Glomeruli and Glomerular Filtration Rate (GFR)
| ✅ Paper Type: Free Essay | ✅ Subject: Biology |
| ✅ Wordcount: 1139 words | ✅ Published: 23 Sep 2019 |
The glomeruli are microscopic filters made of a network of capillaries that filter the blood plasma, which occurs in the renal corpuscle of the nephron in the kidneys (figure 1). Glomerular filtration rate (GFR) is defined by amount of blood filtered by the glomerulus into the Bowman’s capsule (ml/per unit of time), the resulting fluid is called the glomerular filtrate. GFR is influenced by the interaction of several important pressures (Khan Academy, 2019).
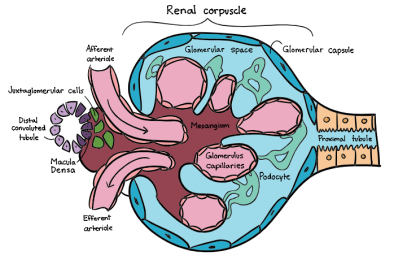
Figure 1 – Structure of the renal corpuscle filtering unit; glomeruli made up of a tuft of small blood capillaries contained with the Bowman’s capsule between the afferent and efferent arterioles. It is connected to the proximal tubule which leads to segments of the renal tubule such as Loop of Henle, the distal convoluted tubule and the collecting duct which leads to the urethra. (Khan Academy, 2019).
GFR is determined by the sum of the filtration rates of all the functioning nephrons in the kidneys. As a rough guide, a healthy GFR can be estimated by calculating 140 – [your age] i.e. a healthy 20-year old’s GFR would be 120ml/min. Body weight and height are also considered in the measurement. A GFR of less than 60ml/min can suggest chronic kidney disease (University of Washington, 2019).
GFR can be measured by quantifying the renal clearance of the endogenous substance of creatine, a by-product of muscle metabolism. It is freely filtered by the glomerulus so can be compared to the serum creatine concentration using the following equation:
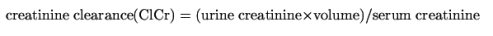
This however often overestimates GFR due to secretion of creatine by tubules (15%). Instead, an endogenous substance such as inulin (a carbohydrate that is purely filtered by the kidneys as it is neither reabsorbed or secreted) can be used to provide a more accurate measure of GFR. (Traynor, J).
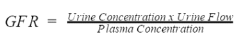
Figure 2 – Equation used to calculate GFR concentration; whereby the urine concentration refers to the concentration of inulin in the sample, the urine flow refers to the volume of urine produced in a given period and the plasma concentration is the concentration of inulin in the blood (Khan academy, 2019).
However, inulin is expensive, must be given by intravenous injection and measurements from blood and urine samples must be taken frequently over several hours to obtain an accurate measure of kidney function and filtration (Traynor, J).
The glomerulus is positioned between the afferent arteriole which delivers blood (1-1.1L per minute) to the glomerulus and the efferent arteriole which carries blood away. The efferent arteriole is significantly thinner than the afferent arteriole (figure 3) which maintains a high glomerular capillary pressure required for filtration (University of Washington, 2019).
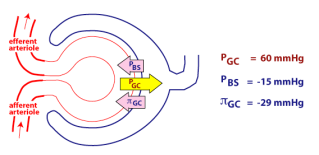




Figure 3 – Filtration rate is determined by three main pressures, one of which promotes filtration (PGC) and two that oppose filtration (πGC and PBS). The overall pressure in the capillaries (PGC) also known as hydrostatic pressure is very high due to the increased diameter of the afferent arteriole. Osmotic pressure (πGC) counteracts this force and occurs due to the higher concentration plasma proteins (e.g. albumin) in the capillaries that cannot be filtered causing water to move back into the capillaries. Together are known as Starling’s forces. Hydrostatic pressure is greater than osmotic pressure, to allow glomerular filtration to occur. The overall net glomerular filtration pressure (NFP) is the sum of PGC minus the hydrostatic pressure in the Bowman’s space (PBS) and the osmotic pressure from the blood proteins (πGC). NFP in this example is 60 – (15 + 29) = 16mmHg. (University of Washington, 2019)
GFR is directly proportional to the NFP. The hydrostatic pressure must be precisely regulated to maintain efficient filtration. High PGC can be maintained through an intrinsic process in the kidney called renal autoregulation (figure 4), regardless of natural changes in blood pressure (between 80 and 160mmHg) (University of Washington, 2019).
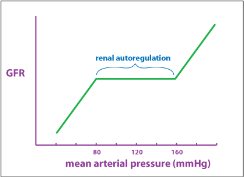
Figure 4 – An autoregulation graph describes the relationship between arterial pressure and GFR. The plateau shows the autoregulation range, which is the mean arterial pressures at which autoregulation remains effective. This is achieved through two primary mechanisms; myogenic reflux and juxtaglomerular apparatus. Beyond the plateau, there are upper and lower limits of GFR which are of clinical importance (University of Washington, 2019).
Myogenic reflux is a sympathetic response. Baroreceptors in the afferent arterioles detect an increase in blood pressure. This stimulates opening of calcium channels, causing action potential and contraction of the smooth muscle, resulting in vasoconstriction. The volume of blood entering the glomerular capillaries decreases, reducing PGC and reducing GFR. The opposite occurs when a decrease in blood pressure is detected, to increase GFR (University of Washington, 2019).
The juxtaglomerular apparatus (figure 5) activates the angiotensin-aldosterone system in response to a detecting a decrease in blood pressure.
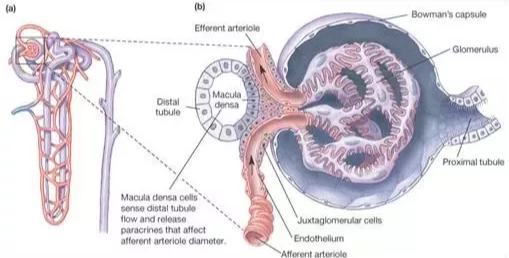
Figure 5 – Juxtaglomerular apparatus – juxtaglomerular cells line the afferent and efferent arterioles meet the macula densa cells in the distal convoluted tubule. The macula densa cells monitor the filtrate that it receives which was originally filtered in the Bowman’s capsule. Macula densa cells detect sodium composition of the filtrate (Histology, Yale. 2018).
In response to elevated sodium levels indicating low blood pressure, the macula densa cells stimulate juxtaglomerular cells to secrete the enzyme renin. This activates angiotensinogen (plasma protein in the blood) which is converted to angiotensin I. This is activated by ACE (angiotensin-converting enzyme) and converted to angiotensin II. This is a vasoconstrictor, causing constriction of the afferent arteriole, reducing blood flow and reducing GFR. Blood pressure is increased as it stimulates the thirst centre in the brain, increasing water retention. It also increases cardiac output by increasing stroke volume and heart rate (Histology, Yale. 2018).
ACE inhibitors are used to treat hypertension and lower blood pressure, by preventing the production of angiotensin II. This allows vasodilation of vessels, so they relax and widen, whilst also reducing water retention and blood volume (British Heart Foundation, 2019).
Conversely, the hormone atrial natriuretic peptide (ANP) can increase GFR. An increase in plasma volume activates secretion of the hormone from the heart which causes vasodilation of the afferent arteriole, an increase in sodium excretion (natriuresis) and increase in fluid excretion (diuresis) (University of Washington, 2019). They also decrease the release of renin, preventing the renin-angiotensin system (R, Klabunde. 2019).
References
- Khan Academy. (2019). Renal physiology: Glomerular filtration. [online] Available at: https://www.khanacademy.org/test-prep/mcat/organ-systems/the-renal-system/a/renal-physiology-glomerular-filtration [Accessed 4 Jan. 2019].
- University of Washington. (2019). Regulation of GFR. [online] Available at: https://courses.washington.edu/conj/bess/gfr/gfr.htm [Accessed 4 Jan. 2019].
- Traynor, J. (2006). How to measure renal function in clinical practice. BMJ, 333(7577).
- Histology, Yale (2019). Juxtaglomerular Apparatus. [online] Available at: http://medcell.med.yale.edu/histology/urinary_system_lab/juxtaglomerular_apparatus.php [Accessed 16 Feb. 2019].
- British Heart Foundation. (2019). Watch: What are ACE inhibitors and what do they do in your body?. [online] Available at: https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/drug-cabinet/ace-inhibitors [Accessed 16 Feb. 2019].
- Klabunde, R. (2019). CV Physiology | Atrial and Brain Natriuretic Peptides. [online] Cvphysiology.com. Available at: https://www.cvphysiology.com/Blood%20Pressure/BP017 [Accessed 16 Feb. 2019].
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on UKEssays.com then please click the following link to email our support team:
Request essay removal


