Cognitive Behavioural Therapy (CBT) in Low Self-Esteem (LSE)
| ✅ Paper Type: Free Essay | ✅ Subject: Psychology |
| ✅ Wordcount: 3868 words | ✅ Published: 11 Sep 2017 |
This case study focuses on a CBT intervention for a client presenting with Low Self-Esteem (LSE) issues and anxiety. The case study will particularly focus on low self-esteem as this was the main issue for the client. Its aims are: to build on existing experience and knowledge; to have a greater understanding of CBT and its application to anxiety disorder and LSE; and how to formulate, implement and monitor CBT as part of a treatment plan. The first part of the case study will outline the background of the client, and this will lead on to the presenting problem. The second part will briefly describe formulation models and processes, which leads to the third part, discussing the course of therapy. Finally, there will be a reflective analysis of the case study.
2.Introduction to Client
MM is the client’s pseudonym, which will be used throughout this study to maintain confidentiality. Both verbal and signed consent was obtained, as per course protocols and the professional code of conduct requirement (British Association for Behavioural & Cognitive Psychotherapies, 2016), permitting her clinical information be used. MM is a 26-year-old female client, who works full time as a communication officer mainly dealing with press. She is single and currently lives with her mother, brother, and stepfather. Prior to this she lived mainly with her father, with whom she had a good relationship. She reports her mother always being over -critical about everything she does. She appears well educated and articulate and presented as smartly dressed. She reports having experienced symptoms of anxiety from age fourteen, since her parents’ divorce.
MM recognised that she was experiencing LSE, which was interfering with her work and social life and in turn increasing her anxiety levels, so she referred herself to local charitable organisation who directed her for CBT therapy.
2.1 Client Presenting Problems
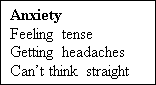
MM presented an increase in anxiety, low mood and low self-esteem. She reported that she has always been an anxious person, but her symptoms were triggered three years ago, following the death of her father, to whom she was very close. She described symptoms of feeling that she is not good enough, having low self-esteem, having the inability to say no to her grandfather, family, friends, and doubting herself, thus seeking reassurance. She defined herself as a “people pleaser, wanting to please everybody”. She reported feeling extremely anxious when on her own. Although she is more comfortable with her close friends, she has a low opinion of herself, feeling she is not as good as them and fearing that she may be evaluated negatively. These thoughts led to feelings of inadequacy and fear of being evaluated negatively by others.
Additionally, some of her anxiety manifests itself when she is alone, especially in her bedroom, and she experiences symptoms of increased heart rate, sweaty palms and an inability to relax. She also has personal conflict regarding her grandfather who needs support, but she feels that this compromises her social life. Her inability to say “no” to her grandfather and others increases her anxiety levels. After her father’s death, she did not wish to have bereavement counselling. At this time she split from her boyfriend. She described their relationship as not a happy one; she stated that he dominated their relationship and she was unable to assert herself. Since then, because of her anxieties, she has felt that she is not “good enough” to start another relationship, although she would like to. She had a brief course of CBT about two years ago and although she found it helpful in some aspect, she felt it did not address LSE.
MM has a diagnosis of anxiety and reported reduced concentration, poor memory and retention of information. She also feels irritable, her emotions fluctuate, and she feels inadequate and not good enough so seeks reassurance from family and others. has not reported physical health issues during this session. Sleep patterns are generally fine and appetite reported to be good. She is not on any prescribed medication. Her current method of coping skills prior to this therapy was trying to avoid any uncomfortable situations such as being in a large group of people, where she felt unable to express her opinion fearing others will disapprove her. The length of this course of therapy was agreed to be up to 12 sessions with a view to review at session six.
3. Formulation and its processes
Formulation is an evolving process bringing the theory and practice together step by step, thus selection of the appropriate model is essential to the successful treatment of the individual because they inform plan interventions (Kuyken, Padesky and Dudley, 2009). Consequently, formulation plays as a “powerful theoretical and therapeutic tool” (Kuyken, et. al. 2009). We formulated collaboratively a treatment plan in stages, starting from Level 1 and progressing into the deeper formulations (Level 1, 2-3) to understand the developmental and the interlinked maintenance cycle in MM’s presenting problem.
3.1- Level 1 Formulation
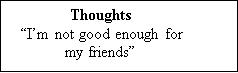
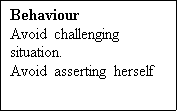
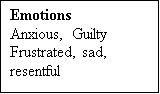
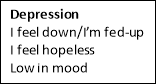
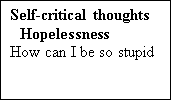
Following on from the initial assessment, all the information was collected and MM and her therapist worked collaboratively and completed the Level 1 formulation, using the Five Areas Model in the second session to help formulate treatment and intervention (see figure 1). The Five Areas Model was chosen as a first step because it encouraged MM to identify the link between situations, thoughts, feelings, behaviours, and physical sensations. This model not only enabled a structured session but also provided a range of techniques to help understand the current problems (Williams, 2003). The simplicity of this model also helped MM ease in to the therapy at the early stages (Padeysky and Mooney, 1990). The model and rationale for this was explained to MM by illustrating a diagram and discussing the key points. She responded well and took an active part in the discussion.
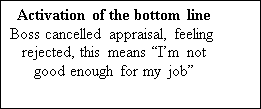
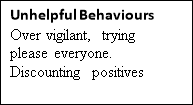
Following this MM recognised the link between the five areas and understand her cognitions as she expressed “I am not good enough for my friends, I will look stupid if I make wrong decisions.” It was easy to use this model as MM could see and relate to her maintenance cycle. However, it was not detailed enough to meet MM’s specific needs. Further formulation was needed for an individualised and effective treatment of LSE. From MM’s description of her symptoms the Cognitive Model of Low Self Esteem by Fennell (2009) was used as it fitted well. See figure 2.
Figure 1- Five Areas Model ( Williams, 2003).
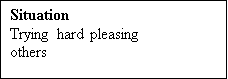 Level 1 Formulation
Level 1 Formulation




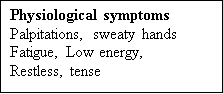
3.3 The Cognitive Model of Low Self-Esteem (Fennell, 2009).
This model was introduced in session four combining Level two and three formulations. This model stems from Beck’s (1979) Longitudinal Model of Depression, which was originally developed for depression and anxiety. It breaks it down in two sections: Developmental Factors being first part, leading to the Maintenance Cycle as the second part. Fennell (1998) suggests that LSE is linked to a wide range of presenting problems and promotes the use of this model in treating LSE. Based on MM descriptions of her symptoms this model seems to fit well. We collaboratively used this model to formulate and MM reflected on how her early experiences influence the maintenance cycle that perpetuates her present problem.
Figure 2. Cognitive Model of Low Self Esteem (Fennell, 2009)
Early Experience
Father “always nurturing and reassuring”
Mother “always critical, blaming me”
“Parents divorced”
The Bottom Line (Core Beliefs)
“I’m inadequate, useless, not good enough for my friends”
“I’m not good enough for anyone”
“I’m not good enough for my mom”
Rules for Leaving (conditional assumptions)
“If I don’t please others they won’t like me and I will be rejected”
“I will look stupid if I say the wrong things”
Trigger Situation (critical incidents)
“Father passed away”
“Returning to live with her mother”
“Mother is critical over whatever I do”





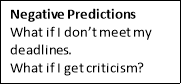




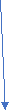


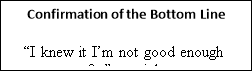
New Rules for Leaving
“I have tested this out and my predictions were wrong”
“The results did not match my prediction ideas”
Table 1- content of CBT sessions
|
Session |
Content |
Measures/ratings |
|
1 |
Initial assessment PHQ and GAD assessment |
PHQ =12 GAD=18 SUDS =3 |
|
2 |
Psychoeducation and rationale for CBT Treatment Formulation level 1 |
SUDS =4 |
|
3 |
Psychoeducation around Assertiveness and anxiety Smart goals Agreed |
SUDS-4 |
|
4 |
Cognitive Model of Low Self Esteem Level 2-3 formulation introduced cognitive re-structuring |
SUDS-5 |
|
5 |
Positive data log Smart Goals progress |
SUDS-6 |
|
6 |
Progress review |
PHQ 9 – 5 GAD 7 -5 SUDS-6 |
|
7 |
Designing behavioural experiment |
SUDS- 7 |
PHQ 9= Patient Health Questioners (see appendix F)
GAD 7=General Anxiety Disorder (see appendix F)
SUDS=Subjective Units of Distress/Disturbance Scale (see appendix D)
4.1 The Essential features of the process of therapy
Therapeutic relationship and good rapport was established and client trust was gained during this course of treatment, as this optimises the client engagement with therapy (Westbrook, Kennerly and Kirk, 2011). In addition, the therapist needs to be competent, and knowledgeable to be able to understand the client presenting problems, eliciting key cognitions and behaviour using guided discovery and helping them to relate formulation to intervention within the CBT treatment models. These essential features underpin a successful therapy process (Blackburn, et. al., 2000). MM engaged actively with the therapy and seemed keen to overcome her presenting difficulties.
The process of this therapy commenced with an initial assessment of her suitability for CBT, which is important so that an appropriate treatment plan can be formulated (Fennell 2009)
Formulation took place collaboratively by engaging MM actively in the session.
It is essential that there is a tailored individualised treatment plan which the client is encouraged to be involved with. As part of the treatment plan smart goals were agreed and interventions were implemented. Feedback from MM was that she is learning skills to help outside of therapy and found the collaboration very empowering and felt reduction in her anxiety levels.
Session 1
The initial assessment and risk assessment showed that MM was low risk and indicated her suitability for CBT. She scored 12 on PHQ 9, suggesting moderate depression; 18 on GAD 7, indicating high levels of anxiety; and 3 on SUDS, suggesting low mood (Wolpe, 1969). Professional boundaries were explained, including confidentiality.
Session 2
In this session, Level 1 formulation was completed collaboratively (see Figure 1). Psychoeducation was delivered, normalising anxiety and validating the client’s feelings, whilst also explaining the process of CBT treatment and its rationale (Kuyken, Padeysky and Dudley, 2009).
Once we had completed the Five Areas Formulation, I educated MM on anxiety and the maintenance cycle. During this process, MM identified key cognitions such as inability to say “no” to others and “I’m not good enough” one of the attributing factors in increasing her anxiety levels, and the impact had on her self-esteem. SMART Goals were discussed and MM wished to work on her assertiveness as a priority, with LSE being second. By the end of this session MM seem to have developed good insight into her maintenance cycle of anxiety, and set the following goal to achieve: “To have reduction in anxiety symptoms, to have confidence and believe in myself”. In order to decrease her anxiety symptoms, it was agreed to work on assertiveness, to enable her to increase her confidence and enhance her self-efficacy.
Session 3
In her list MM prioritised tackling assertiveness to enable her to say “no” comfortably to others, including her grandfather because of his expectation that she would help him with his shopping at weekends. This impacted on her as she felt she had no time for herself at weekends, which led to an increase in frustration, depression, and anxiety. She recognised this is an issue and wanted to be able to “reassure herself that it is okay to say “no” in some circumstances” and to build her confidence around this. MM agreed to practice assertiveness skills during this session and experiment with it outside the sessions. Homework for in between sessions was agreed and designed collaboratively; for her to start practising saying “no”. The aim of the homework was to provide an opportunity to master what was learned outside of therapy sessions (Westbrook et al, 2014).
Session 4 and 5-
We focussed on the Cognitive Model of the Low Self-Esteem (Fennel, 2006) its application and principles. MM reflected and realised that she had been self-doubting and discounting her achievements. We discussed and developed useful strategies to find alternatives to combat unhelpful thoughts, and MM agreed to complete a positive data log as homework (Wells, 2003). (see Apendices 1,2,3).
Session 6
We reviewed progress. MM scored 5 on PHQ 9, 5 on GAD 7 and 6 on SUDs, indicating overall significant improvement from the first session. MM reported feeling more comfortable with saying ‘no’ to others and her grandfather. She recognised this is an active process, and the more she rehearses the process the more effective it becomes. We reviewed homework and MM found observing unhelpful thoughts and replacing them with positive ones by logging them “very helpful”, thus allowing her to see and have a balanced view about herself. MM commented that this activity had helped increase her self-esteem and confidence. Subsequently she felt her anxiety reduced in comparison to the first session. She also learned that normalising and accepting anxiety made it easier to work with, as opposed to fighting it. Measuring her mood, she scored 7 on SUDs.
Session 7
MM wished to take an experimental approach to see if she could tolerate being alone in her bedroom, and if so for how long, as this had previously been an issue. We discussed graded exposure, and MM was willing for us to plan this together and carry out this task as homework. This to be repeated in the next session.
4.2-Future planned session
8- Behavioural Experiments (BE’s)
9- Repeat BE’s
10-Recup on previous sessions and learning
11– Introduce relapse management
12-Complete relapse management
MM was my first client and I am still building my confidence, skills and knowledge and will continue to develop and grow. I have discussed the case regularly in group supervisions and was beneficial. As an experienced community psychiatric nurse, I felt comfortable with the interpersonal process involved in therapy.
Although diagnosis is important, I have learned that dealing with presenting problems is primary concern in therapy. On reflection, although MM has a diagnosis of anxiety and presented with high level of symptoms she identified her current difficulties to be a lack of assertiveness, confidence and low self-esteem and wished to work on these difficulties first. Low Self Esteem was impacting on her anxiety levels and her mood. While LSE is not a diagnosis it was impacting negatively on MM’s work and social life and she wanted to overcome this. When working with MM I became more aware that LSE symptoms overlap with other diagnoses such as anxiety, depression and many other psychological problems thus illustrating the term of diagnosis is broad. Therefore, the therapist must assess carefully, eliciting appropriate emotional, behavioural and key cognitions as they are essential to formulate appropriate CBT treatment plans, without which the clients problem may not be recognised.
The outcome of the measurement indicated improvement by the end of session seven suggesting that the therapy was successful at this stage. The potential reasons for the improvement are the positive therapeutic relationship, collaboration, and MM’s engagement.
One of the challenges was maintaining the regularity of the sessions due to MM’s work commitment.
In hindsight, it would have been more beneficial for session to be weekly basis to allow continuity of therapy. Also, perhaps up to 15 sessions rather than the settings allow.
British Association for Behavioural & Cognitive Psychotherapies, (2016). Accessed on line; www.babcp.com
Beck, A.T., Rush, J.A, Shaw, B.F., and Emery, G. (1979) Cognitive Therapy of Depression. Guildford Press, New York.
Blackburn, I.M., James, I.A., Milne, D.L, and Reichelt, F.K (2000) Cognitive Therapy Scale- Revised (CTS-R). New Castle Upon Tyne, UK.
Fennell, M., (1998) Cognitive Therapy in the Treatment of Low Self-Esteem. Advances in psychiatric Treatment. Vol.,4, pp. 296-304.
Fennell, M. (2009) Overcoming Low self-esteem. A self-help guide using cognitive behavioural therapy techniques.
Kuyken, W., Padesky, A.C., and Dudley, R. (2009) Collaborative Case Conceptualization. Working Effectively with Clients in Cognitive – Behavioural Therapy. Guilford Press, London.
Padesky, A.C., and Mooney, A.K. (1990) Clinical Tip: Presenting the Model to Clients.
6:13-14. Accessed on line, www.padesky.com
Wells, A., (2003) Cogntive Therapy of Anxiety Disorders. A Practice Manual and Conceptual Guide. New York, Willey & Sons.
Westbrook, D., Kennerley, H. and Kirk, J. (2011) An Introduction to Cognitive Behaviour Therapy. Skills and Applications. London, sage.
Williams, C. (2003) Overcoming Anxiety. A Five Areas Approach. London, Hodder Arnold.
Wolpe, J. (1969) The Practice of Behaviour Therapy. New York, Pergamon Press. Obtained from, www.phqscreeners.com
Appendix A-Positive Data Log 1
Old belief: I am not good enough for my friends
Rate how strongly you believe this: 90%
New belief: I am good enough for my friends
Rate how strongly you believe this: 40%
Evidence that supports your new belief and disconfirms your old belief:
– I am very supportive and generous
– They know I would do anything for them
– I am always there for them when they need me
– I am selfless when it comes to my friends
– I always listen and offer them advice
– I am proud of them and I tell them this
– They tell me they are proud of me
– They take an interest in my life
– They always keep in touch
– They were there to support me at the funeral when Dad died
– They have listened and have explained they have found it difficult to deal with
– They always tell me they love me
– They celebrate my successes with me
– They include me in conversations and always invite me to catch ups/nights out
Rate how strongly you believe the old belief: 60%
Rate how strongly you believe the new belief: 75%
Appendix B-Positive Data Log 2
Old belief: I am not good enough for anyone
Rate how strongly you believe this: 90%
New belief: I am good enough for anyone
Rate how strongly you believe this: 40%
Evidence that supports your new belief and disconfirms your old belief:
– I am a good person with a good heart and good intentions
– I am a selfless person which is a valuable quality to have
– I am a nice and friendly person
– I am an outgoing person who is there for anyone and everyone who need me
– I have a good job and I am a driven, ambitious individual
– I have faced very challenging moments in my life so far and I have remained strong throughout
– I am an optimistic, patient individual
– I am reliable and trustworthy
– I am often told that I am a likeable person
– I am often told I should be proud of all I have achieved given all I have been through
– I am told I am a fun person to be around
– I always try to help people see the positives in life
Rate how strongly you believe the old belief: 40%
Rate how strongly you believe the new belief: 85%
Appendix C- PHQ 9 and GADS 7
Appendix D- Subjective Units of Distress Scale (SUDS)
Here is one version of the scale:
10 = Feels unbearably bad, beside yourself, out of control as in a nervous breakdown, overwhelmed, at the end of your rope. You may feel so upset that you don’t want to talk because you can’t imagine how anyone could possibly understand your agitation.
9 = Feeling desperate. What most people call a 10 is actually a 9. Feeling extremely freaked out to the point that it almost feels unbearable and you are getting scared of what you might do. Feeling very, very bad, losing control of your emotions.
8 = Freaking out. The beginning of alienation.
7 = Starting to freak out, on the edge of some definitely bad feelings. You can maintain control with difficulty.
6 = Feeling bad to the point that you begin to think something ought to be done about the way you feel.
5 = Moderately upset, uncomfortable. Unpleasant feelings are still manageable with some effort.
4 = Somewhat upset to the point that you cannot easily ignore an unpleasant thought. You can handle it OK but don’t feel good.
3 = Mildly upset. Worried, bothered to the point that you notice it.
2 = A little bit upset, but not noticeable unless you took care to pay attention to your feelings and then realize, “yes” there is something bothering me.
1 = No acute distress and feeling basically good. If you took special effort you might feel something unpleasant but not much.
0 = Peace, serenity, total relief. No more anxiety of any kind about any particular issue.
Appendix E- Relapse management
PSYCHOTROPIC MEDICATION
Use of psychotropic medication. (DEFINITION: Any medication capable of affecting the mind, emotions and behaviour. Please see list)
YesNo
WORK AND SOCIAL ADJUSTMENT
People’s problems sometimes affect their ability to do certain day-to-day tasks in their lives. To rate your problems look at each section and determine on the scale provided how much your problem impairs your ability to carry out the activity.
1. WORK – If you are retired or choose not to have a job for reasons unrelated to your problem, please tick NA/ (not applicable)
012345678N/A
Not at allSlightlyDefinitelyMarkedlyVery severely
I cannot work•
2. HOME MANAGEMENT – Cleaning, tidying, shopping, cooking, looking after home/ children, paying
bills etc
012345678
Not at allSlightlyDefinitelyMarkedlyVery severely
3. SOCIAL LEISURE ACTIVITIES – With other people, e.g. parties, pubs, outings, entertaining etc.
012345678
Not at allSlightlyDefinitelyMarkedlyVery severely
4. PRIVATE LEISURE ACTIVITIES – Done alone, e.g. reading, gardening, sewing, hobbies, walking
etc.
012345678
Not at allSlightlyDefinitelyMarkedlyVery severely
5. FAMILY AND RELATIONSHIPS – Form and maintain close relationships with others including the people that I live with
012345678
Not at allSlightlyDefinitelyMarkedlyVery severely
A12 – W6SAS total
G A D – 7
Over the last 2 weeks, how often have you been bothered by any of the following problems?
Not at allSeveral daysMorethan half the daysNearly everyDay
1Feeling nervous, anxious or on edge 0123
2NOT being able to stop or control worrying 0123
3Worrying too much about different things 0123
4Trouble relaxing 0123
5Being so restless that it is hard to sit still 0123
6Becoming easily annoyed or irritable 0123
7Feeling afraid as if something awful might happen 0123
A12 – GAD7 total score
PHQ-9
Over the last 2 weeks, how often have you been bothered by any of the following problems?
Not at allSeveral daysMore than half the daysNearly everyDay
1Little interest or pleasure in doing things 0123
2Feeling down, depressed or hopeless 0123
3Trouble falling or staying asleep, or sleeping too much 0123
4Feeling tired or having little energy 0123
5Poor appetite or overeating 0123
6Feeling bad about yourself – or that you are a failure or have let yourself or your family down 0 1 2 3
7Trouble concentrating on things, such as reading the newspaper or watching television 0 1 2 3
8Moving or speaking so slowly that other people could have noticed?
Or the opposite – being so fidgety or restless that you have been moving around a lot more than usual 0 1 2 3
9Thoughts that you would be better off dead or of hurting yourself in some way 01 2 3
A11 – PHQ9 total score
IAPT Phobia Scales
Choose a number from the scale below to show how much you would avoid each of the situations or objects listed below. Then write the number in the box opposite the situation.
012345678
Would not avoid it Slightly avoid it Definitely avoid it Markedly avoid itAlways avoid it
A17Social situations due to a fear of being embarrassed or making a fool of myself
A18Certain situations because of a fear of having a panic attack or other distressing symptoms (such as loss of bladder control, vomiting or dizziness)
A19Certain situations because of a fear of particular objects or activities (such as animals, heights, seeing blood, being in confined spaces, driving or flying).
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on UKEssays.com then please click the following link to email our support team:
Request essay removal


