The Integumentary System in the Human Body
| ✅ Paper Type: Free Essay | ✅ Subject: Physiology |
| ✅ Wordcount: 3068 words | ✅ Published: 08 Feb 2020 |
The integumentary system is the body’s largest organ system. It comprises of the skin, hair, and exocrine glands. The integumentary system’s primary function is to protect the inner body from outside pathogens and harmful rays of light. It also helps to regulate body temperature and eliminate waste products from our bodies. While our skin seems simple from the outside, it is actually a complex network of different layers of cells. This research paper will talk about the integumentary system and its layers, how burn injuries are classified, and three dermatological diseases. The integumentary system has three distinct layers: the epidermis, dermis, and hypodermis.
The epidermis is the most superficial layer of the skin that we see every day. It covers the entirety of our bodies to close off our inner organs from the outside world. The epidermis is avascular, meaning it does not contain any blood or blood vessels. Instead, it receives nutrients via diffusion from the dermis. The epidermis also has its own distinct layers. There are two different types of skin: thick and thin. Thick skin has five layers, while thin skin has four layers. These layers are the stratum basale; the stratum spinosum; the stratum granulosum; the stratum lucidum; and the stratum corneum, as shown in Figure 1. 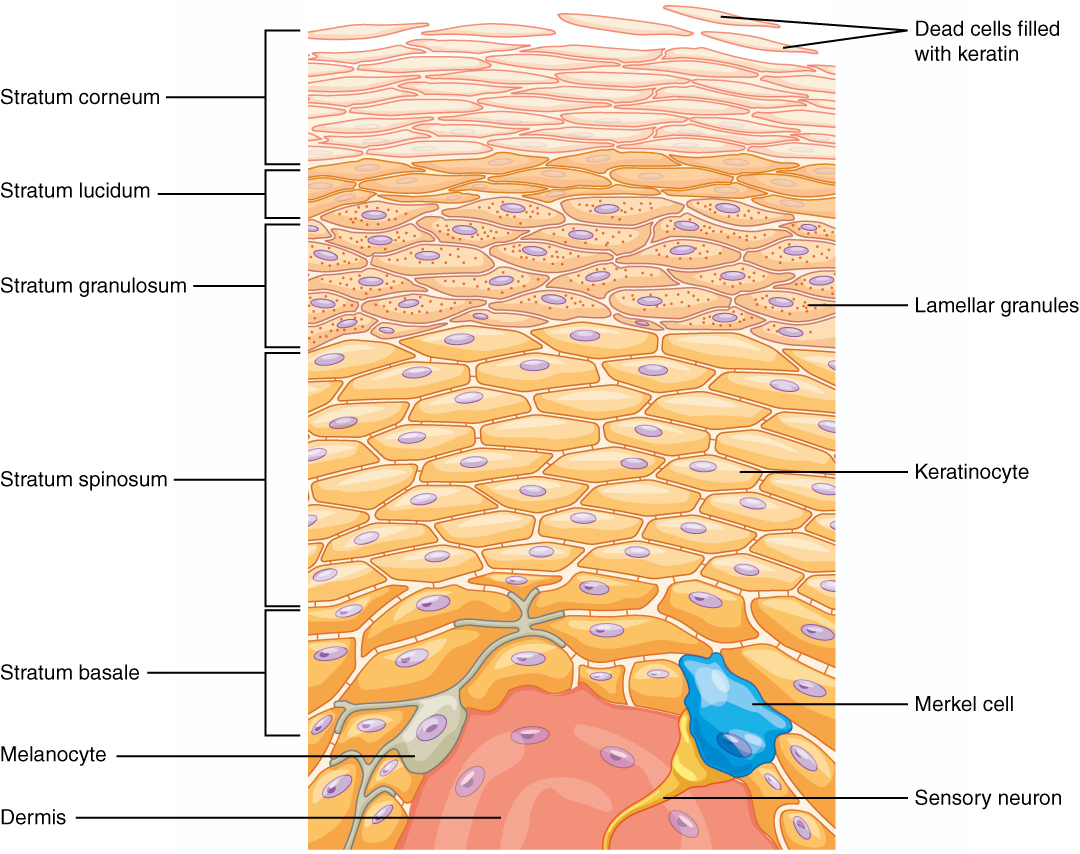
The stratum basale is the deepest layer of the epidermis, serving as the base for the other layers. It lies above the dermis. This layer is made up of cuboidal and columnar cells. There are three types of cells that make up this layer: keratinocytes, melanocytes, and Merkel cells.
Keratinocytes are the most abundant type of cells in the epidermis. They play a special role in that they make keratin, a protein that helps give the epidermis its strength. “Functions of keratin may include resistance to mechanical stress, influence over epithelial cell structure, and making the skin waterproof (3).” Keratinocytes are found in every stratum layer because as they undergo mitosis, a daughter cell is pushed up the stratum layers. However, as it goes up the layers, the keratinocyte begins to die. As seen in Figure 1, keratinocytes dominate most of the epidermal layers.
Melanocytes are the second most abundant type of cell in the basal layer. Their primary role is to produce a pigment called melanin, which give us our skin color. Melanin comes in a variety of colors, usually brown or yellow. The melanin helps protect the DNA found in the nucleus of the keratinocytes in the basal layer from ultraviolet lights. Melanocytes may produce these pigments, but they are not the cells that hold onto them. Instead, they transfer the melanin to keratinocyte have long branches protruding from them and extend to the keratinocytes. “The melanin is transferred via these branches in forms of melanosomes. Once transferred, the melanin enters the keratinocyte’s cytoplasm, encasing and shielding the nucleus (18).” Figure 2 shows the melanocytes’ branches extending to the keratinocytes. The melanin can also be seen surrounding the keratinocytes.
The third cell that occupies the stratum basale is the Merkel cell, also known as tactile cell. They aren’t as numerous as keratinocytes or melanocytes but play a significant role in our sense of touch. They are sensitive to compression; when they are stimulated, chemicals are released that provide our body with the sensory information of an object contacting the skin.
The second deepest layer of the epidermis is the stratum spinosum. In this layer, there are also keratinocytes present. These keratinocytes attach to their neighboring cells via desmosomes. As the keratinocytes prepare to be pushed up further to become part of the epidermal tissue, their cytoplasm begins to diminish.
The fourth type of cell is found in this layer. This cell is called the Langerhans cell, or the epidermal dendritic cell. These cells are important to our bodies as they are immune cells that are tasked with defending the epidermis from infections. “When they undergo phagocytosis, an immune response is activated. This response prepares the body to fight potential pathogens and cancer cells that may have breached the superficial layers of the epidermis (14).”
The third layer is the stratum granulosum. This is the layer in which keratinocytes begin to die, as their nucleus and cytoplasm disintegrate. Replacing their nucleus and cytoplasm is the previously mentioned protein, keratin. This process is referred to as keratinization. In this layer, a structure of keratinocytes begins to look more apparent than any other layer. This structure is known as the keratohyalin granule. “Their primary function is to help bind the keratin together in order to create an impenetrable barrier (7).” They also have glycolipids that contribute to the skin’s waterproof nature.
The fourth layer is the stratum lucidum. As mentioned before, this is only found in thick skin. These areas include the hands and feet, where most of the body’s abrasion occurs. The keratinocytes in this layer are flat and translucent. “In this layer, they are filled with the protein, eleidin. This is the product that results from transforming keratin (14).”
The most superficial layer of the epidermis is the stratum corneum. This is a layer that is made up of 20-30 layers of dead keratinocytes. These keratinocytes went through a process starting from the stratum basale. As they matured and advance up the layers of the epidermis, they bind to neighboring keratinocytes and lose their nucleus and cytoplasm. They are filled with keratin, essentially becoming an encasement of keratin. These dead keratinocytes remain as a barrier before shedding. Then the whole keratinocyte process begins again, starting from the stratum basale.
Under the epidermis is the dermis. This layer is made up of connective tissue and contains collagen, with some elastic and reticular fibers. The dermis serves as a placeholder for accessory structures of the integumentary system. These may include hair follicles, blood vessels, glands, and nail roots. The dermis has two of its own layers. These layers are the papillary layer and the reticular layer.
The papillary layer is the most superficial of the two layers. This layer is mostly composed of adipose connective tissue. In the papillary layer, there are projections from the dermis called dermal papillae, as seen in Figure 3. There are projections that go the opposite direction and piece together with the dermal papillae called epidermal ridges. These teeth-like projections create what we see as fingerprints. They act as tactile receptors, much like Merkel cells. They are able to detect any contact with the epidermis. “The dermal papillae each contain capillaries that are responsible for transporting nutrient and blood to the epidermis (14).” The papillary layer also serves as an anchoring site for the arrector pili muscle. This small muscle is what allows us to feel any feeling when our hair is stimulated.
The reticular layer of the dermis lies between the superficial papillary layer of the dermis and the deep hypodermis layer. This layer is made up of dense irregular connective tissue with collagen fibers going in all directions. In this layer is where we find hair follicles and glands. The sebaceous glands are responsible for secreting an oily substance called sebum. This lubricates the hair and skin. Another gland is the sweat gland. This gland releases sweat to help maintain homeostasis by regulating body temperature. Apocrine glands secrete pheromones around the areas of the groin and armpits.
The hypodermis, or the subcutaneous layer, is the deepest layer of the skin under the reticular layer of the dermis. While it may not necessarily be a part of the integumentary system, it has some functions to the skin. “This layer is mostly made of fatty tissue. Because of the fatty tissue, it serves as a cushion and a way to retain body heat. It also serves as an emergency energy source (14).” The hypodermis also serves as a place for collagen fibers of the reticular layer to intertwine and stabilize the skin. As Figure 4 shows, the hypodermis is also a place for large blood vessels and nerves.
As we live our lives, we are prone to dangers and harm to our bodies. As our lives revolve mostly around fire, burns are bound to happen in our lifetime. A burn is an injury in which our skin and adjacent tissues are destroyed. “The severity of the burn is classified based on how deep the injury is, the location of the injury, and the surface area of the injury (19).” Burn injuries may also be classified based on the patient’s age. There are three classifications of burns: first- degree, second-degree, and third-degree.
A first-degree burn, or a superficial burn, is the least severe of the three burns. The most common symptoms of a first-degree burn are redness in the area and pain. The area of damage is the epidermis. Figure 5 shows the comparison between a first-degree burn and a normal skin layer. As can be seen, there is minor damage to the epidermis. These burns typically heal in 3-5 days. Figure 6 shows a first-degree burn in the form of a sunburn. The burned area is red and inflamed, but otherwise, it is relatively fine.
A second-degree burn, or partial-thickness burn, is more severe. The most common symptoms of this kind of burn are redness or whiteness of skin and blisters. There are two types of partial-thickness burns: superficial partial-thickness burns and deep partial-thickness burns. “Superficial partial-thickness burns destroy the epidermis and about 1/3 of the papillary dermis of the dermis. Deep partial-thickness burns destroy the epidermis and the dermis (21).” As seen in Figure 5, the epidermis is completely destroyed, and the dermis also sustained damage. There are formations of blisters. The blisters are visible in Figure 7, as well as the redness in the area around the burn.
The worst of the three-burn types is the third-degree burn. This burn completely destroys the epidermis, dermis, and the hypodermis. “Symptoms of this kind of burn are brown, black, or white skin on the area of injury, leathery skin, and numbness (6).” This burn destroys the nerves of the skin, causing numbness. As Figure 5 shows, a third-degree burn injury completely eradicated the epidermis and dermis, as well as damaged the subcutaneous layer. Figure 8 shows a third-degree burn injury. There is blackness in some parts of the burned area, as well as exposed fat under the skin.
A way that the severity of a burn is assessed is based on the “Rule of Nines.” “This method helps when trying to figure out how much surface area of the body was destroyed. This is important to remember because by knowing how much of the body was burned, we can estimate the amount of fluid that needs to be replaced (14).” Most of the body is divided in multiples of 9%. The upper limbs and head each count for 9%, while the lower limbs and the trunk count for 18% each, as shown in Figure 9. However, an infant has different percentage on its body than an adult’s. An infant’s head and body accounts for 18%, the lower limbs are 14%, and the upper limb are 9%. Both groin regions are 1%.
Burns may harm our bodies, but there are also dermatological diseases that pose a threat and may cause damage to our skin. Some diseases serve as a mild disturbance in daily life, while others may be life-threatening. Some dermatological diseases include acne vulgaris, rubeola, and basal cell carcinoma.
Acne vulgaris, commonly know as acne, is a chronic disease in which the body’s sebaceous glands produce an excessive amount of sebum, or oil, and gets plugged with dead skin cells. This affects about 20% of teenagers aged 15-17. Acne usually happens when a child is in the stage of puberty. Acne usually appears on the face, forehead, shoulders, and the back. Common symptoms of acne include blackheads, pimples, and painful lumps. When dead skin cells and oil become trapped in the pores of the skin, it builds up. “When exposed to the air, it becomes darker in color. There may also be bacteria trapped in the follicles. These are called blackheads (1).” Pimples are also a common occurrence when someone has acne. Pimples are raised spots on the skin. They are usually a red spot with a white circle in the middle of it. This occurs due to build-up of bacteria in the hair follicle, inflaming it. Acne may also cause scarring, as seen in Figure 10. While the damage to the skin may be minor and non-life threatening, it damages many teenagers emotionally and mentally, as it has been linked to increased self-consciousness and depression.
Another skin disease is rubeola, or measles. Measles is a highly contagious disease caused by the measles virus. “Symptoms of this disease are skin rashes followed by fevers and severe coughs. They may also experience gastrointestinal issues (15).” The rashes on the skin start to appear about 3-5 days after the fever starts. It may start at the face and spread to the trunk and limbs. As Figure 11 shows, the rashes spread from the face and covers most of the back and neck. With measles may come other diseases, such as pneumonia or keratoconjunctivitis. Pneumonia affects the respiratory system and is a big contributor to high measles fatalities. Keratoconjunctivitis causes blindness in the patient.
There are several kinds of skin cancer with the most serious being life-threatening. The most common kind of skin cancer is basal cell carcinoma. A major cause of this cancer is the overexposure to ultraviolet lights. Like many other cancers, damage to the cell’s DNA causes a genetic mutation, in which the cell divides rapidly and destroys adjacent tissues. Figure 12 shows the mass of dividing basal cells, creating a mass in the epidermis and dermis layer. “There are mainly three types of basal cell carcinoma: nodular BCC, superficial BCC, and morpheaform BCC (13).” Nodular BCC lesions consist of nodules with a shiny, pearl quality. This lesion may become crusted and larger over time with minor bleeding. Nodular BCC usually affects the papillary and reticular dermis. Superficial BCC lesions appear scaly and pink or purple. This may also become crusty with borders of purple papules. This type of cancer affects the epidermis and no deeper than the papillary layer. Morpheaform BCC lesions appear pink or white and scar-like. This type of BCC is the most severe as it has the most potential for destruction of the skin. It may invade the reticular layer of the dermis, as well as the subcutaneous layer. While its fatality numbers are low, they still cause significant damage to the skin.
The integumentary system may seem simple when looking from the outside, as it seems like a simple layer of skin. However, when looked under a microscope, there is a complex network of cells and nerves that communicate to protect our bodies. Of course, while the cells’ primary role is to protect our bodies, we are still prone to diseases and injuries to our skin. the integumentary system plays a vital role in keeping our bodies in homeostasis, which in turn, allows us to live.


(Figure 1)(2) (Figure 2)(22)


(Figure 3)(5) (Figure 4)(20)
 (Figure 5)(9)
(Figure 5)(9)


(Figure 6)(8) (Figure 7)(12)
 (Figure 8)(4)
(Figure 8)(4)
 (Figure 9)(10)
(Figure 9)(10)
 (Figure 10)(11)
(Figure 10)(11)
 (Figure 11)(16)
(Figure 11)(16)
 (Figure 12)(17)
(Figure 12)(17)
Works Cited
- “Acne.” Mayo Clinic. Mayo Foundation for Medical Education and Research, 27 Dec. 2018. Web. https://www.mayoclinic.org/diseases-conditions/acne/symptoms-causes/syc- 20368047
- Biga, Lindsay M., Sierra Dawson, Amy Harwell, Robin Hopkins, Joel Kaufmann, Mike LeMaster, Philip Matern, Katie Morrison-Graham, Jon Runyeon, and Leeah Whittier. “Anatomy & Physiology.” 5.1 Layers of the Skin | Anatomy & Physiology. Open Oregon State, Oregon State University, n.d. Web. http://library.open.oregonstate.edu/aandp/chapter/5-1-layers-of-the-skin/.
- Bragulla, Hermann H, and Dominique G Homberger. “Structure and Functions of Keratin Proteins in Simple, Stratified, Keratinized and Cornified Epithelia.” Journal ofAnatomy. 214.4: 516-59. Web.
- “Complications of Burns – That Might Occur.” The Burn Cream. N.p., 23 Mar. 2018. Web. 10 May 2019. http://theburncream.com/complications-burns-occur/.
- Dindicaballes Follow. “Layers of Skin.” LinkedIn SlideShare. N.p., 06 July 2012. Web. 10 May 2019. Slide 22 https://www.slideshare.net/dindicaballes/layers-of-skin.
- Dingwall, J A. “A CLINICAL TEST FOR DIFFERENTIATING SECOND FROM THIRD DEGREE BURNS.” Annals of surgery vol. 118,3 (1943): 427-9.
- Freeman SC. “Histology, Keratohyalin Granules.” StatPearls (2019): StatPearls , 2019. Web.
- “Home Remedies for First-Degree Burns.” Healthy Food Place. N.p., n.d. Web. 10 May 2019. http://www.healthyfoodplace.com/home-remedies-first-degree-burns/.
- “How to Deal with a Burn.” STS First Aid. N.p., 04 Nov. 2016. Web. 10 May 2019. https://sts-firstaid.co.uk/how-to-deal-with-a-burn/.
- Jackson, Andy, Katie, Eugene, James, Eugene, Ruku, and Lee. “Home.” EMTResourcecom. N.p., 27 Apr. 2014. Web. 10 May 2019. http://www.emtresource.com/emergencies/burns/rule-of-nines/.
- Kenan12. “Acne-vulgaris.” Liberal Dictionary. Liberal Dictionary, 12 Nov. 2018. Web. 10 May 2019. http://www.liberaldictionary.com/acne-vulgaris-2/.
- Library, Dr P. Marazzi/science Photo. “Close Up: Second Degree Burn To Male Left Forearm by Dr P. Marazzi/science Photo Library.” Pixels. N.p., n.d. Web. 10 May 2019. https://pixels.com/featured/close-up-second-degree-burn-to-male-left-forearm-dr-p- marazziscience-photo-library.html.
- Marzuka, Alexander G, and Samuel E Book. “Basal Cell Carcinoma: Pathogenesis, Epidemiology, Clinical Features, Diagnosis, Histopathology, and Management.” Yale J Biol Med 88.2: 167-79. Web.
- McKinley, Michael P., Valerie Dean. O’Loughlin, and Theresa Stouter. Bidle. ”Integumentary System.” Anatomy & Physiology: An Integrative Approach. N.p.: McGraw-Hill Higher Education, 2012. 187. Print.
- Moss, William J. “Measles.” Lancet 390.10111 (2017): 2490-502. Web.
- Norvell, Kim. “‘It Was Terrible’: Iowan Remembers Having Measles during One of the State’s Worst Outbreaks.” Des Moines Register. The Des Moines Register, 26 Apr. 2018. Web. 10 May 2019. https://www.desmoinesregister.com/story/news/health/2018/04/25/measles-iowa- vaccine-outbreak/550720002/.
- Riley, Jan. “Is Basal Cell Carcinoma on Your Radar?” Online CPD/CE Portfolio for HealthProfessionals. N.p., 31 Jan. 2016. Web. 10 May 2019. https://www.ausmed.com/cpd/articles/basal-cell-carcinoma.
- Seiberg, Miri. “Keratinocyte–Melanocyte Interactions During Melanosome Transfer.” Pigment Cell Research, vol. 14, no. 4, Aug. 2001, p. 236. EBSCOhost, search.ebscohost.com/login.aspx?direct=true&db=a9h&AN=5808765&site=ehost-live.
- Serrano, Carmen, Rafael Boloix-Tortosa, Tomás Gómez-Cía, and Begoña Acha. “Features Identification for Automatic Burn Classification.” Burns 41.8 (2015): 1883-890. Web.
- Skin (Integumentary) System Information. N.p., n.d. Web. 10 May 2019. http://owh.adam.com/pages/guide/reftext/html/skin_sys_fin.html.
- Vaughn, Lindsay, and Nicole Beckel. “Severe burn injury, burn shock, and smoke inhalation injury in small animals. Part 1: burn classification and pathophysiology.” Journal ofVeterinary Emergency and Critical Care 22.2 (2012): 179-186.
- “Why EVERYONE Should Use a Tyrosinase Inhibitor.” GlyMed Plus. N.p., n.d. Web. 10 May 2019. http://www.glymedplus.com/blog/why-everyone-should-use-a-tyrosinase-inhibitor/.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on UKEssays.com then please click the following link to email our support team:
Request essay removal


