Development of Iodine-131-Therapies
| ✅ Paper Type: Free Essay | ✅ Subject: Chemistry |
| ✅ Wordcount: 1870 words | ✅ Published: 23 Sep 2019 |
Figure Source NTP Radioisotope SOC Ltd
Iodine-131-Therapies
Report on MEDICAL TECHNOLOGY
Contents
The Underlying Physical Principles Iodine-131
Introduction
Cancer has been treated with radiopharmaceuticals since the 1940s. The radionuclides initially utilised, including Iodine-131 and P-32, are still being used. The job of the physicist in radionuclide treatment includes radiation insurance, imaging and dosimetry.
Radionuclide treatment is a fast growing malignancy treatment methodology, both regarding the number and scope of methodology given, and some new radiopharmaceuticals are currently entering the market. At present, there is a lack of rules overseeing the level of activity to administered according to local regulations. These have exhibited that a wide scope of assimilated portions is conveyed both to target tissues and to ordinary tissues from the administration of fixed activities of settled exercises because of varieties in uptake and retention of a radiopharmaceutical. It is likely that, related to patient variation in radiosensitivity, this records for the variable reaction seen with radionuclide treatment. (G. FLUX1, YONG DU, 19-1.1, P-641)
Malignant condition such as Differentiated thyroid cancer (DTS) treated by large Iodine-131. Iodine-131 is important isotope of Iodine, beta-emitting radionuclide with half physical life of 8.02 days. Iodine-131 therapy in the benign thyroid conditioned means oral or intravenous administration of Iodine-131 as sodium iodide (Radiopharmaceutical: Ns 131I). Iodine-131 is approved in the EU for the treatment of benign thyroid disease. (Dal Maso, Bosetti, Vecchia,Franceschi – 2009;20(1):75–86)
History of Development
The utilisation of Iodin-131 has proceeded as a mainstay of treatment for thyroid malignant growth today. The developing attention to significant short and long term outcomes of Iodin-131 treatment and its insufficiency in cutting edge metastatic thyroid carcinoma have prompted an increasingly wary and preservationist way to deal with its utilisation. This report is expected to feature the regions in which Iodin-131 treatment has had its most noteworthy accomplishments just as those clinical circumstances in which its utilisation is not upheld by clinical experience.
Radioiodine treatment of well differentiated thyroid disease includes the adminisshort- and long-termmme amounts of the radionuclide expected to crush the malignant growth. Thus, radiation incited variation from the norm may show and henceforth, radioiodine treatment ought to be given after cautious thought and when there is a sensible expectation that it will benefit the patient. Iodine 131 treatment for thyroid disease has as often as possible been divided into radioiodine ‘ablation’ and radioiodine ‘treatment’. (SWEENY, JOHNSTON – 24 (1995) 803-839)
The term ‘ablation’ shows of radioiodine to obliterate the typical staying thyroid tissue which is abandoned either unintentionally or purposely by the specialist trying to keep any harm to the parathyroid organs.
The term radioiodine ‘treatment’ is frequently used to demonstrate treatment given to leftover thyroid malignancy in the thyroid bed just as the treatment of repetitive infection in the thyroid bed and working metastases. (BALDET, MANDERSCHEID, GLINOER, JAFFIOL, COSTE SEIGNOVERT, PERCHERON, 120 (1989) 547-558)
The Underlying Physical Principles Iodine-131
Iodine (chemical symbol I) is a chemical component. There are 37 known isotopes of iodine, and just a single is not radioactive (Iodine-127). Most radioactive types of iodine are delivered as a side-effect of a splitting response from either atomic weapons testing or atomic power plants. A few types of radioactive iodine are made for use in prescription. Iodine-129 and I-131 are the most ordinarily utilised radioisotopes and will have the effects on the earth whenever discharged.
In radionuclide treatment, as opposed to analytic applications, the discharge of high vitality β radiation is required. Most radionuclides for radiotherapy are generated in nuclear reactor, Iodine-131 in this way, reactor created.
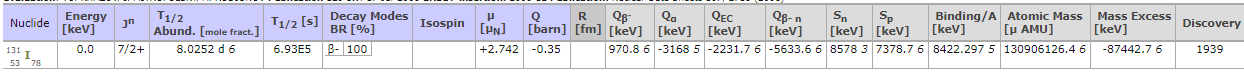
Source: IAEA – Nuclear Data Section
Iodine is a basic element of thyroid hormones LT4 (tetraiodothyronine, T4) and L-Triiodothyronine (T3). Thyroid cells concentrate and extract iodide from plasma. Not long after administrating, radioiodine is taken up from the blood by means of the sodium iodine symporter and gathers inside thyroid follicular cells. About 20% of the coursing iodide is expelled at every entry through the organ. Ingested iodine is assimilated through the small digestive tract and transported in the plasma to the thyroid, where it is concentrated, oxidised, and afterward consolidated into thyroglobulin (Tg) and later T4 and T3. After capacity in thyroid follicles, Tg is exposed to proteolysis and the discharged hormones are discharged into the course. In subjects with typical thyroid capacity up to 20– 30% of orally controlled iodine is taken up by the thyroid. In hyperthyroid patients this division is expanded – in extraordinary cases even up to over 90%. I-131 utilised for the treatment of thyroid issue rots to stable 131Xe by beta outflow.
The physical attributes of I-131 are as per the following:
T1/2 phys= 8.02 days;
β max − = 0.807 MeV;
β avg − =0.192 MeV;
gamma beam extends 80 to 723 keV,
most plentiful γ (82%) 364 keV.
The normal scope of the beta particles in delicate tissue is roughly 0.4 mm;
the most extreme range is around 3 mm. Radiobiological impacts of radioiodine on tissues are immediate (radiation store inside DNA) or circuitous. Backhanded impacts produce free radicals that thus respond with basic macromolecules.
Iodine-131 is specially regulated orally, yet in patients with serious gulping challenges, it very well may be regulated in fluid structure or intravenously in patients in whom retching is an issue. The fluid structure has the focal points over cases that it is more affordable, and it can be put away and effectively administered as required, yet the danger of ruining and defilement is higher. In numerous nations the treatment is performed in an outpatient setting. Care ought to be taken in patients who are incontinent of pee; an inhabiting catheter is suggested before radioiodine organisation to permit safe transfer of pee containing radioiodine. The prerequisite to concede patients due to managed I-131 action fluctuates significantly crosswise over Europe. Patients ought to be empowered to drink a substantial volume of liquid for a 24-h period following radioiodine treatment to bring down the radiation portion to the bladder. The confinements on work and contact with little youngsters rely upon national portion limits. For the most part in Europe, the presentation ought not surpass 1 mSv for other people in the all-inclusive community, which is a combined esteem every year. Generally, the patient is encouraged to keep as much separation as conceivable among themselves as well as other people, counting kids, and to keep contact times as short as possible0.
Clinical Uses
Oral administration of I-131 has been utilised to treat benign states of the thyroid organ since the 1940s
Patients with hyperthyroidism, which is a result of extreme thyroid hormone activity. The reasons for hyperthyroidism incorporate the accompanying:
(1) immune system hyperthyroidism called beforehand toxic diffuse goiter (Graves’ infection);
(2) lone hyperfunctioning thyroid knob;
(3) poisonous multinodular goiter (Plummer’s infection);
(4) quiet thyroiditis; and
(5) subacute thyroiditis
The initial three substances establish an unmistakable sign for Iodine-131 treatment, while quiet thyroiditis furthermore, subacute thyroiditis is never treated with Iodine-131. There is an emerging role for I- 131 in the treatment of purported subclinical hyperthyroidism brought about by any of initial three substances.
Patients with a large nontoxic goiter (NTG). This group incorporates patients who are euthyroid however who may advantage from a decrease in thyroid volume with Iodine-131 treatment.
Iodine-131 is by and large the main line treatment for single hyperfunctioning thyroid nodules, or it very well may be directed if hyperthyroidism isn’t controlled or repeats after beginning antithyroid medication treatment, for example, in Grave disease. The principle signs for radioiodine treatment of NTG are to diminish the measure of a goiter that is causing corrective challenges for the patient and to diminish compressive signs or side effects. The accessible treatment alternatives in NTG patients in whom the danger of harm is considered low are a “sit back and watch” approach, medical procedure, levothyroxine (LT4) at a portion to keep the TSH levels at the lower end of the ordinary range, and radioiodine administered. In patients with postoperative goiter repeat radioiodine treatment is frequently viewed as the primary line treatment, and the doctor ought not hold up until the patient moves toward becoming symptomatic. With LT4 prescription a few patients may accomplish clinically significant (over half) nodules or goiter shrinkage; in any case, this happens just in 10– 20% of patients.
Drawback
Acute Patients with a huge goiter may see transient swelling of the goiter and dyspnoea. Thyroid swelling keeps going for around a week following treatment and a few uneasiness or dyspnoea might be related with it. Slight uneasiness of the salivary gland might be available, however in difference to thyroid malignant growth, lasting damage is exceptional.
There might be a transient ascent in free T4 and free T3 levels 7– 10 days following radioiodine treatment, and patients who have been ineffectively controlled before radioiodine treatment may experience of heart arrhythmias and heart failure. In a few patients a thyroid storm may create. This uncommon condition must be treated with intravenous infusion of ATDs, corticosteroids and β-blockers.
Hypothyroidism The principle reaction of radioiodine treatment is hypothyroidism. Its rate shifts and keeps on expanding after some time, with the goal that deep rooted follow up is basic. Pretreatment forecast is not conceivable utilising current factors; notwithstanding, the rate is higher in Graves illness than in harmful goiter and is uncommon in singular hyperfunctioning nodules. Late perpetual hypothyroidism hence happens at a prior time in the group of patients with transient hypothyroidism than in those without. LT4 prescription is required in all patients with lifted TSH after I-131 treatment, and furthermore in patients with subclinical hypothyroidism.
Contraindications
Absolute:
Pregnancy
Women who are pregnant should not receive Iodine-131 therapy. Pregnancy should be delayed at least 6 to 12 months after Iodine-131 treatment.
Breastfeeding
Breastfeeding should be stope at leaset 6 weeks before Iodine-131 therapy and should not to be resumed.
Relative:
Uncontrolled hyperthyroidism
Active thyroid orbitopathy (particularly in smokers)
Temporary side effect of of Iodine-131 therapies may include:
- Neck tenderness and swelling
- Sickness
- Swollen salivary organs
- Loss of taste or taste change
- Dry mouth/lacking salivary generation
- Dry eyes
References
- (Dal Maso L , Bosetti C, La Vecchia C, Franceschi S. Risk factors for thyroid cancer: an epidemiological review focused on nutritional factors. Cancer Causes Control 2009;20(1):75–86.)
- (SEIDLIN, S.M., MARRINELLI, L.D., OSHRY, E., Radioactive iodine therapy:Effect on functioning metastases of adenocarcinoma of thyroid, JAMA 132 (1946) 838-847.)
- (SWEENY, D.C., JOHNSTON, G.S., Radioiodine therapy for thyroid cancer, Endocrinol Metab Clin North Am 24 (1995) 803-839.)
- (BALDET, L., MANDERSCHEID, J.C., GLINOER, D., JAFFIOL, C., COSTE SEIGNOVERT, B., PERCHERON, C., The management of differentiated thyroid cancer in Europe in 1988, Results of an international survey, Acta Endocrinol (Copenhagen) 120 (1989) 547-558.)
- 0(Eur J Nucl Med Mol Imaging (2010) 37:2218–2228 DOI 10.1007/s00259-010-1536-8)
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on UKEssays.com then please click the following link to email our support team:
Request essay removal



