Care Needs for Patient with Dementia
| ✅ Paper Type: Free Essay | ✅ Subject: Nursing |
| ✅ Wordcount: 4486 words | ✅ Published: 23 Sep 2019 |

Introduction
In this assessment I’m going to look at Dementia, explain what is it and what the effects are. I’m going to explore the person needs in relation to the condition, what the role of the carer/Multidisciplinary team are in assisting the person with dementia, what practices and what care settings are needed for the person suffering from dementia are. I will then outline what approaches there are for developing services for people with dementia.
What is dementia? What are the physiological and psychological changes that occur for the older person with Dementia?
What is Dementia:
‘A chronic or persistent disorder of the mental processes caused by brain disease or injury and marked by memory disorders, personality changes, and impaired reasoning’
Dictionary definition.
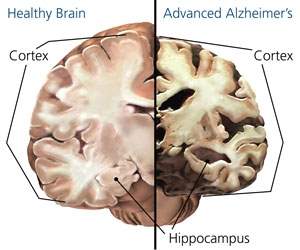
Dementia is a name for an overall group of systems associated with a decline in memory and thinking skills severe enough that will impact on the person’s day to day activities. There are over 400 types of dementia, Alzheimer’s makes up 60/80% of dementia cases, vascular dementia which occurs after the person has had a stroke and Lewy Body Dementia are some of the more common types. 85/90% of clients in nursing homes have Dementia. In the person suffering from Dementia it’s the loss of the ‘familiar’things like family names and events that impact on them. Dementia is not a normal part of ageing, it’s an illness and not to be confused with the person that is suffering from it. Dementia will affect everyone differently and no two cases are the same.
http://www.understandtogether.ie
There are 11 people diagnosed with dementia every day in Ireland, we have 55,000 people suffering from dementia with the figures expecting to rise to 113,000 by 2036. There is someone diagnosed with dementia every 3 seconds worldwide, there were an estimated 50 million people Worldwide diagnosed with dementia in 2017 expecting to rise to 75 million in 2030 and 131.5 in 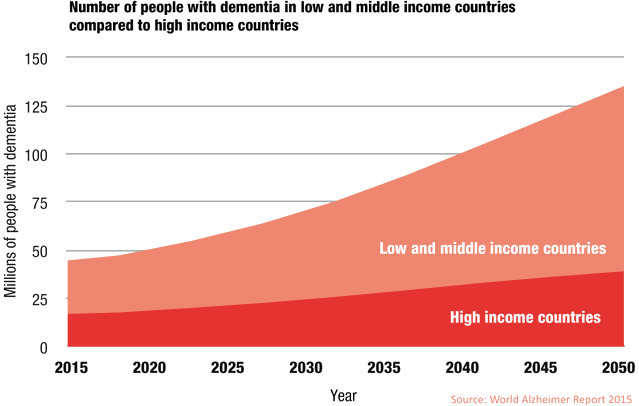 2050.
2050.
We owe a lot to a man called Professor Tom Kitwood who developed PCC (person centered care) he was a pioneer in the field of dementia, he challenged the old concept of care, he wanted to see the viewpoint from the person suffering from dementia. His idea was for his students to develop their own feelings, emotional and intuitive parts of themselves, so they could enrich their personal resources in their working and everyday lives. Innovations like this has played a major role in improving the care of dementia patients worldwide, helped us understand more who we are and more importantly who are the people that suffer from dementia are and how we can make their lives a little bit easier.
Physiological changes:
There are a number of physiological changes that occur to people suffering from dementia, people can start to forget the basic things like dressing or the correct order to dress in, this is known as dressing apraxia. Eating patterns can also be affected, the person may overeat leading to obesity or under eat leading to been malnourished, they may have forgetting to eat or may have eaten and forgotten they had eat. Sleeping can also be affected the person can mix up night and day. Motor Apraxia is when the person jerks or has uncoordinated movements, its not weakness of the affected parts.
https://medical-dictionary.thefreedictionary.com
Anomnia is the inability to recognize the written word and in particular familiar words, names and numbers. Agnosia is the inability to process sensory information, like Anomnia it’s the familiar objects faces and places that are not recognized, putting salt into their tea instead of sugar would be an example. Some dementia suffers are prone to slips, trips and falls due to apraxia and decline in spatial awareness.
Psychological changes:
Probably the most familiar one to the person suffering the psychological effects of dementia is memory loss, not remembering family members names, not remembering family past events. The person suffering from dementia can also have problems with where they are, they can be confused at home or if in care become disorientated not knowing where they are. The person suffering from dementia can also have issues with misplacing objects and in particular familiar objects, for example placing shampoo in the fridge and not been able to remember where familiar objects were left, not remembering where they put the keys to the car which are generally left in one particular place. The person suffering from dementia can become introverted and show signs of apathy, they lose interest in the people around them and more importantly they lose themselves. a person suffering from dementia will also repeat the same questions numerous times, repeat the same story over and over. Some persons can become paranoid and suspicious, they may think that the carer or family member has hidden something on them or accuse their wife/husband of having an affair. Maintaining a flowing conversation is another problem for some people that have dementia, this can lead to them been more withdrawn and isolated. Some persons can expierence hallucinations, some of them can be frightening while others will involve ordinary people, objects or situations from the past, usually found in the later stages of Alzheimer’s.
https://www.alz.org https://www.pinterest.ie
Explore the person’s needs in relation to the condition
Maslow hierarchy of needs was created by Abraham Harold Maslow in his influential paper called “A Theory of Human Motivation” in 1943. It’s a study based on healthy humans and what their needs are such as physiological and safety needs, it’s broken down in a pyramid shape, the bottom starts at physiological needs, safety need, love/belonging need, esteem need and self-actualization is the final goal. An example would be a person living in a war torn country their main concern would be their safety and not self-actualization.
 https://www.psychologytoday.com/us/blog/hide-and-seek/201205/our-hierarchy-needs
https://www.psychologytoday.com/us/blog/hide-and-seek/201205/our-hierarchy-needs
https://www.simplypsychology.org/maslow.html
Physical needs:
The most important thing when it comes to the person needs is to keep them involved, make them feel empowered and responsible, this will give them feelings of confidence and that they make a difference and matter, by simply letting them if they can put their own clothes on, asking them what they would like to eat, what their wishes are for the day will make them feel wanted and important.
If the person is suffering from incontinence a regular toileting regime is needed to ensure comfort, reduce embarrassment, help prevent skin irritation and breakdown and help reduce risk of urinary tract infection in females.
Depending on how far the person is with their dementia will depend on their ability to complete their activities of daily living and the assistance they require. If the dementia is advanced they the person will need assistance eating, there food may need to be pureed and their liquids thickened. Their ability to communicate may also be impaired, to build a relationship to the person we need to make eye contact, watch facial expressions and observe their body language, if there are not able to communicate verbally we can use pictures or sign boards to reach the gap. Speaking clearly, breaking down instructions, been patient, use short questions and check for understanding is very important as it avoids frustrating and confusion in the person.
A person with advanced dementia will need assistance with their hygiene, we can find out what their preference is for a shower or a bath and weather they prefer a wet shave or a dry shave. If the person is having issue dressing we may need to lay the clothes out on the bed or hold them up for the person and hand them the clothes. Having issues with going to the toilet is a very common issue as dementia progresses, having a good routine is place will help prevent issues like urinary tract infections, skin breakdown and irritation, if the person soils their bed sheets they need to be changed, the person washed and clothes put in the laundry, this makes the person feel fresh clean and confident.
If the person has apraxia they will need aids, aids like wearing glasses, walking frame and non-slip footwear, these should be left near the person at all times to prevent accidental slips, trips and falls. If possible the person should have an exercise regime in place, this will make them feel connected, prevent loneliness and maintain muscle mass and keep the joints flexible.
Familiarity is vital to the person suffering from dementia, avoid changes to their routine and leave dishes and cups in the same places helps ground them. Putting pictures on doors and cupboards will help them locate the items they need and lessened the chances of accidents happening.
If a person is showing signs of weight loss or weight gain they will need to be referred to a dietitian or a nutritionist, they will put a plan in place based on the person foods requirement which will be monitored and the person weigh to see what their progress is.
Sleeping during the day is to be avoided, this will insure regular sleep patterns at night. The person needs to remain active during the day and drinking fluids after 6pm is not recommended.
If a person is showing signs of aphasia or anomnia they will need to be referred to a
https://thumbs.dreamstime.com/z/alzheimer-s-disease-symbol-message-concept-25497014.jpg
speech therapist or a speech and language therapist. They will determine if it’s a speech or communication issue. If a person has agnosia they will need assistance and prompting using familiar things items like salt, sugar, toothpaste and cutlery as they often forget how to use these things.
http://www.theneuroethicsblog.com/2011/10/need-for-collaborative-definitions-in.html
Psychological/Intellectual Needs:
At the early stage of dementia, the person is encouraged to read, play Sudoku, jigsaws, card game and word search this keeps the brain active, preserve memory and keep the brain active. As the condition progresses the person will eventually need memory aids to keep them grounded, communicating in written form in clear, written instructions can empower the person to function independently for as long as possible. A message board is a helpful tool in this case, little reminders and messages help them retain some skills.
Communicating in clear, short sentences, pointing and using hand gestures and guidance helps the person stay involved in their active daily activities. Keeping and maintaining the same daily routines and structure will help retain the person’s skills and help prevent apathy.
Placing labels and pictures on cupboards, large clocks and large calendars will help the person find the things they need easier and help them stay centered and preserve cognitive functionality.
Social and emotional needs:
A person diagnosed with dementia will naturally feel very frightened and vulnerable, its important that the people around them are supportive and understanding, it can also be very upsetting to family members but they should try and be flexible and sensitive and try and cope with their own emotions. Each person diagnosed with dementia is a unique individual with their own set of emotions, sense of identity and personal history we should always try and promote them in retaining their sense of identity, support them with their faith, ask them their likes/dislikes and gather as much information on them as we can so we can understand them and support them to the best of our ability. Trying to imagine what it must be like by putting ourselves in their shoes will also make us have more empathy.
The person needs to be involved in their care for as long as its possible, this will give them a sense of ownership and help them retain their identity. Asking them what their opinion are and what preferences they have is very important making sure the tasks needing to be carried out are ‘done with the client’ and ‘not to the client’ this makes the person feel involved, that they matter and help preserve a sense of self-worth. Education is important for the person diagnosed with dementia, the more the person knows about how the condition will affect them the more, the services available and support open to them the more it will help reduce their anxiety and fears.
Active listening to the person is critical, finding out how they feel, what their concerns our, future plans and what sort of care they would like is vital, listening to the person and validating their concerns is important they should be allowed to talk openly and freely this will should help relieve agitation, anxiety and frustration they feel.
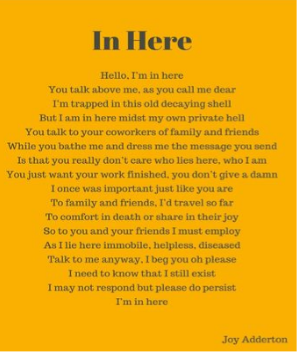
As the person progresses with dementia it will become impossible for them to connect to us, as carers we will need to ‘build a bridge to connect to them’ if the person is showing signs of challenging behavior we need to try and discover what the reason for this is, as they cannot communicate to us they may try and communicate in another fashion and it may come across as challenging but the onus is on the care to discover what they need help with ‘see the person not the behavior’ we need to remember we are dealing with an adult and they should be treated as an adult with respect at all times, never contradicting, talking down too, patronized or made to feel they are not be listened too acting like this will diminish their self-worth and make they grow more introvert.

Like all human beings the person suffering from dementia needs sense of connection, connection to their family’s and the people around them. We can help this by keeping them active and involved in any activities and social engagements. The family can be present at meal times and if the person is able to be brought out, they can bring them out for exercise. Encouraging and assisting the person helps prove them stimulation, prevents isolation, maintains social skills and promotes inclusion.
From reading the person care plan we should be able to see what hobbies, pastimes and interests the person has, from this we can put together activities that will be stimulating, have meaning for the person, this will help prevent apathy that occurs with dementia, boredom, sense of purpose and help reduce challenging behavior through a positive diversion. Activities like reminiscence, music, pet and doll therapy, sudoku, puzzles, painting, baking, card games, bingo and flower arranging people can relate too and help them engage more.
The persons environment plays a vital role, the longer a person can be kept at home and in their community as this will help them feel connected, give them a sense of security and familiarity. There are a number of supports and services available now that help promote keeping the person at home longer, support services like myhomecare.ie offer a service that will train and support home care workers to help the person with whatever needs they have at home. The person needs to be kept involved in matters to do with them and their care, if the person is in a nursing home the room should be decorated to make them feel more at home and the family should be involved. Personal objects like ornaments, pictures and cushions should be incorporated into the room to help them settle and feel comfortable. If special occasions arise the person should be assisted in dressing up and for general day to day, they should be assisted to help them in their appearance and take pride in themselves, this will give them a sense of self-esteem and help promote a positive self-image.
What is the role of the carer and multidisciplinary team in assisting the person with dementia, what practices need to be implemented, what care settings are available?
Carer:
‘A carer is anyone who cares, unpaid, for a friend or family member who due to illness, disability, a mental health problem or an addiction cannot cope without their support’
Multidisciplinary team:
‘A multidisciplinary team is a group of health care workers who are members of different disciplines (professions e.g. Psychiatrists, Social Workers, etc.), each providing specific services to the patient. … This co-ordinate their services and gets the team working together towards a specific set of goals’
The role of a carer/multidisciplinary
Communication is important for both the carer and the multidisciplinary team, been able to communicate in verbal form and written form is essential. Working as a team member and been able to follow written and verbal instructions is very important as it means there can be less of a chance of a breakdown in communication and everybody knows their job. Been able to communicate with one another is important in everyday live its more important when it concerns the care of other people so making sure we are understood and we can understand one another is critical both in verbal and written form like reports.
The role of a carer/multidisciplinary team should be centered around Person centered care, person centered care sees the person in need of care as equal partners in planning, developing and monitoring care to make sure it meets their needs. It means putting the person and their families at the center of decisions and seeing them as experts working alongside professionals to meet their needs.
They should be trying to preserve the person identity as long as possible, avoiding elder speak and calling them by their name, always explain what they are doing and ask for consent from the person, giving them choices in regards to eating as this will make them feel independent, promoting independence will make them feel valued and there their choice matters help preserving their identity. Always respecting their values and beliefs, if they are a church going person and if they are able to bring them to a mass even though you may be non-Christian and have no belief in it. Build a relationship with the person, focus on what they can do and be positive to them, build a bridge and go to them and not the other way around.
They will assist the person with their activities of daily living, observe the client and report any changes in them, they will work as part of a team communicate, share information both in written and verbal format. They will follow the care plan and familiarize themselves with it insuring they know the level of assistance required and the therapy’s required.
There are a number of practices that can be implemented such as Management of actual and potential aggression (MAPA), this helps staff recognize the non-verbal/verbal signs which precede potential aggression and how to deal with such scenarios. Therapeutic lying can be used when a person with dementia becomes confused and the carer needs to calm them down or build a bridge to their reality, an example of that would be when a person thinks their parents are coming to visit, the carer can ask them about them and what ages they are instead of telling them their dead or not around anymore. Safeguarding of Vulnerable Adults (SOVA) this training is about protecting vulnerable adults and keeping them safe from harm. Its about recognizing the signs of abuse and knowing what to do, an example would be if another carer was taking money from a client and the client was showing signs of distress and the carer was able to discover the reason for the challenging behavior. Building a bridge to the person reality as they cannot build a bridge to ours, been with them and allowing them to be and be fully present in their company. The training of Dementia champions in hospitals in another new initiative, this is a person prime role in assisting staff with patients that have dementia.
Care settings:
- Community services
- Home health care
- Post-acute care
- long-term care
- Day care services
- Post-acute care (Short term)
- long-term care (Nursing home)
- Dementia units
- Respite services
State the current approaches towards developing quality services for people with Dementia.
The Irish government published the Irish National Dementia Strategy in 2014, in this report they listed a number of approaches and towards developing quality services for people with dementia. Healthcare assistants, healthcare professionals, clerical and administrative staff, volunteers and staff of external organizations should be all trained and updated in dealing with people with Dementia, training like MAPA (Management of actual or potential aggression) enables staff to feel more confident in de-escalating situations with dementia patients.
Memory clinics are a specialized service for people suffering with memory loss and dementia, they offer treatments and diagnose people that are concerned about their memory.
People suffering from dementia should be assisted for as long as possible to help them retain their skills and kept at home for as long as is possible. The training can be extended to community-based centers and care centers allowing the persons to remain in their home and remain a part of the community for as long as possible. Creating awareness by educating the family and the public on the lifestyles that can lead to dementia is another important strategy, healthy ageing promoting will enable people to live healthy lives and reduce their risk of getting dementia.
Restructuring the current model of dementia care from suffers living in nursing homes to creating dementia villages like the newly created dementia village in Bruff, Co Limerick a purpose-built community village that caters to dementia suffers, this is modeled on the first purpose dementia village which was created in Hogeweyk, Holland and opened in December 2009. Both models give the clients a sense of purpose by allowing them to live in smaller units to do things they wouldn’t normally be allowed do, they can bake, get their hair done, sensory garden, on site shopping center and coffee shop. The villages are staffed by people who have  been specifically trained in dealing with people that have dementia.
been specifically trained in dealing with people that have dementia.
Another new approach and in early development is focused ultrasound, it’s a non-invasive therapeutic therapy with the potential to improve the quality of live and decrease the cost for patients suffering from Alzheimer’s, it uses ultrasounds focused on the brain without using incision or radiation. It uses Magnetic resonance-guided focused ultrasound in combination with intravenously injected microbubbles. It’s very early to say what impact this therapy will or can have it but early signs are positive.
https://www.nature.com/articles/s41467-018-04529-6
https://www.fusfoundation.org/diseases-and-conditions/neurological/alzheimers-disease
Patient centered care is a holistic approach to dealing with people suffering from dementia, it revolves around having respect, been polite, been honest and treating the person with dignity at all times. Using the person’s name and helping them retain their independence and a sense of purpose is very important, having clear and concise communication with the person is vital to promote a positive relationship between carer and patient. The founding father of person centered care is Professor Tom Kitwood.
https://www.dementia.org.au/sites/default/files/20090604_Nat_CON_BrookerPersCentCare.pdf
Conclusion
I have learned a lot about dementia in this assessment, how it impacts the persons suffering with dementia socially, emotionally, intellectually and physically. I have also learned what sort of support and help they need. I think the government need to invest more in providing facilities like Bruff in Co Limerick, educate the population more on dementia as I didn’t know much about it before I started this assessment and course.
I learned what the role of the carer/multidisciplinary team is and how they can support and help the person with dementia. I also think the carer has a role to play in teaching and educating people around them that may know very little about dementia, I also learned about the practices needed to be implemented and about the care facilities available to the dementia patient and the supports available to their family.
In the final part of the assessment I learned a great deal on what therapies and the future of dementia help should be like. Villages like Bruff seem to be the way forward giving the person a sense of independence, connection and a purpose, new therapies like the focused ultrasound with its non-invasive surgery sounds very positive and hopefully it will be something that will produce a solution for dementia in the not too distant future.
Bibliography
- Alzheimers Assocation . (2018). In-home Care. Available: https://www.alz.org/help-support/caregiving/care-options/in-home-care. Last accessed 19/12/2018.
- ALZHEIMER’S DISEASE INTERNATIONAL. (2015). Dementia statistics. Available: https://www.alz.co.uk/research/statistics. Last accessed 19/12/2018.
- Carers Trust. (2015). About carers. Available: https://carers.org/what-carer Last accessed 27/12/2018.
- Dawn Brooker . (2007). Person Centred Dementia Care: Are you serious? Available: https://www.dementia.org.au/sites/default/files/20090604_Nat_CON_BrookerPersCentCare.pdf. Last accessed 02/01/2019.
- Farlex, Inc . (2003 – 2018). Medical Dictionary. Available: https://medical-dictionary.thefreedictionary.com/Apraxia. Last accessed 19/12/2018
- Focused Ultrasound Foundation. (2018). Focused Ultrasound Therapy. Available: https://www.fusfoundation.org/diseases-and-conditions/neurological/alzheimers-disease. Last accessed 02/01/2019
- Health Innovation Network. (2018). Person Centered Care. Available: https://healthinnovationnetwork.com/system/ckeditor_assets/attachments/41/what_is_person-centred_care_and_why_is_it_important.pdf . Last accessed 27/12/2018.
- HSE. (2018). Health Service Executive. Available: http://www.understandtogether.ie/about-dementia/. Last accessed 19/12/2018.
- HSE. (2018). Multi-disciplinary team. Available: https://www.hse.ie/eng/services/list/4/mental-health-services/dsc/communityservices/multidisciplinaryteam.html . Last accessed 27/12/2018.
- Irish Central Staff . (2017). Ireland’s first dementia village is planned to open in early 2018. Available: https://www.irishcentral.com/news/community/ireland-s-first-dementia-village-is-planned-to-open-early-in-2018 . Last accessed 02/01/2019.
- Jodi Scorr. (2018). Myhomecare at the National Dementia Care Conference 2018. Available: https://myhomecare.ie/advice-for-older-people/myhomecare-at-the-national-dementia-care-conference-2018/. Last accessed 27/12/2018.
- Joy Adderton. (2016). 7 best Dementia poems. Available: https://www.pinterest.ie/pin/412994228311596726. Last accessed 19/12/2018.
- Linda Fox. (1999). Obituary: Professor Thomas Kitwood. Available: https://www.independent.co.uk/arts-entertainment/obituary-professor-thomas-kitwood-1045269.html. Last accessed 19/12/2018.
- Merck Sharp & Dohme Corp. (2018). Settings for Care for Older People. Available: https://www.msdmanuals.com/home/older-people%E2%80%99s-health-issues/provision-of-care-to-older-people/settings-for-care-for-older-people . Last accessed 27/12/2018.
- NA. (2018). alzheimer-s-disease-symbol. Available: https://thumbs.dreamstime.com/z/alzheimer-s-disease-symbol-message-concept-25497014.jpg. Last accessed 21/12/2018
- Nature Communications. (2018). Blood–brain barrier opening in Alzheimer’s disease using MR-guided focused ultrasound. Available: https://www.nature.com/articles/s41467-018-04529-6 . Last accessed 02/01/2019.
- Neel Burton M.D. (2012). Our Hierarchy of Needs. Available: https://www.psychologytoday.com/us/blog/hide-and-seek/201205/our-hierarchy-needs. Last accessed 21/12/2018.
- Saul McLeod. (2018). Maslow’s Hierarchy of Needs. Available: https://www.simplypsychology.org/maslow.html . Last accessed 21/12/2018.
- The American Heritage® Science Dictionary. (2011). Dementia. Available: https://www.dictionary.com/browse/dementia. Last accessed 19/12/2018.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on UKEssays.com then please click the following link to email our support team:
Request essay removal


