- Power sharing
- Autonomy
- Making informed choices
- Independence
- Empowerment:
- Respect.
this is giving health care users the choice or opportunity to take care of their health decisions and control their lives if they are capable of doing so (Gibson 1991) patients do have a right to information and choices offered to them.(National Health Care in England (NHS2013)) Health care staff should be encouraged to listen and be involved in decision making that involve their patients’ health care treatment.
Patients unable to make informed choices or decisions regarding their health and treatment should be accorded respect and dignity, by health care professionals who take on such decisions with the patients interests at heart. (Mental Capacity 2005)
Autonomy allows the decision as to will see or attend to their treatment requirements and processes with little or no interference from health care professionals. Autonomy basically gives most of the power of decision making and choice to the patient.
Independence relates to freedom being accorded to service users to feel free in the health and care setting. Service users are allowed privacy and the opportunity to take care of themselves as they desire provided they have the mental capacity and ability to do so. Health care professionals are duty bound to provide up-to-date information to service users regarding patient’s treatment and care and any risks relating to their welfare. (Care Quality Commission).
Collaboration is the lynchpin to power sharing this involves organizations collaborating for a common purpose this enables a common understanding of duties to share and achieve set objectives in a partnership (Gallant et al. 2002).
Respect focusses on offering service users the choice to decide on aspects of their care or health with minimum intervention (Health and social Act 2008) and fairly without any discrimination (Equality Act 2010).
Partnerships have become more necessary today in the health and social care sector, service users issues which atimes could be complex in nature requiring input from a number of professionals and services is more important when designing services than the traditional, centralizing distinctions between community nurses and social workers, or community justice workers and social workers. Different areas and sections of the society have their specific needs and requirements prevalent to the area, for example Enfield may require more specialized care for elderly people than neighbouring or other areas. Also a service user with a health issue may need a particular type of care package that was previously available or provided by the national health service and social services, in the new way of working together the health and social care could come together in partnership to provide a seamless or a one stop shop which meets the needs of service users. Needs over time could change in the same area that traditionally provide a specific service, partnerships may be formed to respond to these type of changes and flexibility. (Aldridge, N. 2005)
Models of Partnership
From time to time it will become necessary to evaluate the partnership relationship, there should always be a care and backup plan should something go wrong. An effective joint contribution can have positive impacts on service users and providers of services. These were some of the factors that were not implemented or ignored among many others at the Stafford hospital.
The Green paper, every child matters, was published by the government in 2003, with a view to safeguard and support young people in need of help and at risk. (Children Act 2004). Under section 18 of the children act 2004, the director of children services has the responsibility of ensuring that local authorities meet specific duties (Department of Education 2013). According to health and social care act 2008/12. Local authorities should work together in partnership with education , health and social care organization to support vulnerable service users by making sure health care workers are properly trained and valued, deal with core problems and intervene to protect children before a crisis situation gets out of control. (Susan Balloch, 2001)

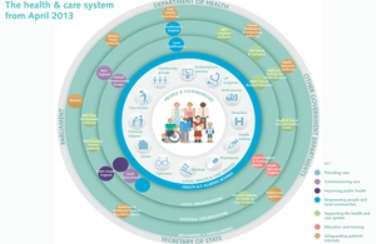
Figure 1 (Health & Social Care Partnership Model)
Figure 1 above shows a typical model of a partnership working across the health and social care.
The hybrid model among other models applicable that shows different partnership functioning in an organization, is likened to an umbrella for some models with organizations working tactically in combination with other models to achieve the best services. This was not the case at the Mid Staffordshire NHS Foundation Trust (Stafford hospital) according to the Francis report, where corporate self-interest and cost control were put ahead of patients and their safety, a lack of care, compassion, humanity and clear leadership. With the most basic standards of care not observed. The failure of collaborative working and an effective partnership model working effectively and efficiently across the Mid Staffordshire NHS Foundation Trust have identified a number of barriers to establishing effective professional partnership. (Babington and Charley, 1990).
There could be other barriers, for example health professionals not sharing the same goals, lack of communication, an organization feeling superior to the other for various reasons. (Scott Reeves, 2010)
Legislation for Partnerships
Legislation is, ‘’Law which has been enacted by parliament” or a governing body, and a Policy the statement of an agreed intent that sets out an organisations’ views with respect to a particular practice. Setting out principles and rules that provide the direction for an organisation to follow.
A Practice is the step-by-step method of implementation of the policy and responsibility.
The current and relevant legislation for organisation practice, policies and procedure affecting partnership working in health and social care include:
- Equality Act 2010,
- Care Standard Act 2000,
- Disability Discrimination Act 2005.
- Care Standards Act (2000) (England and Wales)
- Health and Safety at Work Act (1974), the act ensures that any working environment should be safe and free from hazards for both employers and employees.
- Human Rights Act (1998), empowers individuals if they feel unfairly treated can resort to court action.
- Manual Handling Regulations (1992), covers the safe moving and handling of equipment, loads and patients.
- Reporting of Injuries, Diseases and Dangerous Occurrences Regulations (1995) (RIDDOR)
In the scenario case of the Mid Staffordshire NHS foundation trust at the Stafford hospital in 2007, there was enough legislation in place at the time to have prevented the incidents and scandal that took place in at the hospital at the time. But working practices and policies were lacking, relaxed not in place or plainly ineffective or not in force or enforced. (Susan Balloch, 2001)
Effects of Negative Working Partnerships
Hospital management and staff, nurses etc, mental health and GPs, social services care and service users, and so on, all within the health and social care sector. The differences in working practices across the health and social care sector cannot be more pronounced in the negative impact it can bring more than what has been seen and the numerous scandals and mistakes that happened at the Stafford hospital Mid Staffordshire NHS foundation trust, where patients were left unattended, patients drinking from flower vases. There was no collaborative working practices in place, where the planning process should involve a number of practices and practitioners working together (cited in the oxford university press 1996 pg. 317). Professionals and organizations should be working together, for example
- GPs (general practitioners) first point of call for patients health problems,
- Support workers, bringing some form of independence to vulnerable service users by helping and support of vulnerable service users and recommending available services.
A disjointed service sector with different working practices not harmonised can not only be very ineffective, wasteful and more expensive but can also end up to be dangerous to service users, in the absence of any form of follow up and or expertise which may well be available but not accessed or utilised.
The Team Ro les that Meredith Belbin identified are widely used in organisations. They are used to identify people’s behavioural strengths and weaknesses in the workplace. This information can be used to:
- Build productive working relationships
- Select and develop high-performing teams
- Raise self-awareness and personal effectiveness
- Build mutual trust and understanding
- Aid recruitment processes
(Evans, D. & Killoran, A. 2000)
Case Study
When most a times outcomes of partnerships are scrutinized or looked at it often almost involve a tragic case, in this report I have been looking at the tragic case of a patient which I refer to as patient A. which prompted a case review in Greater Manchester. A Multi-disciplinary and multi-organisational partnership with good communication and relationships with organizations and people from different disciplines will enlarge the efficiency and size of the service team to service users which allows for a holistic approach and responsiveness to service delivery, better value for money with reduced duplication of services.
Looking again at our case scenario of patient A, (a 64 year old male) who was not mentally and physically able to defend himself, and made few demands on the health and social care services for support and did not have much support considering his condition to exercise control over his own life, the outcome of these failure in partnership was that patient A was not empowered to make choices and neither were the professionals supposed to be on the lookout for vulnerable people empowered with responsibilities or resources to make necessary changes, and neither the health professionals get to understand the issues or get involved fully and should be accountable for lack of action. There was no body or institution tasked to monitor situations adequately leading to no proper assessment of the situation even by psychological professional services, these outcomes can also be attributed lack of proper information gathering and sharing which led to exclusion of necessary and important participants, contributors and help to give patient A that was readily available due to lack of a clear leadership, clarity of role and a unified information and management system. For positive outcomes in partnerships and to provide person centred care it is essential that communication between interagencies, individuals, key people, service user’s family and friends, G.P’s, nurses, opticians, dentists, Physiotherapists, O.Ts, psychologists etc. to be really effective. Any barriers to communication should be minimised to ensure good communications. There should be an opening of a subject to widespread discussion and debate to enable the communication of ideas to all those working together in the partnership, so that they can be used and lead to change. This should be an on-going activity which is used to inform changes to policies and procedures within the workplace and involves the sharing of good practice leading to reduced professional isolation. (Frances Sussex, 2008)
Barriers to Effective Partnerships
While working in partnership is significantly crucial and important in the health and social care sector, working in collaboration and partnership across various agencies can be a daunting task, as there need to be an understanding of respective duties, roles, and organizational structure of different professionals, agencies and their language, therefore this could frustrating and be a barrier that could lead to poor communication and misunderstanding, coupled with the fact of having to deal with different legislations, funding streams, professional complexes and organizational structures.
Where there is a perception of superiority differences in status between individuals or partners in a partnership, this creates a barrier for a proper partnership relationship. There could be ways in which the above stated barriers could be overcome.
- The sharing of objectives, goals and outcomes.
- Sharing information and the use of a standard and common terminology.
- Meetings not being too formal and joint team building activities.
- Having joint training and face to face working.
- A full commitment to the partnership relationship with a clear demarcation of roles.
(Hudson, B. 2002)
If we look at one of the above points for example having joint training and face to face working will create a closer relationship and understanding in partnership relationships by reducing formality, improving understanding among partners, and an opportunity to bring up any problems or issues that may require resolving.
Recommmendations
Having looked at the issues relating to patient A, published in the Guardian newspaper of Friday 12 March 2010 a Serious Case Review such as that of Adult A gives an invaluable lesson to be learnt in what can be done to prevent such incidents and tragedies. A range of strategies need to be considered to improve outcomes and partnership working. Professionals working in different health and social care services have a shared responsibility to know what their role is individually within any partnership, with measures to be taken jointly or individually to protect vulnerable people from preventable harm.
Before dwelling on inter-agency co-operation and participation, it is important to consider the promotion, participation and empowerment of the service user. The effectiveness of interagency collaboration and information sharing can be diminished and less productive if the service user does not feel part of the process and the chances of a successful outcome will be significantly reduced. Hence it will be produce a better outcome to work in partnership with carers, families, advocates and other people who are sometimes called “significant others”. In order to work well in partnership, there has to be good communication and you will need to have good communication skills.
Some suggested strategies for an improved and positive outcome for an effective and productive partnership in the health and social services are to:
- Analyse the importance of working in partnership with others.
- Develop procedures for effective working relationships with others.
- Agree common objectives when working with others within the boundaries of own role and responsibilities.
- Evaluate procedures for working with others.
- Deal constructively with any conflict that may arise with others.
(Department of Health (DH) 2007)
Conclusion
In conclusion, having looked at the issues at the Stafford hospital coupled with the issue of patient A in Manchester, the factors that have impacted the hospitals could be looked at as down to lack of the full and proper training coupled with effective implementation of partnership with relevant bodies like the voluntary sector and families.
Most of the factors discussed above will have impacted on the provision of effective services to service users
References
Aldridge, N. (2005) Communities in Control: The New Third Sector Agenda for Public Sector Reform. Social Market Foundation.
Bulloch S. Taylor M. (2001). Partnership Working. Great Britain.
Evans, D. & Killoran, A. (2000) Tackling health inequalities through partnership working: learning from a realistic evaluation. Critical Public Health, 10, 125-140.
Martin V. e1 al. (2010). Managing in health and social care. Rouleledge. Oxon.
Cameron, A. and Lart, R. (2003) ‘Factors promoting and obstacles hindering joint working: a systematic review of the research evidence’, Journal of Integrated Care, vol 11, no 2, pp 9-17.
Dowling, B., Powell, M. and Glendinning, C. (2004) ‘Conceptualising successful partnerships’, Health & S9cial Care in the Community, vol 14, no 4, pp 309-317.
Department of Health (DH) (2007) Putting people first: a shared vision and commitment to the transformation of adult social care, London: DH.
Hudson, B. (2002) lnterprofessionality in health and social care: the Achilles’ heel of partnership? Journal of lnterprofessional Care, 16, 7-17.
Huxham, C. & Vangen, S. (2005) Managing to Collaborate: The Theory and Practice of Collaborative Advantage. Routledge.
Larkin, C. & Callaghan, P. (2005) Professionals ‘ perceptions of inter.professional working in community mental health teams. Journal of Interprofessional Care, 19, 338- 346.
Vaughan, B. and Lathlean, J. (1999) Intermediate care models in practice, London: The King’s Fund.
Btcc national can:. Mark Walsh. (2003).
Duncan. M .. Heighway. P. and Chaddcr. P.201 0 . II calth and safety al work essential. 6th ed.London: la pack publishing Ltd.
Health and social care. Bleenationa J level 3. Caroly AJdworth (2010).
Health and social care Btech level 3. Beryl stretch and Mary Whitehouse (2010).
lnlemational health and social care. Neil Moonic and Gou~11cth Windsor (200).
Introduction to health and safe~ at work. Phil Hughes. Ed ferett (2011 .
Managing in health and social care. Vivien martin. Julie Charlesworth. Euan Henderson (2010).
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on UKEssays.com then please click the following link to email our support team:
Request essay removal


