Compassion Focused Therapy Intervention to Reduce Self-criticism
Info: 63607 words (254 pages) Dissertation
Published: 28th Jan 2022
Tagged: PsychologyTherapy
Abstract
Objectives
Self-criticism is a transdiagnostic process that is receiving increased research attention. This uncontrolled pilot study evaluated the feasibility and acceptability of a novel intervention based on Compassion Focused Therapy to reduce self-criticism, as well as investigating changes in a range of outcome and process measures.
Methods
Twenty-three student participants with significant impaired functioning associated with high levels of self-criticism completed a six-session formulation-focused intervention and a two-month follow-up appointment. Sessions were delivered weekly and the majority of techniques focused on increasing self-compassion. Self-report outcome and process measures were collected weekly prior to each session. Acceptability was assessed through qualitative feedback and rating scales.
Results
The intervention was feasible in terms of recruitment and retention of participants, and both the assessment methods and intervention were acceptable to participants. One way repeated measure ANOVAs showed statistically significant differences between pre and post-intervention on outcome measures (self-critical thinking, functional impairment, depression, anxiety, self-esteem and unhealthy perfectionism) and process measures (self-compassion, unhelpful beliefs about emotions and emotion regulation strategies). Participants either continued to improve between post-intervention and follow-up, or the gains were maintained between these two time points for all outcome measures. Effect sizes were medium to large for all outcome and process measures at both post-intervention and follow-up. Pearson correlations indicated that reductions in self-criticism were associated with increases in self-compassion suggesting it could be investigated further as a possible mediator of treatment outcome.
Conclusions
The compassion-focused intervention showed preliminary evidence of effectiveness for self-critical students and was a feasible and acceptable treatment approach.This intervention now requires investigation in a randomised controlled trial.
Contents
Click to expand Contents
1. Introduction
1.1 Self-criticism
1.2 The treatment of self-criticism
1.3 Constructs related to self-criticism and their treatment
1.3.1 Perfectionism
1.3.2 Self-esteem
1.3.3 Depressive rumination
1.4 Self-compassion interventions to target self-criticism
1.5 Student mental health
2. Aims
2.1 Hypotheses
3. Method
3.1 Ethical Approval
3.2 Design
3.3 Participants
3.4 Measures
3.4.1 Primary outcome measures
3.4.2 Secondary outcome measures
3.4.3 Process measures
3.4.4 Measures to aid formulation
3.4.5 Participant feedback
3.5 Procedure
3.6 Intervention
3.7 Feasibility & acceptability objectives
3.8 Data preparation and analysis
3.8.1 Hypotheses 1 & 2: Feasibility & acceptability
3.8.2 Hypotheses 3, 4 & 5: Changes in self-criticism and other outcomes
3.8.2.1 Therapist effects
3.8.2.2 Effects of waiting for intervention
3.8.2.3 Comparison between pre and post-intervention
3.8.2.4 Associations with reductions in self-criticism
4. Results
4.1 Participant demographic information
4.2 Hypothesis 1: Feasibility
4.2.1 Recruitment and retention
4.2.2 Inclusion / exclusion criteria
4.3 Hypothesis 2: Acceptability
4.3.1 Acceptability of assessment methods
4.3.2 Acceptability of the intervention
4.3.2.1 The intervention as a whole
4.3.2.2 Treatment rationale
4.3.2.3 Psycho-education components
4.3.2.4 Acceptability and use of specific techniques
4.3.2.5 Session attendance
4.4 Treatment protocol: fidelity & revisions
4.4.1 Fidelity
4.4.2 Protocol revisions
4.5 Changes in self-criticism and other outcomes
4.5.1 Therapist effects
4.5.2 Effect of waiting time for intervention
4.5.3 Hypotheses 3 and 4: Comparison between pre and post-intervention
4.5.3.1 Hypothesis 3A, 4 & 5: Primary outcome measures
4.5.3.2 Hypothesis 3B, 4 & 5: Secondary outcome measures
4.5.3.3 Hypothesis 3C, 4 & 5: Comparison between pre and post-intervention for process measures
4.5.3.4 Hypothesis 3C: Associations with reductions in self-criticism
5. Discussion
5.1 Hypothesis 1: Feasibility
5.2 Hypothesis 2: Acceptability
5.2.1 Acceptability of assessment methods
5.2.2 Acceptability of the intervention
5.3 Hypotheses 3, 4 & 5: Changes in self-criticism and other outcomes and associations between the changes
5.3.1 Impact on self-criticism and associated impairment
5.3.2 Changes in secondary outcome measures
5.3.3 Changes in process measure
5.4 Limitations
5.5 Strengths
5.6 Implications
5.7 Conclusions
References
Appendices contents page
Appendix 1. Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (PNM RESC) original approval (18.11.2014)
Appendix 2. Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (PNM RESC) modification approval (27.02.2015)
Appendix 3. Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (PNM RESC) modification approval (16.07.2015)
Appendix 4. Questionnaires completed at each time point
Appendix 5. Study questionnaires
Appendix 6. Participant feedback questionnaire
Appendix 7. Measure of frequencies of use of specific intervention techniques since end of treatment collected at two-month follow-up appointment
Appendix 8. Flow chart to show participants’ journey and involvement of therapists
Appendix 9. Online recruitment advertisement
Appendix 10. Participant information sheet
Appendix 11. Participant consent form
Appendix 12. Session protocols
Appendix 13. Blank participant formulation worksheet
Appendix 14. Participant booklets
Appendix 15. Post-intervention ratings of how useful participants found the intervention
Appendix 16. Post-intervention ratings of how useful participants found each technique
Appendix 17. Ratings of frequency of use for each technique since end of treatment collected at follow-up appointment
Appendix 18. Results of independent t-tests comparing the two therapists on participant measures across time points
Appendix 19. Results of linear regressions investigating relationship between (a) length of baseline (time between screening and pre-intervention), (b) time from screening to post-intervention and (c) time from pre to post intervention and change in study measures
Appendix 20. Line graphs for secondary outcome measures (PHQ-9, GAD-7, RSES and ‘maladaptive perfectionism) at main study time points
Appendix 21. Line graphs for process measures (SCS, ERQ-reappraisal, ERQ-suppression, and BES) at main study points
List of Tables
Table 1 Feasibility objectives and outcomes
Table 2 Acceptability of assessment methods and intervention
Table 3 Participant baseline demographic information
Table 4 Primary outcome measures: Results of one-way ANOVAs, means and standard deviations and effect sizes
Table 5 Secondary outcome measures: Results of one-way ANOVAs, means and standard deviations and effect sizes
Table 6 Process measures: Results of one-way ANOVAs, means and standard deviations and effect sizes
List of Figures
Figure 1 Study flow diagram showing recruitment process
Figure 2 Line graph to show mean scores for the Habitual Index of Negative Thinking (HINT) at screening, pre-intervention, post-intervention & follow-up (one standard deviation error bars)
Figure 3 Line graph to show mean scores for the Self-Critical Rumination Scale (SCRS) at screening, pre-intervention, post-intervention & follow-up (one standard deviation error bars)
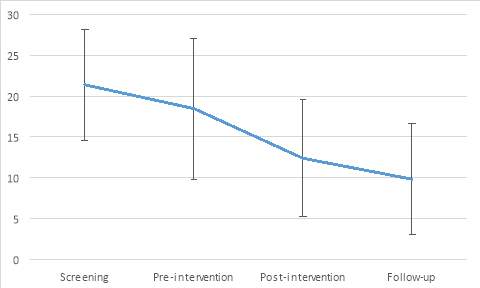
Figure 4 Line graph to show mean scores for the Work and Social Adjustment Scale (WASAS) at screening, pre-intervention, post-intervention & follow-up (one standard deviation error bars)
1. Introduction
1.1 Self-criticism
Self-criticism is a self-evaluative process where individuals judge themselves in a harsh or punitive way (Shahar et al., 2015). Self-criticism is considered to be a common experience; it has been reported across a range of settings including academia (Powers et al., 2011), and within both clinical and non-clinical populations (Baiao et al., 2014). Self-criticism has been described as a transdiagnostic process; high levels of self-criticism are predictive of a wide range of clinical difficulties including depression (Luyten et al., 2007), suicidality (O’Connor & Noyce, 2008), social anxiety (Cox, Fleet & Stein, 2004; Shahar, Doron & Szepsenwol, 2015) and eating disorders (Fennig et al., 2008). The relationship between self-criticism and depression has been a particular focus in previous research; levels of self-criticism have been found to predict depression and global psychosocial impairment in a clinical population after a four-year period (Dunkley et al., 2009). Self-critical individuals also have more difficulties forming and maintaining therapeutic relationships in treatment (Whelton, Paulson & Marusiak, 2007), and have poorer outcomes after treatment for depression (Marshall et al., 2008; Rector et al., 2000).
1.2 The treatment of self-criticism
Recently, specific interventions have been piloted to directly target high levels of self-criticism. Shahar et al (2012) found that an emotion-focused two-chair dialogue technique significantly reduced self-criticism in individuals recruited from university and community advertisements who scored at least one standard deviation above the means reported on the Forms of Self-Criticising/Attacking and Self-Reassuring Scale (FSCRS) by Gilbert et al (2004). These gains were maintained at a six-month follow-up (Shahar et al., 2012). Shahar et al (2015) used a Loving-Kindness Meditation (LKM) intervention with individuals who were ‘above average’ on the 11-item self-critical perfectionism subscale of the Dysfunctional Attitude Scale (SCP-DAS) (de Graaf, Roelofs & Huibers, 2009) and found significant reductions in self-criticism and increases in self-compassion compared to a waitlist control. Other than these studies, research focused on specific self-criticism interventions have been limited. Instead, interventions have been developed targeting overlapping or related constructs such as certain forms of perfectionism, self-esteem and rumination. These constructs will briefly be outlined below, including their relationship with self-criticism and the different treatment approaches designed to target them.
1.3 Constructs related to self-criticism and their treatment
1.3.1 Perfectionism
Self-criticism is often suggested to be a component of certain forms of perfectionism. Different types of perfectionism are thought to exist (Bergman, Nyland & Burns, 2007); for example, some have distinguished between maladaptive ‘self-critical perfectionism’ (SCP) (also called ‘evaluative-concerns’) and ‘positive striving’, a more adaptive perfectionism (Bieling, Israeli & Antony, 2004).SCP has been defined as a “hypersensitivity to perceived excessive external standards and criticism” (Powers et al., 2004, P. 62).Interestingly, Dunkley, Zuroff & Blankstein (2006) found that the Depressive Experiences Questionnaire (DEQ) (Blatt, D’Afflitti & Quinlan, 1976) self-criticism was the only sub-component of SCP that was a unique significant predictor of anxiety, depression and eating disorder symptoms after controlling for the effects of the other SCP subcomponents, suggesting that self-criticism is the key component of SCP that is associated with clinical problems.
Other researchers have drawn a distinction between perfectionism and ‘clinical perfectionism’, the latter of which has been conceptualised to include increased levels of self-critical thinking (Shafran, Cooper & Fairburn, 2002; 2003).Shafran, Cooper & Fairburn (2002) have developed a cognitive behavioural model of clinical perfectionism and CBT interventions have been shown significantly reduce clinical perfectionism (Riley et al., 2007; Steele et al., 2013). As part of these interventions, self-critical thoughts are targeted through psychoeducation, thought challenging and behavioural experiments. Of note, Steele et al (2013) found reductions in both perfectionism and the self-criticism subscale of the DAS (Weissman and Beck, 1978) after a group CBT intervention for psychiatric patients with clinical levels of perfectionism and a variety of Axis 1 diagnoses.
1.3.2 Self-esteem
Self-criticism is associated with lower self-esteem (Thompson & Zuroff, 2004) which in turn is a risk factor for mental health problems, such as depression and anxiety (Sowislo & Orth, 2013)and eating disorders (Cervera et al., 2003). High self-esteem has been defined in terms of a feeling that one is ‘good enough’ with a sense of self-worth (Rosenberg, 1989). In a CBT model of self-esteem, self-criticism is suggested to be a maintaining factor for low self-esteem (Fennell, 1998). Based on this model, a CBT intervention has been developed to improve self-esteem (Fennell, 1998; 2013). Part of this intervention targets self-criticism through thought challenging and behavioural experiments (Fennell, 2013). However, as this intervention contains multiple components, it is unclear to what extent self-criticism is a specific focus, and the impact of CBT for self-esteem on self-critical thinking has not been reported.
1.3.3 Depressive rumination
The relationship between self-criticism and rumination is also important to consider. Depressive rumination is defined as repetitive thinking or analysing about oneself, one’s symptoms or mood, as well as the reasons and implications of one’s problems (Nolen-Hoeksema, 1991; Watkins et al., 2014). Rumination is a risk factor for the onset and maintenance of depression (Nolen-Hoeksema, 2000). Self-critical individuals have a tendency to respond to low mood with more rumination (Spasojevic & Alloy, 2001). Although both self-criticism and rumination are self-focused, and rumination may include self-criticism, rumination is also conceptualised to include a far broader range of content including blaming others. Watkins and Nolen-Hoeksema (2014) conceptualise rumination as a learnt habitual behaviour. Watkins’ Rumination-Focused CBT (RF-CBT; Watkins et al., 2007; 2011) aims to identify warning signs of rumination and practice alternative responses to depressed mood in order to develop more adaptive habits. However, the impact of RF-CBT on self-critical thinking has not been investigated.
Like rumination, self-critical thinking could be conceptualized as a habitual response to, for example, making mistakes. An intervention to target self-criticism could therefore be based on a similar principle; identifying situations that trigger self-criticism and develop more adaptive habits. Research focused on self-compassion suggests that this could be an effective adaptive habit to teach individuals with high levels of self-criticism. This will be discussed further in the section below.
1.4 Self-compassion interventions to target self-criticism
Low levels of self-compassion have been suggested to be a key feature of self-critical individuals (Neff, 2003a). Self-compassion has been associated with lower levels of anxiety and depression, and higher levels of wellbeing and happiness (see Barnard & Curry, 2011; Macbeth & Gumley, 2012 for reviews). Furthermore, self-compassion has been found to partially mediate the relationship between self-criticism and depression (Joeng & Turner, 2015).
In an experimental design, Falconer et al (2014) found that a one-off virtual reality paradigm that focused on practicing a compassionate response to a child avatar from different perspectives led to reductions in self-criticism in individuals who reported high levels of self-criticism as measured by the FSCRS. However, such an approach is not available in most settings as requires virtual reality equipment.
A range of treatment approaches have been developed to increase self-compassion (e.g. Neff & Germer, 2012; Jazaieri et al., 2013; Gilbert, 2009). One of these, Gilbert’s Compassionate Focused Therapy (CFT) has been designed specifically for individuals with high levels of self-criticism and shame (Gilbert, 2009; 2010a). CFT is based on the idea that there are at least three types of emotion regulation systems: a threat-protection system, designed to detect and respond to threats in the environment; a drive-motivation system, designed to direct individuals towards appropriate rewards, and a contentment-soothing-safeness system, designed to regulate feelings of contentment and calm (Gilbert, 2010a). CFT uses a ‘threat/safety strategy’ formulation (Gilbert, 2010c) which focuses on the organisation of these three systems, with a particular focus on threat and safety strategy development (Gilbert, 2010a). In this formulation, an individual’s early experiences lead to the development of key ‘internal’ fears, i.e. fears that an individual has about themselves, and ‘external’ fears, i.e. fears that an individual has about other people or the world. Individuals then develop ‘safety protection strategies’ as a way of coping with these key fears. For example, individuals may use achievement as a way of avoiding negative events or feelings of rejection leading to over-active drive-motivation systems (Gilbert, 2009). Individuals may also engage in self-criticism as a safety strategy that develops, for example, in the context of abuse, bullying or harsh parenting styles (Gilbert, 2009). As a safety strategy, self-criticism has both ‘intended’ consequences such as ‘to learn from mistakes’ and ‘unintended’ consequences, such as ‘worry, anxiety and low mood’ (Welford, 2012). Over time, self-critical individuals become even more highly sensitive to threats and, because they focus most of their attentional resources on detecting and responding to threat, the contentment-soothing-safeness system does not develop properly (Gilbert & Irons, 2005). Thus, self-critical individuals are thought to have over-active threat-protection and drive-motivation systems, and an under-active contentment-soothing-safeness system (Gilbert, 2009). CFT therefore aims to develop the contentment-soothing-safeness system using Compassionate Mind Training (CMT); a range of skills and practices that focus on developing self-compassion (Gilbert, 2009; 2010b).
Self-compassion is thought to consist of a range of attributes including ‘care for well-being’: having the intention and commitment to care about oneself; ‘sensitivity to distress’: being aware and open to one’s distressing experiences; ‘non-judgement’: trying not to judge or condemn one’s thoughts, feelings and behaviours; ‘distress tolerance’: learning to tolerate one’s difficult feelings rather than avoiding them, and ‘sympathy’ and ‘empathy’: being emotionally touched by one’s experiences (Gilbert, 2009). In CMT, individuals are taught to, for example, accept and tolerate their emotional experiences and develop more compassionate beliefs about distressing and difficult emotions. This is particularly important given that, in line with previous research about ‘maladaptive’ perfectionism, self-critical individuals may have unhelpful beliefs about experiencing or expressing negative emotions (Rimes & Chalder, 2010), and as a result, may have a tendency to suppress difficult emotions. Specific CMT exercises include using compassionate thought records to develop a ‘compassionate reframe’ or a compassionate reappraisal of difficult situations (Gilbert, 2005). This technique may help individuals increase their use of ‘cognitive reappraisal’, an adaptive emotion regulation strategy (Gross, 1998). CMT also includes the use of imagery, for example, developing a ‘compassionate other’ image, which has been shown to reduce self-reported self-criticism in individuals with depression (Gilbert & Irons, 2004).
Although there is growing evidence-base for CMT for individuals with severe and enduring mental health problems (Gilbert & Procter, 2006; Mayhew & Gilbert, 2008), the CFT approach has not yet been applied to individuals with specific difficulties with self-criticism. This study aimed to develop a novel intervention based on CFT to target self-criticism in a student population as a form of early intervention.
1.5 Student mental health
Half of all mental health problems start by mid-teens and three quarters by the age of 24 years (Kessler et al., 2007). Furthermore, in 2012 approximately 80% of university students were aged between 18 (and under) and 24 years (Higher Education Statistics Agency, 2016). Therefore, providing interventions to university students is a potential method for addressing mental health problems at an early stage before they may become chronic.
Whilst at university, students face a range of different stressors, such as managing the transition from school to university, their academic studies, and issues related to diversity and relationships (Hurst et al., 2013). These burdens have been positively associated with depression (Mikolajczyk et al., 2008). In a UK student survey, 31% of females and 23% of males reported to have had depression in the preceding year (El Ansari et al., 2011). This is similar to the rates of depression in the general population (Blanco et al., 2008). However, the mental health of students has become a particular concern for universities (Castillo & Schwartz, 2013); both the number and severity of mental health problems in this population is increasing (Gallagher, 2008). Furthermore, mental health problems can have a negative impact on academic performance (Brackney & Karabenick, 1995) or lead students to prematurely end their education (Kessler et al., 1995). Mental health problems in young adulthood have also been associated with a number of negative outcomes including fewer employment opportunities (Eisenberg, Goldberstein & Gollust, 2007). Given this context, it has been suggested that university is a promising setting for the early intervention of mental health problems (Hunt & Eisenberg, 2010).
One advantage of targeting self-criticism is that it is a transdiagnostic factor associated with a range of different psychological problems. It can also be present and impairing in the absence of a full clinical disorder and therefore addressing it could be a form of primary prevention for mental health problems. For students, learning to effectively manage self-criticism is not only important because of its relationship to mental health problems, but it has also been found to be associated with lower levels of goal pursuit (Powers et al., 2011), which in turn could impact on a student’s academic performance. Furthermore, in academic settings there is a high prevalence of perfectionistic tendencies (Arpin-Cribbie et al., 2008) and maladaptive forms of perfectionism have been associated with higher levels of anxiety and depression in students (Kawamura et al., 2001). There may also be particular benefit in helping students increase their self-compassion; it has been associated with lower levels of procrastination (Williams, Stark & Foster, 2008), personal distress (Neff & Pommier, 2012), and an increased sense of self-efficacy (Iskender, 2009). Self-compassion has also been found to act as a ‘buffer’ against the difficulties associated with the transition to university such as homesickness (Terry, Leary & Mehta, 2014).
2. Aims
The present study involved the development of a new six-session intervention, drawing predominantly on methods from CFT, to reduce self-criticism in students with high levels of self-criticism. An uncontrolled pilot study was conducted with the following specific aims:
- To assess the acceptability and feasibility of the new intervention and assessment methods to investigate the impact of this intervention.
- To investigate changes in self-criticism, impaired functioning, depression, anxiety, self-esteem and ‘maladaptive’ perfectionism, comparing pre-treatment scores with those at post-treatment and two-month follow-up.
- To gain preliminary information about possible mechanisms of change including self-compassion, beliefs about emotions and emotion regulation strategies (‘cognitive reappraisal’ and ‘expressive suppression’), as these are all addressed in CFT.
2.1 Hypotheses
It was hypothesized that:
- The intervention would be feasible to deliver in terms of the recruitment and retention;
- Participants would find both the intervention and assessment methods acceptable;
- At post-treatment compared to baseline participants would report:
- Lower levels of self-criticism and associated impairments in functioning;
- Lower levels of depression, anxiety and ‘maladaptive’ perfectionism and higher levels of self-esteem;
- Higher levels of self-compassion and ‘cognitive reappraisal’ and a reduction in ‘expressive suppression’ and unhelpful beliefs about the unacceptability of negative emotions. Linked to this, it was hypothesised that reductions in self-criticism would be associated with increases in self-compassion, ‘cognitive reappraisal’ and reductions in ‘expressive suppression’ and unhelpful beliefs about emotions.
- There would be significantly larger improvements in key outcomes from pre-treatment to post-treatment than between screening and pre-treatment assessments.
- The gains made in the intervention would be maintained over time (i.e. between post-treatment and follow-up).
3. Method
3.1 Ethical Approval
Ethical approval was gained from the King’s College London (KCL) Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (see Appendices 1, 2 and 3).
3.2 Design
The study was an uncontrolled pilot study of a new intervention. A mixed qualitative and quantitative design was utilized in order to collect participant feedback about the acceptability of the intervention and assessment methods. Standardised questionnaire measures of self-criticism and other outcomes were completed at screening, prior to the weekly intervention sessions and at the 2-month follow-up appointment (see Appendix 4 for details about which questionnaires were completed at each time-point).
3.3 Participants
All participants were KCL students (see below for the inclusion and exclusion criteria). In regards to point 3 of the inclusion criteria, all participants had high scores on the self-criticism measures, however, an exact cut-off was not specified. Part of the development work of this study was to identify suitable questionnaire cut-off scores for inclusion as no previous studies were identified using this strategy.
Inclusion Criteria:
Exclusion Criteria:
|
The target sample size was 16-25 participants. This was in line with recommendations regarding sample sizes for pilot studies assessing intervention efficacy in a single group of participants (Hertzog, 2008).
3.4 Measures
Questionnaires were completed online using an online survey tool, Survey Monkey. To reduce burden placed on participants, the complete data set was only completed at session 1, 3, 6 and follow-up (see Appendix 4). Of note, two self-criticism questionnaires were completed at each time point. Two additional self-criticism questionnaires were completed once prior to session 1 to aid with the development of individualized formulations. The questionnaires are described below (see Appendix 5 for copies). The Cronbach’s alphas of the measures were examined at pre-intervention to confirm their internal consistency. Only the ‘doubts about actions’ subscale of the Multi-Dimensional Perfectionism Scale (MDPS) and the ‘inadequate self’ subscale of the FSCRS were below 0.70. Thus, the other measures were within satisfactory limits (Nunnaly & Bernstein, 1994).
3.4.1 Primary outcome measures
The Habitual Index of Negative Thinking (HINT) (Verplanken et al., 2007)
The HINT has 12 items measuring habitual negative self-thinking. Participants rated their agreement on a 5-point Likert scale ranging from “Strongly disagree” to “Strongly agree”. A score was given out of 60; higher scores represented higher levels of negative self-thinking. In previous research the internal consistency was 0.95 (Verplanken et al., 2007); in this study Cronbach’s alpha= 0.88.
Self-Critical Rumination Scale (SCRS) (Smart, Peters & Baer, 2015)
The SCRS has 10 items measuring self-critical rumination. Participants rated their agreement on a 5-point Likert scale ranging from “Strongly disagree” to “Strongly agree”. A score was given out of 40; higher scores represented higher levels of self-critical rumination. In previous research the internal consistency was 0.92 (Smart et al., 2015); in this study Cronbach’s alpha= 0.75.
Work and Social Adjustment Scale (WASAS) (Mundt et al., 2002)
The WASAS has 5 items and was used to measure the impact of self-criticism on different areas of an individual’s life. Each item focused on a different area of functioning such as work and home management.Participants rated their agreement on a 9-point Likert scale ranging from “Not at all” to “Very severely”.In previous research the internal consistency ranged from 0.70 to 0.94 (Mundt et al., 2002); in this study Cronbach’s alpha= 0.80. A score was given out of 40; higher scores represented more impaired levels of functioning. Scores of 10 and above are thought to indicate significant functional impairment (Mundt et al., 2002). As there is little evidence about scores on measures of self-criticism that would indicate a clinically significant level of self-criticism, the WASAS was used as the measure for calculating the proportion of the participants whose scores fell below clinical cut-off (i.e. WASAS score of 9 and below) after treatment.
3.4.2 Secondary outcome measures
Patient Health Questionnaire (PHQ-9) (Kroenke, Spitzer & Williams, 2001)
The PHQ-9 has 9 items measuring depressive symptoms over the last 2 weeks. Participants rated their agreement on a 4-point Likert scale ranging from “Not at all” to “Nearly every day”. A score was given out of 27; higher scores represented more severe depression. In previous research the internal consistency ranged from 0.86 to 0.89 (Kroenke et al., 2001); in this study Cronbach’s alpha= 0.83.
Generalised Anxiety Disorder (GAD-7) (Spitzer et al., 2006)
The GAD-7 has 7 items measuring anxiety over the last 2 weeks. Participants rated their agreement on a 4-point Likert scale ranging from “Not at all” to “Nearly every day”. A score was given out of 21; higher scores represented more severe anxiety. In previous research the internal consistency was 0.92 (Spitzer et al., 2006); in this study Cronbach’s alpha= 0.90.
Rosenberg’s Self-Esteem Scale (Rosenberg, 1965)
The RSES has 10 items measuring global self-esteem. Participants rated their agreement on a 4-point Likert scale ranging from “Strongly agree” to “Strongly disagree”. Items 3, 5, 8, 9 and 10 were reverse scored. In previous research the internal consistency ranged between 0.72 – 0.88 (Rosenberg, 1965); in this study Cronbach’s alpha= 0.81. A score was given out of 30; higher scores represented higher self-esteem.
The Multi-Dimensional Perfectionism Scale (MDPS) (Frost et al., 1990)
The MDPS has 35 items measuring perfectionism. Participants rated their agreement on a 5-point Likert scale ranging from “Strongly agree” to “Strongly disagree”. There are 6 subscales: ‘concern over mistakes’ (CM), ‘personal standards’ (PS), ‘parental expectations’ (PE), ‘parental criticism’ (PC), ‘doubts about actions’ (DA) and ‘organisation’ (O). For this study, the CM, DA, PE and PC subscales were totalled to measure ‘maladaptive’ perfectionism (Range: 22 – 110) (Stumpf & Parker, 2000). In previous research internal consistency ranged from 0.77 to 0.93 (Frost et al., 1990); in this study subscales Cronbach’s alpha ranged from 0.67 – 0.90.
3.4.3 Process measures
Self-Compassion Scale (SCS) (Neff, 2003b)
The SCS has 26 items divided into 6 subscales: 3 measure ‘self-compassion’ (‘common humanity’, ‘self-kindness’ and ‘mindfulness’) and 3 measure ‘coldness towards the self’ (‘self-judgement’, ‘over identification’ and ‘isolation’). Participants rate their agreement on a 5-point Likert scale ranging from “Almost never” to “Almost always”. Items from the 3 ‘coldness towards the self’ subscales are reverse scored. A score was given out of 130; higher scores represented higher levels of self-compassion. In previous research the internal consistency was 0.97 (Neff & Germer, 2013); in this study Cronbach’s alpha= 0.88.
The Emotion Regulation Questionnaire (ERQ) (Gross & John, 2003)
The ERQ has 10 items divided into 2 subscales measuring individual differences in the use of 2 emotion regulation strategies: ‘cognitive reappraisal’ and ‘expressive suppression’ (referred to as ‘reappraisal’ and ‘suppression’ in following sections). Participants rate their agreement on a 7-point Likert scale ranging from “strongly disagree” to “strongly agree”. Higher scores indicated a greater use of this type of strategy. In previous research the internal consistency was 0.79 for ‘reappraisal’ and 0.73 for ‘suppression’ (Gross & John, 2003); in this study Cronbach’s alpha was 0.79 for ‘reappraisal’ and 0.80 for ‘suppression’.
Beliefs about Emotions scale (BES) (Rimes & Chalder, 2010)
The BES has 12 items measuring the unacceptability of experiencing or expressing negative emotions. Participants rated their agreement on a 7-point Likert scale ranging from “totally agree” to “totally disagree”. A score was given out of 72; higher scores represented stronger beliefs about the unacceptability of negative emotions. In previous research the internal consistency was 0.91 (Rimes & Chalder, 2010); in this study Cronbach’s alpha= 0.83.
3.4.4 Measures to aid formulation
The Forms of Self-Criticizing/Attacking and Self-Reassuring Scale (FSCRS) (Gilbert et al., 2004)
The FSCRS has 22 items measuring different forms of self-critical and self-reassuring responses to a setback. It has 3 subscales: ‘inadequate self’ (9 items; internal consistency = 0.90), ‘hated self’ (5 items; internal consistency = 0.86), and ‘self-reassurance’ (8 items; internal consistency = 0.86). Participants rated their agreement on a 5-point Likert scale ranging from “Not at all like me” to “Extremely like me”. In this study, Cronbach’s alpha were 0.62 for ‘inadequate self’, 0.83 for ‘reassure self’ and 0.75 for ‘hated self’.
The Functions of Self-Criticizing/Attacking Scale (FSCS) (Gilbert et al., 2004)
The FSCS has 21 items examining reasons why individuals may be self-critical. It has 2 subscales: ‘self-correction’ (13 items; internal consistency = 0.92) and ‘self-persecution’ (8 items; internal consistency = 0.92). Participants rated their agreement on a 5-point Likert scale ranging from “Not at all like me” to “Extremely like me”. In this study Cronbach’s alpha for the whole scale was 0.72.
3.4.5 Participant feedback
Feedback was collected at various points throughout the study. In session 1, participants rated how ‘logical’ the intervention approach seemed to be on a 5-point Likert scale where 0 was “not at all” and 4 was “extremely”. Feedback was also collected online through Survey Monkey after the last intervention session (completion was optional). The survey was devised for the purpose of this study and contained both quantitative rating scales and open-ended questions (see Appendix 6). As part of this questionnaire, participants were asked to rate different aspects about the intervention on a 5-point Likert scale where 1 was “strongly disagree” and 5 was “strongly agree”. Participants also rated the usefulness of techniques on 5-point Likert scale where 0 was “not at all” and 4 was “very much”. At follow-up, participants rated how often they had used each technique since the end of treatment using a 6-point Likert scale where 0 was “not at all” and 5 was “every day” (see Appendix 7).
3.5 Procedure
The current study was completed by two trainee clinical psychologists. Both were involved equally in all stages of the study design, procedure and participant data collection. Therapist 1 (author) analysed the feasibility, acceptability and pre and post outcome data for the current study. Therapist 2 analysed the data that was collected from a qualitative interview that took place immediately prior to session 1. Appendix 8 displays a flow chart highlighting the participants’ journey through the study and the tasks completed by both therapists.
Two recruitment drives were completed; the first took place between February – March 2015, the second took place in September 2015. For each drive, the study was advertised twice through a fortnightly email about current KCL research projects and further information about the study was included on the KCL intra-net (see Appendix 9 for advertisement). Individuals who responded were sent a Participant Information Sheet (see Appendix 10) and a link to the screening questionnaires.
Individuals who appeared to meet the inclusion criteria were offered a telephone screening to further assess eligibility. During this screening, past and current mental health problems were assessed using the latest version of the Mini International Neuropsychiatric Interview (M.I.N.I) (English Version 6.0.0), a brief structured interview that assesses DSM-IV and ICD-10 psychiatric disorders through different modules (Medical Outcome Systems, 2016). The M.I.N.I has been validated against other clinical interviews and expert opinion across different European countries (Lecrubier et al., 1997; Sheehan et al., 1997; Amorim et al., 1998; Sheehan et al., 1998). If any risk issues were identified through the M.I.N.I ‘suicidality’ section, a further detailed risk assessment was completed.
Decisions about eligibility were made after discussions with the research team and then communicated to the individual by either phone or email. If they still wished to take part, participants then completed a participant consent form (see Appendix 11). Individuals who were not eligible were signposted to appropriate alternative sources of support.
Two trainee clinical psychologists delivered the intervention supervised by a consultant clinical psychologist. Treatment was offered on a first-come-first-served basis but also took account of participants’ availability to complete a course of weekly sessions. The average time between screening and session 1 was 13 weeks (SD=7.62).
Measures were completed weekly through Survey Monkey (see Appendix 4). Immediately prior to session 1, a semi-structured interview was conducted by the therapist about the participant’s experiences of self-critical thinking. This ranged from 45 minutes to 1.5 hours. These interviews were used for therapist’s 2 research project, however, the information gained was also utilised in session 1.
3.6 Intervention
The intervention consisted of six 1-hour individual sessions (seeAppendix 12 for session protocols). Sessions were delivered approximately weekly. The time between some of the sessions varied in length; reasons for this included university holidays and sickness. Every session was audio-recorded and listened to by the therapist’s supervisor to ensure fidelity to the protocol and for supervision purposes. A telephone follow-up appointment took place approximately 2-months post-intervention.
In session 1, the information gathered during the semi-structured interview was used to develop an individualized formulation with the participant based on Gilbert’s (2010c) ‘threat/safety strategy formulation’ (see Appendix 13). Participants were given psychoeducation about the self-compassion approach, including information about the 3-emotion regulation systems (Gilbert, 2009; 2010a). Finally, as part of the acceptability objectives, participants were given an overview of the intervention and rated how ‘logical’ the treatment rationale was.
The remaining sessions followed the same general structure: agenda setting and check in, review of the homework tasks, completion of an experiential exercise to practice a new technique and, finally, a summary of the session and homework setting. The sessions covered techniques primarily aimed at helping participants to reduce and cope with their self-critical thinking, as well as developing self-compassion. Throughout the sessions, where appropriate, links were made to the both the original formulation and the 3 emotion-regulation systems. Participants were given a booklet at the end of sessions 1-5 with further details about the session content (see Appendix 14). The treatment protocol and booklets were designed by the two trainee psychologists providing the intervention and their primary supervisor, drawing heavily from Gilbert’s Compassionate Mind approach as well as general cognitive behavioural therapy principles and research evidence about self-criticism.
3.7 Feasibility & acceptability objectives
Feasibility and acceptability were assessed through specific objectives which were further operationalized into specific outcomes (Thabane et al., 2010) (see Table 1 & 2).
Table 1 Feasibility objectives and outcomes
| Objective | Specific Objective | Outcome |
| Recruitment | How easy is it to recruit eligible participants? |
|
| Is the inclusion/exclusion criteria appropriate for the target population? |
|
|
| Retention | Do participants complete the intervention? | Number of drop outs:
|
Table 2 Acceptability of assessment methods and intervention
| Objective | Specific Objective | Outcome |
| Assessment methods | How acceptable are the:
|
|
| Intervention | How acceptable is the intervention content?
|
|
| How acceptable are the practical aspects of the sessions? |
|
3.8 Data preparation and analysis
3.8.1 Hypotheses 1 & 2: Feasibility & acceptability
Written responses to the open-ended feedback questions were analysed using brief content analysis (Mayring, 2000). Inductive category development was utilised whereby responses were read through and categories were defined based on the material. After reading through approximately 50% of the text for each question, these categories were refined before the entire text was analysed using the final categories.
3.8.2 Hypotheses 3, 4 & 5: Changes in self-criticism and other outcomes
As there were only 11 missing items across the dataset, mean item scores were computed and input for missing items (Fox‐Wasylyshyn and El‐Masri, 2005). As multiple tests were used, a more conservative cut-off p value ≤0.01 was used to indicate statistical significance; p values between 0.01 and 0.05 were considered to be a ‘non-significant trend’. As well as this, in line with the assumption of equal standard deviations, a rule of thumb was used for t-tests and ANOVAs to check that the smallest standard deviation between, for example, therapists, was not less than half of the largest standard deviation (Howell, 2012). Throughout, pre-intervention is defined as session 1 as this was the first time point that participants completed all measures; post-intervention is defined as session 6. Of note, a statistician was consulted prior to data analysis.
3.8.2.1 Therapist effects
Independent t-tests were completed to determine if there were differences in outcomes between therapists at each time point. The data was assessed to confirm that it met specific parametric assumptions. Although there were 3 extreme data-points, the inclusion and exclusion of them resulted in no changes to conclusions and they were therefore included in the analyses. Normality was assessed using the Shapiro-Wilk test. A number of time points for therapist (2) violated this assumption. However, as independent t-tests are considered ‘robust’ to deviations from normality, and the non-parametric Mann-Whitney U test resulted in no changes to the final conclusions, parametric t-tests were used. For each t-test, homogeneity of variances was also confirmed.
3.8.2.2 Effects of waiting for intervention
Linear regressions were used to investigate whether the time between screening and pre-intervention and the subsequent time to complete the intervention (time between screening and post-intervention and time between pre and post-intervention) predicted change in any of the study measures. It was confirmed that the data met the following assumptions for linear regressions: linearity, independence of observations, no significant outliers, homoscedasticity, and residuals (errors) were approximately normally distributed.
3.8.2.3 Comparison between pre and post-intervention
To examine the effect of the intervention on the study measures separate repeated measures ANOVAs were conducted for each measure with time as the repeated measure factor. The time points included were screening (if completed), pre-intervention, mid-treatment (session 3), post-intervention and follow-up. When a significant effect of time was found, planned pairwise comparisons were completed to determine whether there were significant differences between measures at the end of the intervention and follow-up compared with pre-intervention. A further t-test was conducted to investigate whether gains were maintained between post-intervention and follow-up. Contrasts between screening and pre-intervention were also completed to determine whether there were any significant changes during the baseline period prior to treatment.
Effect sizes were calculated using Cohen’s d and interpreted using the following cut-offs: ‘negligible’ effect <0.2; small effect ≥0.2, medium effect ≥ 0.5, large effect ≥ 0.8. Effect sizes for post-intervention and follow-up were calculated by dividing the mean differences between post and pre-intervention and follow-up and pre-intervention by the mean standard deviations at pre-intervention. Effect sizes were also calculated for measures collected at both screening and pre-intervention by dividing the mean difference between pre-intervention and screening by the mean standard deviation at screening. This was done to see how participants changed over time without treatment; these effect sizes are referred to as ‘pre-treatment changes’.
Across the dataset, there was 1 extreme outlier. As there were no changes to final conclusions without this data point, it was included in the analyses. Normality was assessed using the Shapiro-Wilk test. Although a number of time-points for the PHQ-9 and GAD-7 violated this assumption, since repeated measures ANOVA are considered ‘robust’ to deviations from normality and the non-parametric Friedman test resulted in no changes to the final conclusions, the ANOVAs are presented. Where the Mauchly’s test of sphericity indicated that the assumption of sphericity had been violated, Greenhouse-Geisser was used to correct the ANOVAs.
For outcome measures that were completed at both screening and pre-intervention, paired t-tests were also completed to determine whether there were statistically significant differences between the mean change in scores between screening and pre-intervention and between pre-intervention and post-intervention. Change in scores were computed by pre-intervention scores minus screening scores and post-intervention scores minus pre-intervention scores.
3.8.2.4 Associations with reductions in self-criticism
Pearson correlations were used to determine whether reductions in self-criticism were associated with increases in self-compassion and ‘reappraisal’, and reductions in ‘suppression’ and unhelpful beliefs about emotions. For this analysis, change in scores between pre-intervention and post-intervention were used.
4. Results
The results are presented in five different sections: participant baseline demographic information, feasibility and acceptability objectives and outcomes (see Table 1 & 2), details about the treatment protocol (fidelity and revisions), and descriptive statistics and statistical analyses for outcome data.
4.1 Participant demographic information
Table 3 summarizes baseline demographic information. The majority of participants were Caucasian female postgraduate students. Although only 7 participants had a current mental health diagnosis (anxiety and/or depression), 13 participants had a past diagnosis of depression.
Table 3 Participant baseline demographic information
| Characteristics | |
| Age, mean (SD), years | 25.3 (6.16) |
| Sex, n (%) | |
| Female | 19 (82.61) |
| Male | 4 (17.39) |
| Ethnicity, n (%) | |
| Caucasian | 17 (73.91) |
| Non-Caucasian | 6 (26.09) |
| Current antidepressant medication, n (%) | 2 (8.70) |
| Current Psychiatric Diagnoses at screening, n (%) | |
| None | 16 (69.57) |
| Depression | 1 (4.35) |
| Social phobia | 1 (4.35) |
| Generalised anxiety disorder (GAD) | 1 (4.35) |
| Social phobia & GAD | 1 (4.35) |
| Depression, social phobia & GAD | 1 (4.35) |
| Depression, agoraphobia, social phobia & GAD | 1 (4.35) |
| Depression, agoraphobia, obsessive compulsive disorder & GAD | 1 (4.35) |
| Past diagnosis of depression, n (%) | 13 (56.52) |
| Stage at university | |
| Undergraduate | 7 (30.43) |
| Postgraduate | 16 (69.57) |
4.2 Hypothesis 1: Feasibility
4.2.1 Recruitment and retention
Figure 1 displays the recruitment and retention numbers for this study. A sufficient number of eligible participants were recruited and subsequently completed the intervention.
Figure 1 Study flow diagram showing recruitment process
Responded to online advertisement (n=176)

Excluded (n=17)
- Lack of distress or significant impairment (n=4)
- Unsuitable level of English language (n=3)
- Alcohol dependence (n=3)
- Level of risk (n=2)
- Availability issues (n=2)
- Anorexia nervosa (n=1)
- Not stable medication (n=1)
- Receiving another intervention (n=1)
Completed screening questionnaires (n=93)








Offered telephone screening (n=68)
Assessed for eligibility (n=47)
Consented (n=30)
Withdrew prior to starting treatment (n=6)
- Change in personal circumstance (n=1)
- Started student counselling (n=1)
- Other family commitments (n=1)
- Unknown reasons (n=3)
Started treatment (n=24)
Did not complete treatment (n=1)
- Withdrew after session 2 due to life event
Completed treatment (n=23)
Complete two-month follow-up measures (n=23)
Attended telephone follow-up appointment (n=22)
4.2.2 Inclusion / exclusion criteria
The inclusion / exclusion criteria resulted in a group of participants who were all experiencing significant distress or impairment as a result of their self-criticism and were able to complete the intervention. There was therefore no indication that the criteria would need adjusting for a follow-on study.
4.3 Hypothesis 2: Acceptability
Twenty-one of the 24 participants completed the feedback questionnaire about the acceptability of the assessment methods and intervention. The open-ended questions were optional and therefore not always completed by all 21 participants.
4.3.1 Acceptability of assessment methods
Qualitative analysis revealed that the telephone screening appointment provided participants with a helpful introduction to the study and therapists. Some participants suggested that they would have preferred to complete this appointment face-to-face rather than over the phone due to the sensitive nature of some of the questions.
All participants completed the outcome measures at each time point (see Appendix 4). The qualitative analysis revealed that some participants thought that there were too many questionnaires in the full questionnaire pack. Some participants described the weekly questionnaires as “repetitive” to complete.
4.3.2 Acceptability of the intervention
4.3.2.1 The intervention as a whole
Results from the feedback ratings about the usefulness of the intervention are presented in Appendix 15. Of the 21 participants who completed these ratings, 100% of participants “agreed” or “strongly agreed” that the intervention was useful and that they would recommend it to others with high levels of self-criticism. Nineteen participants (90.5%) “agreed” or “strongly agreed” that their therapist understood their needs. Nineteen participants (90.5%) “agreed” or “strongly agreed” that the intervention reduced their self-criticism and 95.2% (n=20) “agreed” or “strongly agreed” that they had improved their ability to cope with it. In line with this, the qualitative analysis revealed that the intervention helped participants learn about the causes and negative impacts of self-criticism, as well as increasing their awareness and control over it. Seventeen participants (81%) “agreed” or “strongly agreed” that the intervention improved their self-compassion. Qualitative feedback revealed that participants had learnt how to use self-compassion towards their self-criticism as well as towards their distress more generally. For the single participant who had not agreed with the statements that the intervention had helped to reduce self-criticism or their ability to cope with it had, nevertheless, indicated that the intervention was helpful, their feedback about “the most important thing” about the intervention was inspected. This indicated that they had learned to view things in in a more positive light instead of focusing on the negative and that mental health requires effort and practice and should not be neglected or disregarded.
4.3.2.2 Treatment rationale
In session one 90.5% of participants (n=19) described the intervention rationale as either “very” or “extremely” ‘logical’ (Mean= 3.60, SD= 0.56).
4.3.2.3 Psycho-education components
The mean percentage of the weekly booklets read by participants was 79.5% (SD= 27.51).In the qualitative analysis participants described them as clear and comprehensive and as a useful way of recapping on the techniques covered in the sessions.
4.3.2.4 Acceptability and use of specific techniques
The mean time spent practicing techniques each week was 140.8 mins (SD= 155.58). Results from the ratings about the usefulness of each technique are presented in Appendix 16. All techniques were rated as at least “somewhat” useful by most of the participants. ‘Decentering’ and ‘compassionate reframes’ received the greatest proportion of the two highest usefulness ratings (both 76%, n=16). Relaxation had the smallest proportion of the two highest ratings, although 38% of participants (n=8) rated it as very useful.
At follow-up, 100% of participants who attended the telephone follow-up (n=22) had been using at least 1 of the techniques during the time between post-intervention and follow-up (see Appendix 17 participants’ reports of technique usage at follow-up). Fifteen participants (68%) had been using either ‘decentering’ or ‘compassionate behaviours’ at least “once a week”. Thirteen participants (59.3%) had been using ‘compassionate reframes’ at least “once a week”. Thus, ‘compassionate reframes’, ‘decentering’ and ‘compassionate behaviours’ were the most frequently used techniques. In the follow-up session, the majority of participants commented that the ‘compassionate reframe’ had become fairly automatic rather than a deliberate process each time.
4.3.2.5 Session attendance
Across all treatment phases, there were 16 cancelled and rearranged appointments. No sessions were missed without prior warning. The qualitative analysis revealed that the majority of participants could not identify anything that could have been changed about the delivery of the intervention to improve participation (n=16, 76.2%). Specific suggestions described by participants were offering sessions at a different point in the academic year (although further explanation as to why was not given), as well as offering longer sessions or sessions fortnightly, in the evenings or during weekends. Most participants felt the number of sessions had been appropriate; only 1 participant suggested that they would have preferred 1-2 additional sessions.
4.4 Treatment protocol: fidelity & revisions
4.4.1 Fidelity
For 21 participants, the full treatment protocol was followed. There were 2 participants whose treatment deviated (slightly) from the protocol. The first participant required a longer time to go through the ‘compassionate self’ technique (across 2 sessions rather than 1 session) and was therefore offered an additional telephone appointment to finalise the session 6 action plan. The second participant was slower to engage with the techniques practiced in the first few sessions and the decision was taken to support them using those techniques rather than practising new methods in session 5 or 6, although they received information about all techniques in the booklets.
4.4.2 Protocol revisions
The feedback and engagement of the first 4 participants were discussed in supervision and, based on these discussions, there were 3 minor changes to the treatment protocol. Firstly, the ‘self-criticism summary’ was made into a homework task after session 1 to allow more time in session 2 to practice the ‘compassionate reframe’. Secondly, in order to support participants to access their ‘compassionate self’ specific participant responses were incorporated into a script which was read and audio-recorded by the therapist. Finally, the ‘loving-kindness meditation’ was incorporated into the session 6 protocol, rather than given as a homework task.
4.5 Changes in self-criticism and other outcomes
4.5.1 Therapist effects
Independent t-tests revealed that at session 1, there was a significant difference in ‘suppression’ scores between therapist (1) (M= 11.73, SD= 5.71) and therapist (2) (M= 17.67, SD= 3.70); [t(21)= -2.99, p= 0.007]. No other statistically significant differences were found (see Appendix 18).
4.5.2 Effect of waiting time for intervention
Linear regression analyses showed that length of the baseline period, the time between screening and post-treatment and the time between pre-treatment and post-treatment were not significantly associated with the change in any of the study measures (see Appendix 19).
4.5.3 Hypotheses 3 and 4: Comparison between pre and post-intervention
The Results of one-way repeated ANOVAs for primary, secondary and process measures are displayed in Table 4, 5, & 6 respectively. Results of the subsequent planned pairwise comparisons are summarised below.
4.5.3.1 Hypothesis 3A, 4 & 5: Primary outcome measures
In line with hypotheses, there were statistically significant reductions between pre and post-intervention and between pre-intervention and follow-up for all primary outcome measures (p values ≤0.002). There were also statistically significant reductions between post-intervention and follow-up (p values ≤0.009) (Figures 2, 3 & 4 display mean scores for the HINT, SCRS and WASAS at main study time points). The Cohen’s d indicated that the intervention had a large effect size for self-criticism at both post-intervention and follow-up, compared with a small effect size for changes over the pre-treatment period. For impaired functioning there was a small effect size for the pre-treatment period, medium effect size from pre-treatment to post-intervention and a large effect size from pre-treatment to follow-up. No significant changes in the primary outcome measures were found over the baseline period between screening and pre-intervention (p values >0.08). Comparing change during the baseline period with the treatment period directly, paired t-tests indicated significantly larger reductions in pre- to post-treatment mean scores than screening to pre-treatment changes for the HINT [t(22)= -6.23, p<0.001], the SCRS [t(22)= -8.24, p<0.001], and the WASAS [t(22)= -5.07, p<0.001].
At post-intervention 8/23 (35%) of participant’s impaired functioning related to self-criticism reduced to below sub-clinical cut-off (Mundt et al., 2002). At follow-up, this had increased to 14/23 (61%) of participants.
Table 4 Primary outcome measures: Results of one-way ANOVAs, means and standard deviations and effect sizes
| Mean scores (standard deviations) | ANOVA | Effect sizes | |||||||||||
| Screening | Session 1 (Pre) | Session 2 | Session 3 | Session 4 | Session 5 | Session 6 (Post) | Follow-up | F (4, 88) | p-value | Pre-treatment changes (Pre – Screening) | Post – Pre | FU – Pre | |
| Habitual Index of Negative Thinking | 48.91
(5.09) |
47.35
(7.30) |
49.39 (5.15) | 46.52
(6.69) |
45.00 (5.05) | 43.00 (5.73) | 41.70
(5.76) |
37.35
(6.70) |
22.76 | <0.001 | -0.31 | -0.77 | -1.37 |
| Self-Critical Rumination Scale (i) | 32.13
(4.42) |
31.35
(4.83) |
31.04 (4.79) | 28.48
(5.60) |
27.48 (4.91) | 26.26 (5.75) | 23.61
(4.75) |
20.61
(5.47) |
36.93
(2.42, 53.30) |
<0.001 | -0.18 | -1.60 | -2.22 |
| Work and Social Adjustment Scale | 21.39
(6.79) |
18.48
(8.63) |
20.30 (7.86) | 17.70
(7.25) |
17.26 (7.68) | 15.87 (8.82) | 12.39
(7.15) |
9.83
(6.81) |
20.65 | <0.001 | -0.43 | -0.71 | -1.00 |
Notes:
Scores for session 2, 4 and 5 are included for information and were not included in any of the analyses.
(i) Greenhouse-Geisser correction applied & degrees of freedom listed in table; FU: Follow-up.
Figure 2 Line graph to show mean scores for the Habitual Index of Negative Thinking (HINT) at screening, pre-intervention, post-intervention & follow-up (one standard deviation error bars)
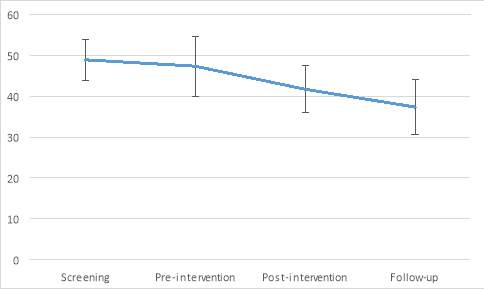
Figure 3 Line graph to show mean scores for the Self-Critical Rumination Scale (SCRS) at screening, pre-intervention, post-intervention & follow-up (one standard deviation error bars)
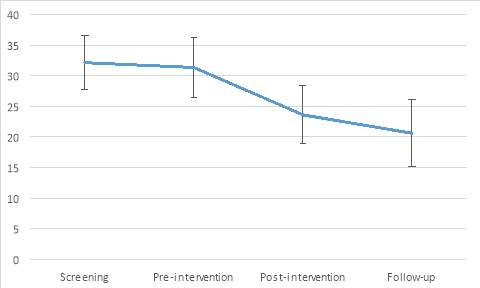
Figure 4 Line graph to show mean scores for the Work and Social Adjustment Scale (WASAS) at screening, pre-intervention, post-intervention & follow-up (one standard deviation error bars)
4.5.3.2 Hypothesis 3B, 4 & 5: Secondary outcome measures
In line with hypotheses, there were statistically significant differences between pre and post-intervention and between pre-intervention and follow-up for all secondary outcome measures (p values ≤0.005) (see Appendix 20 for line graphs displaying mean scores for the PHQ-9, GAD-7, RSES and ‘maladaptive’ perfectionism at main study time points).Participants reported lower levels of depression, anxiety and ‘maladaptive’ perfectionism, and higher levels of self-esteem at post-intervention and follow-up compared with pre-intervention.For depression, anxiety and self-esteem there was no significant further change between post-intervention and follow-up. There was a trend that participants reported lower levels of ‘maladaptive’ perfectionism between post-intervention and follow-up (p= 0.03).Cohen’s d indicated that the intervention had a medium effect size for depression at both post-intervention and follow-up, compared with a ‘negligible’ effect size for change over the pre-treatment period. For anxiety, there was a small effect size for change over the pre-treatment period, medium effect size at post-intervention and a large effect size at follow-up. For self-esteem, there was a small effect size for change over the pre-treatment period and a large effect size at both post-intervention and follow-up.The effect sizes for ‘maladaptive’ perfectionism were medium at post-intervention and large at follow-up.
No significant differences were found for depression, anxiety and self-esteem between screening and pre-intervention (p values >0.24). Indeed, additional paired t-tests indicated significantly larger changes in scores between pre-intervention to post-intervention than over the baseline period for the PHQ-9 [t(22)= -3.61, p=0.002], the GAD-7 [t(22)= -4.14, p<0.001], and the RSES [t(22)= 6.38, p<0.001].
Table 5 Secondary outcome measures: Results of one-way ANOVAs, means and standard deviations and effect sizes
| Mean scores (standard deviations) | ANOVA | Effect sizes | |||||||||
| Screening | Session 1 (Pre) | Session 3 | Session 6 (Post) | Follow-up | F (df) | p-value | Pre-treatment changes (Pre – Screening) | Post – Pre | Follow-up – Pre | ||
| df | (4, 88) | ||||||||||
| Patient Health Questionnaire (PHQ-9) | 7.87
(4.07) |
8.13
(5.15) |
7.52
(4.64) |
4.87
(4.53) |
4.83
(4.54) |
7.30 | <0.001 | 0.06 | -0.63 | -0.64 | |
| Generalised Anxiety Disorder (GAD-7) | 8.78
(4.32) |
7.78
(5.08) |
7.39
(5.05) |
4.91
(4.09) |
3.83
(3.51) |
12.58 | <0.001 | -0.23 | -0.56 | -0.78 | |
| Rosenberg Self-Esteem Scale (i) | 12.22
(3.77) |
13.22
(3.95) |
13.09
(3.90) |
17.57
(3.79) |
18.48
(3.84) |
30.11
(2.26, 49.73) |
<0.001 | 0.27 | 1.10 | 1.33 | |
| df | (3, 66) | ||||||||||
| ‘Maladaptive’ perfectionism | N/A | 69.70
(14.64) |
68.13
(14.47) |
61.48
(14.30) |
56.83
(13.79) |
14.62 | <0.001 | N/A | -0.56 | -0.88 | |
Notes: (i) Greenhouse-Geisser correction applied & degrees of freedom listed in table; df: degrees of freedom
4.5.3.3 Hypothesis 3C, 4 & 5: Comparison between pre and post-intervention for process measures
In line with hypotheses, there were statistically significant improvements between pre and post-intervention and between pre-intervention and follow-up for self-compassion, beliefs about negative emotions and the ‘reappraisal’ emotion regulation strategy (p values <0.005) (see Appendix 21 for line graphs displaying mean scores for the SCS, ERQ-reappraisal, ERQ-suppression and BES at main study time points). Cohen’s d calculations indicated large effect sizes for these three process measures at post-intervention; at follow-up, the effect size for self-compassion and beliefs about negative emotions was large and the effect size for ‘reappraisal’ was medium. For self-compassion and ‘reappraisal’, there was no further significant change between post-intervention and follow-up (p values >0.09). For the BES, there was a non-significant trend for participant’s beliefs about negative emotions to continue to improve between post-intervention and follow-up (p= 0.03).
In terms of the emotion regulation strategy ‘suppression’, there was statistically significant decrease between pre and post-intervention (p= 0.003) but between pre-intervention and follow-up there was only a non-significant trend (p= 0.016).There was no significant change between post-intervention and follow-up (p= 0.71).Cohen’s d indicated a medium effect size for this emotion regulation strategy at post-intervention and follow-up.
4.5.3.4 Hypothesis 3C: Associations with reductions in self-criticism
Pearson correlations were used to determine whether reductions in self-criticism were associated with increases in self-compassion and ‘reappraisal’, and reductions in ‘suppression’ and unhelpful beliefs about emotions. For the HINT, in line with predictions, there was a strong significant negative correlation between changes in self-criticism and self-compassion [r(23)= -0.65, p= 0.001]. The correlation between changes in self-criticism and unhelpful beliefs about emotions, [r(23)= -.34, p= 0.11], ‘reappraisal’ [r(23)= -0.32, p= .13] and ‘suppression’ [r(23)= 0.24, p= .27] were non-significant.
For the SCRS, there was also a strong significant negative correlation between changes in self-criticism and changes in self-compassion [r(23)= -0.67, p<0.001]. There was a trend that changes in self-criticism correlated negatively with changes in unhelpful beliefs about emotions [r(23)= 0.50, p= 0.02] and ‘reappraisal’ [r(23)= -0.48, p= 0.02]. The correlations between changes in self-criticism and ‘suppression’ [r(23)= 0.30, p= .17] were non-significant.
Table 6 Process measures: Results of one-way ANOVAs, means and standard deviations and effect sizes
| Mean scores (standard deviations) | ANOVA | Effect sizes | ||||||
| Session 1 (Pre) | Session 3 | Session 6 (Post) | Follow-up | F (3, 66) | p-value | Post – Pre | Follow-up – Pre | |
| Self-Compassion Scale | 60.13
(12.65) |
62.13
(12.75 |
81.30
(11.75) |
85.04
(14.97) |
46.82 | <0.001 | 1.67 | 1.97 |
| Emotion Regulation Questionnaire-Reappraisal | 27.48
(6.23) |
26.91
(6.37) |
32.48
(4.79) |
32.13
(4.95) |
8.73 | <0.001 | 0.80 | 0.74 |
| Emotion Regulation Questionnaire-Suppression | 14.83
(5.56) |
13.04
(4.51) |
12.00
(5.18) |
11.70
(5.61) |
4.58 | 0.006 | -0.51 | -0.56 |
| Beliefs about Emotions Scale | 45.04
(10.98) |
41.87
(11.98) |
33.91
(12.75) |
29.78
(11.33) |
17.57 | <0.001 | -1.01 | -1.39 |
5. Discussion
This uncontrolled pilot study investigated the feasibility and acceptability of a novel intervention targeting self-criticism in a student population. Changes in self-criticism and other outcome and process measures were also investigated by comparing scores at pre-intervention with those at post-intervention and two-month follow-up.
5. 1 Hypothesis 1: Feasibility
In line with the first hypothesis that the intervention would be feasible to deliver, advertisements on the university volunteer webpage and email circular were sufficient to recruit adequate numbers of participants for the study. Retention was also good; although 6 individuals who had consented to participate in the study withdrew before starting the intervention, only 1 dropped out once the intervention had started (due to a significant life event).
The inclusion criteria of a score of at least 10 on the WASAS was successful in selecting a participant sample who reported significant distress or impairment associated with self-criticism in the screening interview and who reported at least some benefit from the intervention. This study also provides information about the mean and SD scores on measures of self-criticism that could be utilized in relation to inclusion criteria in future research studies. It should be emphasized that although these participants had a significant level of impaired functioning due to their self-criticism, they were a student sample responding to an advertisement for a research study and were not a clinical population. Thus, future research would need to assess the applicability of these cut-offs to patient populations.
In line with previous research about gender differences in psychological help-seeking (Oliver et al., 2005), the majority of participants were female. Over 50% had experienced depression in the past which suggests that it may be helpful to intervene earlier. The majority of participants were also postgraduate students, so future research could focus more on recruiting undergraduate students or even those still at school or college. Research is needed into the prevalence of high levels of self-criticism in the secondary school/college population and the feasibility and acceptability of a similar intervention for this age group.
5.2 Hypothesis 2: Acceptability
5.2.1 Acceptability of assessment methods
In line with the second hypothesis that the assessment methods would be acceptable to highly self-critical students, the telephone screening appointment was described as a helpful way to introduce individuals to the study and specific therapists. Some participants would have preferred for this appointment to have been completed face-to-face due to the sensitive nature of the questions. This may also have allowed for greater rapport from an earlier stage.Future research could assess the feasibility of face-to-face screening, taking into account challenges such as the multisite nature of the campus, room-booking issues and the extra clinician time that would be required to book in sufficiently long screening slots. It could be that other formats, for example, Skype may be an appropriate way of providing individuals with the non-verbal therapeutic cues that are less evident over the telephone, whilst still being feasible for researchers to complete.
The weekly questionnaires were completed by every participant. However, qualitative feedback suggested that some participants found the full questionnaire pack to be too lengthy to complete. This study used several measures of self-criticism; this could be reduced in future research, and fewer process measures could be included. Some participants found it burdensome to complete weekly measures. Weekly assessment had been included in case of a high level of drop-out, however, as this was not a problem, the collection of data in future studies could be reduced to pre, post and follow-up.
5.2.2 Acceptability of the intervention
In line with the second hypothesis that the intervention would be acceptable to participants, the treatment rationale was rated as logical by 90.5% of participants and 100% either “agreed” or “strongly agreed” that the intervention was useful and that they would recommend it to others. Furthermore, only one participant dropped out after starting the intervention (due to a significant life event) which is also consistent with adequate treatment acceptability. At post-intervention participant feedback indicated that the practicalities of session appointments were also acceptable; all but one participant said that there were a sufficient number of sessions, and the majority of participants (76.2%) said that no changes could be made to the intervention delivery that would have improved participation. In line with some participant feedback, future research could consider offering a choice over frequency of appointments (for example, weekly or fortnightly), or offering evening appointments.
Participants engaged well with intervention protocols both within and between sessions. On average, participants reported spending over 2 hours practicing the intervention techniques each week. On average, participants read approximately 80% of session booklets, and described these as a useful way of recapping on the session techniques. This may provide an interesting avenue for future research; ‘guided self-help’, which commonly uses written psychoeducation components, are NICE recommended for common mental health problems (NICE, 2011), thus the effectiveness of a modified form the study intervention could be assessed within the context of, for example, an Improving Access to Psychological Therapies (IAPT) service.
In terms of the specific intervention techniques, on average, all techniques were rated as at least “somewhat useful”, and the mean rating for 6 out of 8 of these was “quite a lot”. ‘Decentering’ received the highest proportion of the top usefulness rating and at follow-up 68% reported using it at least “once a week”. ‘Decentering’ is thought to enable people to distance themselves from the content of their thoughts and emotions, and gain a sense of mastery over them (Gecht et al., 2014). In line with this, the qualitative feedback suggested that participants had learnt to control their self-criticism. The ‘compassionate reframe’ was the other most popular technique; 76% gave it the first or second highest usefulness rating, which was the same proportion as for ‘decentering’. Furthermore, at follow-up, approximately 60% of participants were continuing to use this technique at least “once a week”.
Although, on average, participants rated ‘compassionate behaviours’ as “somewhat” useful at the end of the intervention, at follow-up 68% were completing these “once a week”, making this one of the three most popular technique at this time point (in addition to ‘decentering’ and ‘compassionate reframes’).It is possible that initially participants found the idea of ‘compassionate behaviours’ threatening because they may have believed that they did not deserve to do nice things for themselves, but over time felt more comfortable with it (Gilbert, 2009).
Overall, there was nothing in the participant feedback that indicated that changes to the protocol are required. However, if the intervention were to be reduced in length, the findings suggest that ‘decentering’, ‘compassionate reframes’ and ‘compassionate behaviours’ may be the most appropriate methods on which to focus.
5.3 Hypotheses 3, 4 & 5: Changes in self-criticism and other outcomes and associations between the changes
5.3.1 Impact on self-criticism and associated impairment
As predicted, there were significant reductions in self-criticism and impaired functioning from pre to post-intervention and from pre-intervention to follow-up. The intervention had a large effect size for self-criticism and a medium to large effect size for impaired functioning. Overall, these findings provide preliminary indication that the intervention may be an efficacious treatment for self-criticism. However, due to the uncontrolled nature of the study, other explanations for the reductions in self-criticism and impairment cannot be ruled out. For example, the self-criticism may have reduced anyway with the passage of time. This explanation is less likely, however, given that the average time between screening and pre-intervention was 13 weeks (i.e. longer than the time taken to complete the intervention) and the changes between screening and pre-intervention for all study measures were non-significant, with ‘negligible’ to small effect sizes, compared with medium to large effect sizes between pre-treatment and post-intervention and follow-up. Also, paired t-tests showed that there were significantly larger changes between pre-intervention and post-intervention compared with screening and pre-intervention for measures collected at both time points. Nevertheless, further research using controlled study designs would be needed to confirm these findings.
Self-criticism and functional impairment continued to decrease between end of treatment and two-month follow-up. Indeed, although only 35% of participants had moved to scores below the ‘significant functional impairment’ range on the WASAS at post-intervention, this increased to 61% at follow-up. This may have been because the additional two months had given participants more time to practice the techniques and integrate them into their day-to-day life. It is also possible that the follow-up session helped to motivate or remind participants to continue applying the techniques as they knew they would be reporting back to their therapist.
In line with the reductions on the standardised outcome measures, the participant feedback highlighted that 100% “agreed” or “strongly agreed” that the intervention was useful. However, one participant indicated “neither agree nor disagree” in relation to both the statements that the intervention had reduced their self-criticism or improved their ability to cope with self-criticism. Although this participant had not benefitted in the two key ways intended, they reported that they had learnt to view things in a more positive light.
5.3.2 Changes in secondary outcome measures
In line with hypotheses, at post-intervention participants reported lower levels of depression, anxiety and ‘maladaptive’ perfectionism and higher levels of self-esteem, and gains were maintained at follow-up. The effect sizes were medium, medium to large and large for respective outcome measures at post-intervention and follow-up. Mean levels of depression moved from the upper end of the ‘mild’ range on the PHQ-9 to the cut-off between the ‘mild’ and ‘subclinical’ range. In terms of anxiety, mean scores moved from the ‘mild’ range to the ‘sub-clinical’ range (IAPT, 2010).
Although only a minority of participants met criteria for social phobia, anecdotally, a common theme reported by individuals was self-criticism related to social situations. The CBT model of social phobia highlights the role of anticipatory and post-event processing in this disorder which can include self-critical components (Rachman, Grüter-Andrew & Shafran, 2000). It may be interesting for future research to explore further the role of self-criticism with pre and post-event cognitive processing, and whether self-compassion techniques could help deal with these components.
At pre-treatment, the mean level of self-esteem was lower than in previous research using the RSES; for example, Sinclair et al (2010) reported a mean score of 19.67 in a general population sample of people aged 18 – 25. It is therefore encouraging that participants’ mean scores increased from their much lower mean level of 12.22 to a post-intervention level that was almost the same (18.48) as that general population sample. The ‘threat/safety strategy formulation’ (Gilbert, 2010b) helped participants to identify their ‘key internal fears’ which often corresponded to negative, global, self-devaluative ‘core’ beliefs such as “I am not good enough”. It is therefore possible that the intervention helped them re-evaluate and update these with a more compassionate view of themselves.
Levels of ‘maladaptive’ perfectionism significantly reduced from pre to post-intervention, and there was a non-significant trend that participants continued to improve between post-intervention and follow-up (the effect sizes were medium at post-intervention and large at follow-up). This is not surprising as self-criticism is considered to a key component of unhealthy or ‘self-critical’ perfectionism (Dunkley, Zuroff & Blankstein, 2006). Compassionate-focused intervention may merit further investigation for students who are impaired by their perfectionism.
5.3.3 Changes in process measure
The third aim of this study was to gain preliminary information about possible mechanisms of change of the intervention. Specifically, this study focused on four possible mechanisms: self-compassion, beliefs about emotions and emotion regulation strategies (‘reappraisal’ and ‘suppression’ were measured separately).
As predicted there was a significant increase in self-compassion from pre to post-intervention with a large effect size. Furthermore, in line with hypotheses, reductions in self-criticism were associated with increases in self-compassion. This suggests that self-compassion could be investigated as a potential mediator of treatment effects in future research. These findings are consistent with the theoretical orientation of the intervention which was strongly influenced by Gilbert’s Compassionate Mind approach (2009; 2010a) and the majority of techniques were specifically focused on increasing self-compassion. The aim of Gilbert’s approach is to help participants to activate their ‘contentment-soothing-safeness system’ whilst reducing activation of their ‘threat-protection system’ (Gilbert, 2009). It is interesting to note that, at follow-up, approximately 60% of participants were completing ‘compassionate reframes’ at least “once a week” and through further discussion the majority explained that they were completing these “in their head” rather than writing down the situations. This is consistent with Gilbert’s (2009) suggestion that it is important for self-critical individuals to change their self-to-self relating (i.e. their internal dialogue with themselves) to a more compassionate stance.
However, it is important to note that one participant disagreed with the statement that the intervention had helped them to improve their self-compassion and three rated that they neither agreed nor disagreed with this statement. It is possible that these participants may have benefitted from a more intensive intervention. Alternatively, some participants may have found it more useful to have a broader focus with less emphasis on self-compassion techniques.
In terms of the emotion regulation strategy ‘reappraisal’, there was a significant increase in the use of this from pre to post-intervention, with a large effect size. There was also a non-significant trend for increases in this strategy to be correlated with reductions in self-criticism. This is consistent with the aim of the ‘compassionate reframe’ technique to facilitate a specific form of reappraisal, i.e. a more self-compassionate way of viewing the situation.
Participants reported a significant reduction in their beliefs about the unacceptability of experiencing and expressing negative emotions pre to post-intervention and pre-intervention to follow-up. There was a non-significant trend that reductions in self-criticism were associated with reductions in these unhelpful beliefs about emotions. Part of the intervention focused on the idea that self-compassion is made up of a number of ‘compassionate attributes’, including attributes about emotional expression such as distress tolerance and taking a non-judgemental acceptance towards emotions (Welford, 2012). Through these, participants were encouraged to recognize the complexity of human experience and therefore not to judge or condemn their own feelings. Participants may therefore have re-evaluated their unhelpful beliefs about emotional expression and possibly developed more compassionate beliefs about how to respond to their own distress.
In terms of ‘suppression’, there was a significant reduction between pre and post-intervention and a non-significant trend for further reduction between pre-intervention and follow-up. Similarly, to that described above, it may have been that as participants’ beliefs about negative emotions improved, they relied on the use of ‘suppression’ less. The association between changes in self-criticism and suppression was not significant, however, this may have been a power issue.
In summary, the results from this study suggest that self-compassion could be investigated further as a possible mediator of treatment outcome, although the non-significant associations between self-criticism and beliefs about emotions and emotion regulation strategies may have been related to power issues. It is likely that there were many other mechanisms of change. For example, decentering was also taught as a technique to cope with self-critical thoughts. Future research could therefore use the Experiences Questionnaire (Fresco et al., 2007) to measure decentering as an additional possible mediator.
It may also be interesting for future research to investigate other potential mechanisms, for example, the intervention may have led to increases in positive self-talk, overall self-awareness or self-acceptance or decreases in positive beliefs about self-criticism. Additionally, it is possible that more general therapeutic factors such as the strength of the therapeutic relationship, the therapist warmth and kindness, or the therapist’s ability to model the self-compassionate approach mediated the change in outcome measures; these too could be investigated further in future research.
Uncontrolled pilot studies such as the current study are limited in their ability to investigate mechanisms of change. Nevertheless a recent systematic review highlighted the need for future research to identify the ‘active’ ingredients responsible for improvements after Compassion Focused Therapy (Leaviss & Uttley, 2015). Thus, future research could explore potential mediators using a randomised controlled trial (RCT), comparing the current intervention to another treatment approach, e.g. Cognitive Behavioural Therapy. Having an active control is necessary in order to show that the study intervention specifically leads to changes in the mediator, as well as showing that the mediator changes outcome measure. Furthermore, because mediation is a causal process, future research should measure proposed mediators at time points before the outcome variable (Windgassen et al., 2016).5.4 Limitations
A key limitation of the current study is that it was an uncontrolled pilot study. It is therefore possible that improvements were due to factors other than the specific intervention. However, the baseline period prior to the intervention beginning was, on average, longer than the intervention period, and there was no significant reduction in the outcome measures between screening and pre-treatment. Secondly, the intervention consisted of multiple techniques and because no component analysis was completed, it is unclear which techniques may have been effective in bringing about change. On the other hand, participant feedback did highlight differences in the subjective usefulness of different techniques which could be used to refine the intervention for future research. Thirdly, this study had a variable baseline period (time between screening and session 1). However, the results of linear regressions suggested that this pre-intervention time variation did not account for changes in study measures. Fourthly, although the sample size was in line with what is typically viewed as sufficient for an initial pilot study, power issues are likely to have affected some of the analyses such as the correlations between outcome and process measures. The results of this study could be used to inform power calculations for future research. Finally, the study sample consisted of a small group of mainly white female student participants at one university. It is unknown to what extent these findings, including effect sizes, are generalizable to students with other characteristics, to students at other universities or to a clinical population. The current results should therefore be interpreted with caution.
5.5 Strengths
One strength of the study was the use of a two-month follow-up assessment, which provided preliminary evidence that improvements were maintained. Two therapists provided the intervention with no significant therapist differences. Furthermore, fidelity to the treatment protocol was verified by the supervisor listening to all treatment sessions. Finally, all participants completed the full set of outcome measures at every assessment point, with only a few items being missing that could be pro-rated.
5.6 Implications
This study suggests that, like other processes such as depressive rumination, presenting self-criticism as a habit that is amenable to change is acceptable for highly self-critical individuals, and that a treatment rationale based on reducing self-criticism while increasing self-compassion seemed logical. The positive results in terms of both improvements on standardised outcome measures and qualitative feedback suggests that further research, such as a larger randomised controlled trial (RCT), would be warranted. Results from the current study could be used to guide power calculations, the choice of outcome measures and potential mediators to investigate. Future research could also explore the effectiveness of the intervention in different contexts, with different populations, or using different delivery formats, such as a group or a web-based approach.
5.7 Conclusions
Self-criticism is a transdiagnostic process associated with many mental health problems and poorer outcomes in disorder-specific therapies. This is one of the first studies to target self-criticism as the main focus of an intervention. This uncontrolled pilot study assessed the feasibility and acceptability of a novel formulation-driven intervention targeting self-criticism in university students who reported distress or impairment associated with self-criticism. Multiple techniques were taught over 6-weekly sessions, the majority of which were based on Compassion Focused Therapy and therefore focused on increasing self-compassion. The intervention was found to be feasible and acceptable to participants, and intervention effect sizes ranged from medium to large at post-intervention and two-month follow-up. Secondary analyses showed statistically significant improvements across a range of outcomes which were maintained at a 2-month follow-up. Reductions in self-criticism were associated with increases in self-compassion which could be investigated as a mediator of treatment outcome. Overall, these findings suggest that a 6-session compassion-focused intervention is a promising treatment approach for self-critical university students and a larger RCT would be a promising avenue for future research.
References
Amorim P, Lecrubier Y, Weiller E, Hergueta T, Sheehan D. (1998). DSM-III-R Psychotic Disorders: procedural validity of the M.I.N.I. International Neuropsychiatric Interview (M.I.N.I.). Concordance and causes for discordance with the CIDI. European Psychiatry, 13, 26-34.
Arpin-Cribbie, C. A., Irvine, J., Ritvo, P., Cribbie, R. A., Flett, G. L., & Hewitt, P. L. (2008). Perfectionism and psychological distress: A modeling approach to understanding their therapeutic relationship. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 26(3), 151-167.
Arpin-Cribbie, C., Irvine, J., & Ritvo, P. (2012). Web-based cognitive-behavioral therapy for perfectionism: a randomized controlled trial. Psychotherapy Research, 22(2), 194-207.
Baião, R., Gilbert, P., McEwan, K., & Carvalho, S. (2015). Forms of Self‐Criticising/Attacking & Self‐Reassuring Scale: Psychometric properties and normative study. Psychology and Psychotherapy: Theory, Research and Practice, 88(4), 438-452.
Barnard, L. K. & Curry, J. F. (2011). Self-compassion: Conceptualizations, correlates, & interventions. Review of general psychology, 15, 289.
Bergman, A. J., Nyland, J. E. & Burns, L. R. (2007). Correlates with perfectionism and the utility of a dual process model. Personality and Individual Differences, 43, 389-399.
Bieling, P. J., Israeli, A. L. & Antony, M. M. (2004). Is perfectionism good, bad, or both? Examining models of the perfectionism construct. Personality and Individual Differences, 36, 1373-1385.
Blanco, C., Okuda, M., Wright, C., Hasin, D. S., Grant, B. F., Liu, S.-M. & Olfson, M. (2008). Mental health of college students and their non–college-attending peers: results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of general psychiatry, 65, 1429-1437.
Blatt, S., D’Afflitti & Quinlan, D. M. (1976). Experiences of Depression in Normal Young Adults. Journal of Abnormal Psychology, 85(4), 383 – 389.
Brackney, B. E. & Karabenick, S. A. (1995). Psychopathology and academic performance: The role of motivation and learning strategies. Journal of Counseling Psychology, 42, 456.
Castillo, L. G. & Schwartz, S. J. (2013). Introduction to the special issue on college student mental health. Journal of clinical psychology, 69, 291-297.
Cervera, S., Lahortiga, F., Angel Martínez-González, M., Gual, P., Irala-Estévez, J. D. & Alonso, Y. (2003). Neuroticism and low self-esteem as risk factors for incident eating disorders in a prospective cohort study. International Journal of Eating Disorders, 33, 271-280.
Cox, B. J., Fleet, C. & Stein, M. B. (2004). Self-criticism and social phobia in the US national comorbidity survey. Journal of Affective Disorders, 82, 227-234.
De Graaf, L. E., Roelofs, J., & Huibers, M. J. (2009). Measuring dysfunctional attitudes in the general population: the dysfunctional attitude scale (form A) revised. Cognitive therapy and research, 33(4), 345-355.
Dunkley, D. M., Zuroff, D. C., & Blankstein, K. R. (2006). Specific perfectionism components versus self-criticism in predicting maladjustment. Personality and Individual Differences, 40(4), 665-676.
Dunkley, D. M., Sanislow, C. A., Grilo, C. M. & Mcglashan, T. H. (2009). Self-criticism versus neuroticism in predicting depression and psychosocial impairment for 4 years in a clinical sample. Comprehensive psychiatry, 50, 335-346.
Eisenberg, D., Golberstein, E. & Gollust, S. E. (2007). Help-seeking and access to mental health care in a university student population. Medical care, 45, 594-601.
El Ansari, W., & Stock, C. (2011). Feeling healthy? A survey of physical and psychological wellbeing of students from seven universities in the UK. International journal of environmental research and public health, 8(5), 1308-1323.
Falconer, C. J., Slater, M., Rovira, A., King, J. A., Gilbert, P., Antley, A., & Brewin, C. R. (2014). Embodying compassion: A virtual reality paradigm for overcoming excessive self-criticism. PloS one, 9(11), e111933.
Fennell, M. J. (1998). Cognitive therapy in the treatment of low self-esteem. Advances in Psychiatric Treatment, 4, 296-304.
Fennell, M. (2013). Cognitive Therapy for Low Self-Esteem: A Transdiagnostic Perspective. Workshop Handouts for University of Bath Clinical Psychology Doctorate
Fennig, S., Hadas, A., Itzhaky, L., Roe, D., Apter, A. & Shahar, G. (2008). Self‐criticism is a key predictor of eating disorder dimensions among inpatient adolescent females. International Journal of Eating Disorders, 41, 762-765.
Fox‐Wasylyshyn, S. M., & El‐Masri, M. M. (2005). Handling missing data in self‐report measures. Research in nursing & health, 28(6), 488-495.Fresco, D. M., Moore, M. T., van Dulmen, M. H., Segal, Z. V., Ma, S. H., Teasdale, J. D., & Williams, J. M. G. (2007). Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behavior therapy, 38(3), 234-246.
Frost, R. O., Marten, P., Lahart, C. & Rosenblate, R. (1990). The dimensions of perfectionism. Cognitive therapy and research, 14, 449-468.
Gallagher, R. (2008). National Survey of Counseling Center Directors. Available at: http://www.iacsinc.org/2008%20National%20Survey%20of%20Counseling%20Center%20Directors.pdf. Accessed on: March 1, 2016.
Gecht, J., Kessel, R., Forkmann, T., Gauggel, S., Drueke, B., Scherer, A., & Mainz, V. (2014). A mediation model of mindfulness and decentering: sequential psychological constructs or one and the same? BMC psychology, 2(1), 1.
Gilbert, P., Clarke, M., Hempel, S., Miles, J. & Irons, C. (2004). Criticizing and reassuring oneself: An exploration of forms, styles and reasons in female students. British Journal of Clinical Psychology, 43, 31-50.
Gilbert, P. (2005). Compassion: Conceptualisations, Research and Use in Psychotherapy. East Sussex: Routledge
Gilbert, P. (2009). Introducing compassion-focused therapy. Advances in Psychiatric Treatment, 15, 199-208.
Gilbert, P. (2010a). An introduction to compassion focused therapy in cognitive behavior therapy. International Journal of Cognitive Therapy, 3, 97-112.
Gilbert, P. (2010b). Compassion Focused Therapy: The CBT Distinction Features Series. East Sussex: Routledge
Gilbert, P. (2010c). An Introduction to the Theory & Practice of Compassion Focused Therapy and Compassionate Mind Training for Shame Based Difficulties. Available at: http://www.compassionatemind.co.uk/downloads/training_materials/1.%20Workbook_2010.pdf
Gilbert, P., & Irons, C. (2004). A pilot exploration of the use of compassionate images in a group of self‐critical people. Memory, 12(4), 507-516.
Gilbert, P., & Irons, C. (2005). Focused therapies and compassionate mind training for shame and self‐attacking. In P. Gilbert (Ed.), Compassion: Conceptualisations, research and use in psychotherapy (pp. 263–325). London: Routledge.
Gilbert, P. & Procter, S. (2006). Compassionate mind training for people with high shame and self‐criticism: Overview and pilot study of a group therapy approach. Clinical psychology & psychotherapy, 13, 353-379.
Gross, J. J. (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2, 271−299.
Gross, J. J. & John, O. P. (2003). Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85, 348.
Hertzog, M. A. (2008). Considerations in determining sample size for pilot studies. Research in nursing & health, 31(2), 180-191.
Higher Education Statistics Agency (2016, May 1). Higher Education Statistics for the United Kingdom 2012/3. Retrieved from: https://www.hesa.ac.uk/component/content/article?id=3129
Howell, D. (2012). Statistical Methods for Psychology. 8th Belmont, California: Wadsworth Publishing.
Hunt, J. & Eisenberg, D. (2010). Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health, 46, 3-10.
Hurst, C. S., Baranik, L. E. & Daniel, F. (2013). College student stressors: A review of the qualitative research. Stress and Health, 29, 275-285.
Ibrahim, A. K., Kelly, S. J., Adams, C. E., & Glazebrook, C. (2013). A systematic review of studies of depression prevalence in university students. Journal of psychiatric research, 47(3), 391-400.
Improving Access to Psychological Therapies (2011). The IAPT Data Handbook: Guidance on recording and monitoring outcomes to support local evidence-based practice. National IAPT programme. Available at: http://www.iapt.nhs.uk/services/measuring-outcomes.
Iskender, M. (2009). The relationship between self-compassion, self-efficacy, and control belief about learning in Turkish university students. Social Behavior and Personality: an international journal, 37(5), 711-720.
Jazaieri, H., Jinpa, G. T., Mcgonigal, K., Rosenberg, E. L., Finkelstein, J., Simon-Thomas, E., Cullen, M., Doty, J. R., Gross, J. J. & Goldin, P. R. (2013). Enhancing compassion: A randomized controlled trial of a compassion cultivation training program. Journal of Happiness Studies, 14, 1113-1126.
Joeng, J. R., & Turner, S. L. (2015). Mediators between self-criticism and depression: Fear of compassion, self-compassion, and importance to others. Journal of counseling psychology, 62(3), 453.
Kawamura, K. Y., Hunt, S. L., Frost, R. O., & DiBartolo, P. M. (2001). Perfectionism, anxiety, and depression: Are the relationships independent? Cognitive Therapy and Research, 25(3), 291-301.
Kessler, R. C., Foster, C. L., Saunders, W. B. & Stang, P. E. (1995). Social consequences of psychiatric disorders, I: Educational attainment. American journal of psychiatry, 152, 1026-1032.
Kessler, R. C., Amminger, G. P., Aguilar‐Gaxiola, S., Alonso, J., Lee, S., & Ustun, T. B. (2007). Age of onset of mental disorders: a review of recent literature. Current opinion in psychiatry, 20(4), 359.
Kroenke, K., Spitzer, R. & Williams, J. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606-613. Leaviss, J., & Uttley, L. (2015). Psychotherapeutic benefits of compassion-focused therapy: an early systematic review. Psychological medicine,45(05), 927-945.
Lecrubier Y, Sheehan D, Weiller E, Amorim P, Bonora I, Sheehan K, Janavs J, Dunbar G. (1997). The M.I.N.I. International Neuropsychiatric Interview (M.I.N.I.) A Short Diagnostic Structured Interview: Reliability and Validity According to the CIDI. European Psychiatry, 12: 224-231.
Luyten, P., Sabbe, B., Blatt, S. J., Meganck, S., Jansen, B., De Grave, C., Maes, F. & Corveleyn, J. (2007). Dependency and self‐criticism: relationship with major depressive disorder, severity of depression, and clinical presentation. Depression and anxiety, 24, 586-596.
Macbeth, A. & Gumley, A. (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32, 545-552.
Marshall, M. B., Zuroff, D. C., McBride, C., & Bagby, R. M. (2008). Self‐criticism predicts differential response to treatment for major depression. Journal of clinical psychology, 64(3), 231-244.
Mayhew, S. L. & Gilbert, P. (2008). Compassionate mind training with people who hear malevolent voices: A case series report. Clinical psychology & psychotherapy, 15, 113-138.
Mayring, P. (2000). Qualitative Content Analysis. Forum: Qualitative Social Research, 1(2), 20, 1-10.
Medical Outcome Systems (2016, March 1) M.I.N.I International Neuropsychiatric Interview (M.I.N.I 6.0). Retrieved from: http://www.medical-outcomes.com/index/faq
Mikolajczyk, R. T., Maxwell, A. E., Naydenova, V., Meier, S. & El Ansari, W. (2008). Depressive symptoms and perceived burdens related to being a student: Survey in three European countries. Clinical Practice and Epidemiology in Mental Health, 4, 19.
Mundt, J. C., Marks, I. M., Shear, M. K. & Greist, J. M. (2002). The Work and Social Adjustment Scale: a simple measure of impairment in functioning. The British Journal of Psychiatry, 180, 461-464.
Neff, K. (2003a). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and identity, 2, 85-101.
Neff, K. D. (2003b). The development and validation of a scale to measure self-compassion. Self and identity, 2, 223-250.
Neff, K. D. & Germer, C. K. (2013). A pilot study and randomized controlled trial of the mindful self‐compassion program. Journal of clinical psychology, 69, 28-44.
Neff, K. D., & Pommier, E. (2013). The relationship between self-compassion and other-focused concern among college undergraduates, community adults, and practicing meditators. Self and Identity, 12(2), 160-176.
NICE (2011). Common mental health problems: identification and pathways to care. NICE Clinical Guideline 123. London: National Institute for Health and Clinical Excellence.
Nolen-Hoeksema, S. (1991). Responses to depression and their effects on the duration of depressive episodes. Journal of abnormal psychology, 100, 569.
Nolen-Hoeksema, S. (2000). The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of abnormal psychology,109(3), 504.
Nunnaly, J. C., & Bernstein, I. H. (1994). Psychometric theory. Sydney: McGraw-Hill.
O’Connor, R. C., & Noyce, R. (2008). Personality and cognitive processes: Self-criticism and different types of rumination as predictors of suicidal ideation. Behaviour Research and Therapy, 46(3), 392-401.
Oliver, M. I., Pearson, N., Coe, N., & Gunnell, D. (2005). Help-seeking behaviour in men and women with common mental health problems: cross-sectional study. The British Journal of Psychiatry, 186(4), 297-301.
Powers, T. A., Zuroff, D. C. & Topciu, R. A. (2004). Covert and overt expressions of self‐criticism and perfectionism and their relation to depression. European Journal of Personality, 18, 61-72.
Powers, T. A., Koestner, R., Zuroff, D. C., Milyavskaya, M. & Gorin, A. A. (2011). The effects of self-criticism and self-oriented perfectionism on goal pursuit. Personality and Social Psychology Bulletin, 37, 964-975.
Rachman, S., Grüter-Andrew, J., & Shafran, R. (2000). Post-event processing in social anxiety. Behaviour Research and Therapy, 38(6), 611-617.
Rector, N. A., Bagby, R. M., Segal, Z. V., Joffe, R. T., & Levitt, A. (2000). Self-criticism and dependency in depressed patients treated with cognitive therapy or pharmacotherapy. Cognitive Therapy and Research, 24(5), 571-584.
Riley, C., Lee, M., Cooper, Z., Fairburn, C. G. & Shafran, R. (2007). A randomised controlled trial of cognitive-behaviour therapy for clinical perfectionism: A preliminary study. Behaviour Research and Therapy, 45, 2221-2231.
Rimes, K.A. & Chalder, T. (2010). The Beliefs about Emotions Scale: Validity, Reliability and Sensitivity to Clinical Change. Journal of Psychosomatic Research, 68, 295-282.
Rosenberg, M. (1965). Society and the adolescent self-image. Princeton, Princeton University Press.
Rosenberg, M. (1989). Society and the adolescent self-image (rev. ed.). Middletown, CT: Wesleyan University Press.
Schanche, E. (2013). The transdiagnostic phenomenon of self-criticism.Psychotherapy, 50(3), 316.
Shafran, R., Cooper, Z., & Fairburn, C. G. (2002). Clinical perfectionism: A cognitive–behavioural analysis. Behaviour research and therapy, 40(7), 773-791.
Shafran, R., Cooper, Z., & Fairburn, C. G. (2003). “Clinical perfectionism” is not “multidimensional perfectionism”: A reply to Hewitt, Flett, Besser, Sherry & McGee. Behaviour Research and Therapy, 41(10), 1217-1220.
Shahar, B., Carlin, E. R., Engle, D. E., Hegde, J., Szepsenwol, O., & Arkowitz, H. (2012). A pilot investigation of emotion‐focused two‐chair dialogue intervention for self‐criticism. Clinical Psychology & Psychotherapy, 19(6), 496-507.
Shahar, B., Szsepsenwol, O., Zilcha‐Mano, S., Haim, N., Zamir, O., Levi‐Yeshuvi, S., & Levit‐Binnun, N. (2015). A Wait‐List Randomized Controlled Trial of Loving‐Kindness Meditation Programme for Self‐Criticism. Clinical psychology & psychotherapy, 22(4), 346-356.
Shahar, B., Doron, G., & Szepsenwol, O. (2015). Childhood Maltreatment, Shame‐Proneness and Self‐Criticism in Social Anxiety Disorder: A Sequential Mediational Model. Clinical psychology & psychotherapy, 22(6), 570-579.
Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Janavs J, Weiller E, Bonara LI, Keskiner A, Schinka J, Knapp E, Sheehan MF, Dunbar GC. (1997). Reliability and Validity of the M.I.N.I. International Neuropsychiatric Interview (M.I.N.I.): According to the SCID-P. European Psychiatry, 12, 232-241.
Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar G. (1998). The M.I.N.I. International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview. J. Clin Psychiatry, 59(20), 22-33.
Sinclair, S. J., Blais, M. A., Gansler, D. A., Sandberg, E., Bistis, K., & LoCicero, A. (2010). Psychometric properties of the Rosenberg Self-Esteem Scale: Overall and across demographic groups living within the United States. Evaluation & the Health Professions, 33(1), 56-80.
Smart, L. M., Peters, J. R., & Baer, R. A. (2015). Development and validation of a measure of self-critical rumination. Assessment, 1073191115573300.
Sowislo, J. F. & Orth, U. (2013). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychological Bulletin, 139, 213.
Spasojević, J. & Alloy, L. B. (2001). Rumination as a common mechanism relating depressive risk factors to depression. Emotion, 1, 25.
Spitzer, R., Kroenke, K., Williams, J. & Löwe, B. (2006). A brief measure for assessing generalised anxiety disorder: the GAD-7. Archives of Internal Medicine, 166, 1092-1097.
Steele, A. L., Waite, S., Egan, S. J., Finnigan, J., Handley, A., & Wade, T. D. (2013). Psycho-education and group cognitive-behavioural therapy for clinical perfectionism: A case-series evaluation. Behavioural and cognitive psychotherapy, 41(02), 129-143.
Stumpf, H., & Parker, W. D. (2000). A hierarchical structural analysis of perfectionism and its relation to other personality characteristics. Personality and individual differences, 28(5), 837-852.
Terry, M. L., Leary, M. R., & Mehta, S. (2013). Self-compassion as a buffer against homesickness, depression, and dissatisfaction in the transition to college. Self and Identity, 12(3), 278-290.
Thabane, L., Ma, J., Chu, R., Cheng, J., Ismaila, A., Rios, L. P., Robson, R., Thabane, M., Giangregorio, L. & Goldsmith, C. H. (2010). A tutorial on pilot studies: the what, why and how. BMC medical research methodology, 10, 1.
Thompson, R., & Zuroff, D. C. (2004). The Levels of Self-Criticism Scale: comparative self-criticism and internalized self-criticism. Personality and individual differences, 36(2), 419-430.
Verplanken, B., Friborg, O., Wang, C. E., Trafimow, D. & Woolf, K. (2007). Mental habits: Metacognitive reflection on negative self-thinking. Journal of Personality and Social Psychology, 92, 526.
Waller, H., Garety, P. A., Jolley, S., Fornells-Ambrojo, M., Kuipers, E., Onwumere, J., … & Craig, T. (2013). Low intensity cognitive behavioural therapy for psychosis: a pilot study. Journal of behavior therapy and experimental psychiatry, 44(1), 98-104.
Watkins, E., Scott, J., Wingrove, J., Rimes, K., Bathurst, N., Steiner, H., Kennell–Webb, S., Moulds, M. & Malliaris, Y. (2007). Rumination-focused cognitive behaviour therapy for residual depression: A case series. Behaviour Research and Therapy, 45, 2144-2154.
Watkins, E. R., Mullan, E., Wingrove, J., Rimes, K., Steiner, H., Bathurst, N., Eastman, R. & Scott, J. (2011). Rumination-focused cognitive-behavioural therapy for residual depression: phase II randomised controlled trial. The British Journal of Psychiatry, 199, 317-322.
Weissman, A. N., & Beck, A. T. (1978). Development and validation of the Dysfunctional Attitude Scale: A preliminary investigation. Paper presented at the Annual Meeting of the American Educational Research Association, Toronto, Canada.
Welford, M. (2012). The Compassionate Mind Approach To Building Your Self-Confidence. Robinson: London.
Whelton, W. J., Paulson, B., & Marusiak, C. W. (2007). Self-criticism and the therapeutic relationship. Counselling Psychology Quarterly, 20(2), 135-148.
Williams, J. G., Stark, S. K., & Foster, E. E. (2008). Start today or the very last day? The relationships among self-compassion, motivation, and procrastination. American Journal of Psychological Research, 4, 37-44.
Windgassen, S., Goldsmith, K., Moss-Morris, R., & Chalder, T. (2016). Establishing how psychological therapies work: the importance of mediation analysis. Journal of Mental Health, 25(2), 93-99.
Appendices contents page
- Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (PNM RESC) original approval (18.11.2014)
- Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (PNM RESC) modification approval (27.02.2015)
- Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (PNM RESC) modification approval (16.07.2015)
- Questionnaires completed at each time point
- Study questionnaires
- The Habitual Index of Negative Thinking
- Self-Critical Rumination Scale
- Work and Social Adjustment Scale
- Patient Health Questionnaire (PHQ-9)
- Generalised Anxiety Disorder (GAD-7)
- Rosenberg’s Self-Esteem Scale
- The Multi-Dimensional Perfectionism Scale
- Self-Compassion Scale
- The Emotion Regulation Questionnaire
- Beliefs about Emotions scale
- The Forms of Self-Criticizing/Attacking and Self-Reassuring Scale
- The Functions of Self-Criticizing/Attacking Scale
- Participant feedback questionnaire
- Measure of frequencies of use of specific intervention techniques since end of treatment collected at two-month follow-up appointment
- Online recruitment advertisement
- Participant information sheet
- Participant consent form
- Session protocols
- Blank participant formulation worksheet
- Participant booklets
- Session 1
- Session 2
- Session 3
- Session 4
- Session 5
- Post-intervention ratings of how useful participants found the intervention
- Post-intervention ratings of how useful participants found each technique
- Ratings of frequency of use for each technique since end of treatment collected at follow-up appointment
- Results of independent t-tests comparing the two therapists on participant measures across time points
- Results of linear regressions investigating relationship between (a) length of baseline (time between screening and pre-intervention), (b) time from screening to post-intervention and (c) time from pre to post intervention and change in study measures
- Line graphs for secondary outcome measures (PHQ-9, GAD-7, RSES and ‘maladaptive perfectionism) at main study time points
- Line graphs for process measures (SCS, ERQ-reappraisal, ERQ-suppression, and BES) at main study points
Appendix 1. Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (PNM RESC) original approval (18.11.2014)
| Alexandra Rose and Ruth McIntyre Department of Psychology PO78 Addiction Sciences Building
Institute of Psychiatry, Psychology and Neuroscience King’s College London De Crespigny Park 20 November 2014 Dear Alexandra and Ruth, PNM/14/15-33 Self-criticism: Development of a new intervention Review Outcome: Full Approval Thank you for submitting your application for ethical approval. This was reviewed by the PNM RESC on 18 November 2014. As a result, the Committee have granted full ethical approval for your study. Provisos
You are not required to provide evidence to the Committee that these provisos have been met, but your ethical approval is only valid if these changes are made. You must not commence your research until these provisos have been met. Please ensure that you follow all relevant guidance as laid out in the King’s College London Guidelines on Good Practice in Academic Research (http://www.kcl.ac.uk/college/policyzone/index.php?id=247). For your information ethical approval is granted until 20 November 2017. If you need approval beyond this point you will need to apply for an extension to approval at least two weeks prior to this explaining why the extension is needed, (please note however that a full re-application will not be necessary unless the protocol has changed). You should also note that if your approval is for one year, you will not be sent a reminder when it is due to lapse. Ethical approval is required to cover the duration of the research study, up to the conclusion of the research. The conclusion of the research is defined as the final date or event detailed in the study description section of your approved application form (usually the end of data collection when all work with human participants will have been completed), not the completion of data analysis or publication of the results. If you do not start the project within three months of this letter please contact the Research Ethics Office. Should you wish to make a modification to the project or request an extension to approval you will need approval for this and should follow the guidance relating to modifying approved applications: http://www.kcl.ac.uk/innovation/research/support/ethics/applications/modifications.aspx Please would you also note that we may, for the purposes of audit, contact you from time to time to ascertain the status of your research. If you have any query about any aspect of this ethical approval, please contact your panel/committee administrator in the first instance (http://www.kcl.ac.uk/innovation/research/support/ethics/contact.aspx) Yours sincerely, James Patterson – Senior Research Ethics Officer For and on behalf of Professor Gareth Barker, Chairman Psychiatry, Nursing and Midwifery Research Ethics Subcommittee (PNM RESC) Cc: Katharine Rimes and Patrick Smith |
Appendix 2. Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (PNM RESC) modification approval (27.02.2015)
| Dr Ruth McIntyre and Alexandra Rose Doctoral Programme in Clinical Psychology Department of Psychology Institute of Psychiatry, Psychology and Neuroscience
King’s College London 27 February 2015 Dear Ruth and Alexandra, PNM/14/15-33 Self-criticism: Development of a new intervention Thank you for submitting a modifications request for the above study. I am writing to confirm approval of these. The approved modifications are summarised broadly below:
If you have any queries, please do not hesitate to contact the Research Ethics Office. Yours sincerely, James Patterson – Senior Research Ethics Office |
Appendix 3. Psychiatry, Nursing & Midwifery Research Ethics Subcommittee (PNM RESC) modification approval (16.07.2015)
| Alexandra Rose Doctoral Programme in Clinical Psychology Department of Psychology Institute of Psychiatry, Psychology and Neuroscience PO78 Addiction Sciences Building London SE5 8AF
16 July 2015 Dear Alexandra, PNM/14/15-33 Self-criticism: Development of a new intervention Thank you for submitting a modifications request for the above study. I am writing to confirm approval of this. The approved modification is broadly summarised below:
If you have any questions, please let me know. Yours sincerely, James Patterson – Senior Research Ethics Officer Cc: Ruth McIntyre |
Appendix 4. Questionnaires completed at each time point
| Questionnaire | Type of measure | Time point |
| The Habitual Index of Negative Thinking | Primary outcome measure | Every time point |
| Self-Critical Rumination Scale | Primary outcome measure | Every time point |
| Work and Social Adjustment Scale | Primary outcome measure | Every time point |
| Patient Health Questionnaire (PHQ-9) | Secondary outcome measure | Screening, S1, S3, S6 & follow-up |
| Generalised Anxiety Disorder (GAD-7) | Secondary outcome measure | Screening, S1, S3, S6 & follow-up |
| Rosenberg’s Self-Esteem Scale | Secondary outcome measure | Screening, S1, S3, S6 & follow-up |
| The Multi-Dimensional Perfectionism Scale | Secondary outcome measure | S1, S3, S6 & follow-up |
| Self-Compassion Scale | Process measure | S1 – S6 & follow-up |
| The Emotion Regulation Questionnaire | Process measure | S1, S3, S6 & follow-up |
| Beliefs about Emotions scale | Process measure | S1, S3, S6 & follow-up |
| The Forms of Self-Criticizing/Attacking and Self-Reassuring Scale | To aid formulation | S1 only |
| The Functions of Self-Criticizing/Attacking Scale | To aid formulation | S1 only |
Notes: S1: session 1; S3: session 3; S6: session 6
Appendix 5. Study questionnaires
- The Habitual Index of Negative Thinking
Occasionally we think about ourselves. Such thoughts may be positive, but may also be negative. In this study we are interested in negative thoughts you may have about yourself. Please indicate how much you agree or disagree with the following statements.
| 1. | Thinking negatively about myself is something…
I do frequently |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 2. | Thinking negatively about myself is something…
I do automatically |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 3. | Thinking negatively about myself is something…
I do unintentionally |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 4. | Thinking negatively about myself is something…
That feels sort of natural to me |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 5. | Thinking negatively about myself is something…
I do without further thinking |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 6. | Thinking negatively about myself is something…
That would require mental effort to leave |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 7. | Thinking negatively about myself is something…
I do every day |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 8. | Thinking negatively about myself is something…
I start doing before I realize I’m doing it |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 9. | Thinking negatively about myself is something…
I would find it hard not to do |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 10. | Thinking negatively about myself is something…
I do not do on purpose |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 11. | Thinking negatively about myself is something…
That’s typically “me” |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
| 12. | Thinking negatively about myself is something…
I have been doing for a long time |
1 | Strongly agree |
| 2 | Agree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Disagree | ||
| 5 | Strongly Disagree |
- Self-Critical Rumination Scale
|
My attention is often focused on aspects of myself that I’m ashamed of | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
| 2. | I always seem to be rehashing in my mind stupid things that I’ve said or done | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
| 3. | Sometimes it’s hard for me to shut off critical thoughts about myself | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
| 4. | I can’t stop thinking about how I should have acted differently in certain situations | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
| 5. | I spend a lot of time thinking about how ashamed I am of some of my personal habits | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
| 6. | I criticize myself a lot for how I act around other people | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
| 7. | I wish I spent less time criticizing myself | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
| 8. | I often worry about all of the mistakes I have made | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
| 9. | I spend a lot of time wishing I were different | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
| 10. | I often berate myself for not being as productive as I should be | 1 | Strongly disagree |
| 2 | Disagree | ||
| 3 | Neither agree nor disagree | ||
| 4 | Agree | ||
| 5 | Strongly agree |
C. Work and Social Adjustment Scale
People’s problems sometimes affect their ability to do certain day-to-day tasks in their lives. To rate your problems look at each section and determine on the scale provided how much your problem impairs your ability to carry out the activity. This assessment is not intended to be a diagnosis. If you are concerned about your results in any way, please speak with a qualified health professional.

If you’re retired or choose not to have a job for reasons unrelated to your problem, tick here
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||||||
| Not at all | Slightly | Definitely | Markedly | Very severely | ||||||||||
| 1. | Because of my self-critical thinking my ability to work is impaired.
‘0’ means ‘not at all impaired’ and ‘8’ means very severely impaired to the point I can’t work. |
| 2. | Because of my self-critical thinking my home management (cleaning, tidying, shopping, cooking, looking after home or children, paying bills) is impaired. |
| 3. | Because of my self-critical thinking my social leisure activities (with other people e.g. parties, bars, clubs, outings, visits, dating, home entertaining) are impaired. |
| 4. | Because of my self-critical thinking my private leisure activities (done alone, such as reading, gardening, collecting, sewing, walking alone) are impaired. |
| 5. | Because of my self-critical thinking my ability to form and maintain close relationships with others, including those I live with, is impaired. |
D. Patient Health Questionnaire (PHQ-9)
Over the last 2 weeks, how often have you been bothered by any of the following problems?
| 1. | Little interest or pleasure in doing things | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 2. | Feeling down, depressed or hopeless | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 3. | Trouble falling or staying asleep, or sleeping too much | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 4. | Feeling tired or having little energy | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 5. | Poor appetite or overeating | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 6. | Feeling bad about yourself – or that you are a failure or have let yourself or your family down | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 7. | Trouble concentrating on things, such as reading the newspaper or watching television | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 8. | Moving or speaking so slowly that other people could have noticed. Or the opposite – being so fidgety or restless that you have been moving around a lot more than usual | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 9. | Thoughts that you would be better off dead, or hurting yourself | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
E. Generalised Anxiety Disorder (GAD-7)
Over the last 2 weeks, how often have you been bothered by any of the following problems?
| 1. | Feeling nervous, anxious or on edge | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 2. | Not being able to stop or control worrying | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 3. | Worrying too much about different things | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 4. | Trouble relaxing | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 5. | Being so restless that it is hard to sit still | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 6. | Becoming easily annoyed or irritable | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
| 7. | Feeling afraid as if something awful might happen | 0 | Not at all |
| 1 | Several days | ||
| 2 | More than half the days | ||
| 3 | Nearly every day |
F. Rosenberg’s Self-Esteem Scale
Below is a list of statements dealing with your general feelings about yourself. If you strongly agree, circle 1. If you agree with the statement, circle 2. If you disagree, circle 3. If you strongly disagree, circle 4.
| 1. | I feel that I’m a person of worth, at least on an equal plane with others. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
| 2. | I feel that I have a number of good qualities. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
| 3. | All in all, I am inclined to feel that I am a failure. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
| 4. | I am able to do things as well as most other people. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
| 5. | I feel I do not have much to be proud of. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
| 6. | I take a positive attitude toward myself. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
| 7. | On the whole, I am satisfied with myself. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
| 8. | I wish I could have more respect for myself. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
| 9. | I certainly feel useless at times. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
| 10 | At times, I think I am no good at all. | 1 | Strongly agree |
| 2 | Agree | ||
| 3 | Disagree | ||
| 4 | Strongly Disagree |
G. The Multi-Dimensional Perfectionism Scale
| Please circle the number that best corresponds to your agreement with each statement below. Please rate how you feel now. | Strongly Strongly disagree agree | ||||
| 1. My parents set very high standards for me. | 1 | 2 | 3 | 4 | 5 |
| 2. Organisation is very important to me. | 1 | 2 | 3 | 4 | 5 |
| 3. As a child, I was punished for doing things less than perfectly. | 1 | 2 | 3 | 4 | 5 |
| If I do not set the highest standards for myself, I am likely to end up a second-rate person. | 1 | 2 | 3 | 4 | 5 |
| 5. My parents never tried to understand my mistakes. | 1 | 2 | 3 | 4 | 5 |
| 6. It is important to me that I be thoroughly competent in everything I do. | 1 | 2 | 3 | 4 | 5 |
| 7. I am a neat person. | 1 | 2 | 3 | 4 | 5 |
| 8. I try to be an organised person. | 1 | 2 | 3 | 4 | 5 |
| 9. If I fail at work / school, I am a failure as a person. | 1 | 2 | 3 | 4 | 5 |
| 10. I should be upset if I make a mistake. | 1 | 2 | 3 | 4 | 5 |
| 11. My parents wanted me to be the best at everything. | 1 | 2 | 3 | 4 | 5 |
| 12. I set higher goals than most people. | 1 | 2 | 3 | 4 | 5 |
| If someone does a task at work / school better than I, then I feel like I failed the whole task. | 1 | 2 | 3 | 4 | 5 |
| 14. If I fail partly, it is as bad as being a complete failure. | 1 | 2 | 3 | 4 | 5 |
| Only outstanding performance is good enough in my family. | 1 | 2 | 3 | 4 | 5 |
| 16. I am very good at focusing my efforts on attaining a goal. | 1 | 2 | 3 | 4 | 5 |
| Even when I do something very carefully, I often feel that it is not quite right. | 1 | 2 | 3 | 4 | 5 |
| 18. I hate being less than best at things. | 1 | 2 | 3 | 4 | 5 |
| 19. I have extremely high goals. | 1 | 2 | 3 | 4 | 5 |
| 20. My parents have expected excellence from me. | 1 | 2 | 3 | 4 | 5 |
| 21. People will probably think less of me if I make a mistake. | 1 | 2 | 3 | 4 | 5 |
| 22. I never felt like I could meet my parents’ expectations. | 1 | 2 | 3 | 4 | 5 |
| 23. If I do not do as well as other people, it means I am an inferior human being. | 1 | 2 | 3 | 4 | 5 |
| 24. Other people seem to accept lower standards from themselves than I do. | 1 | 2 | 3 | 4 | 5 |
| 25. If I do not do well all the time, people will not respect me. | 1 | 2 | 3 | 4 | 5 |
| 26. My parents have always had higher expectations for my future than I have. | 1 | 2 | 3 | 4 | 5 |
| 27. I try to be a neat person. | 1 | 2 | 3 | 4 | 5 |
| 28. I usually have doubts about the simple everyday things I do. | 1 | 2 | 3 | 4 | 5 |
| 29. Neatness is very important to me. | 1 | 2 | 3 | 4 | 5 |
| 30. I expect higher performance in my daily tasks than most people. | 1 | 2 | 3 | 4 | 5 |
| 31. I am an organised person. | 1 | 2 | 3 | 4 | 5 |
| 32. I tend to get behind in my work because I repeat things over and over. | 1 | 2 | 3 | 4 | 5 |
| 33. It takes me a long time to do something ‘right’. | 1 | 2 | 3 | 4 | 5 |
| 34. The fewer mistakes I make, the more people will like me. | 1 | 2 | 3 | 4 | 5 |
| 35. I never felt like I could meet my parents’ standards. | 1 | 2 | 3 | 4 | 5 |
H. Self-Compassion Scale
HOW I TYPICALLY ACT TOWARDS MYSELF IN DIFFICULT TIMES
Please read each statement carefully before answering. To the left of each item, indicate how often you behave in the stated manner, using the following scale:
Almost never Almost always
1 2 3 4 5
1. I’m disapproving and judgmental about my own flaws and inadequacies.
2. When I’m feeling down I tend to obsess and fixate on everything that’s wrong.
3. When things are going badly for me, I see the difficulties as part of life that everyone goes through.
4. When I think about my inadequacies, it tends to make me feel more separate and cut off from the rest of the world.
5. I try to be loving towards myself when I’m feeling emotional pain.
6. When I fail at something important to me I become consumed by feelings of inadequacy.
7. When I’m down and out, I remind myself that there are lots of other people in the world feeling like I am.
8. When times are really difficult, I tend to be tough on myself.
9. When something upsets me I try to keep my emotions in balance.
10. When I feel inadequate in some way, I try to remind myself that feelings of inadequacy are shared by most people.
11. I’m intolerant and impatient towards those aspects of my personality I don’t like.
12. When I’m going through a very hard time, I give myself the caring and tenderness I need.
13. When I’m feeling down, I tend to feel like most other people are probably happier than I am.
14. When something painful happens I try to take a balanced view of the situation.
15. I try to see my failings as part of the human condition.
16. When I see aspects of myself that I don’t like, I get down on myself.
17. When I fail at something important to me I try to keep things in perspective.
18. When I’m really struggling, I tend to feel like other people must be having an easier time of it.
19. I’m kind to myself when I’m experiencing suffering.
20. When something upsets me I get carried away with my feelings.
21. I can be a bit cold-hearted towards myself when I’m experiencing suffering.
22. When I’m feeling down I try to approach my feelings with curiosity and openness.
23. I’m tolerant of my own flaws and inadequacies.
24. When something painful happens I tend to blow the incident out of proportion.
25. When I fail at something that’s important to me, I tend to feel alone in my failure.
26. I try to be understanding and patient towards those aspects of my personality I don’t like.
I. The Emotion Regulation Questionnaire
We would like to ask you some questions about your emotional life, in particular, how you control (that is, regulate and manage) your emotions. The questions below involve two distinct aspects of your emotional life. One is your emotional experience, or what you feel like inside. The other is your emotional expression, or how you show your emotions in the way you talk, gesture, or behave. Although some of the following questions may seem similar to one another, they differ in important ways. For each item, please answer using the following scale:
1—————–2——————3——————4——————5——————6——————7
strongly neutral strongly
disagree agree
| Rating (0-7) | |
| 1. When I want to feel more positive emotion (such as joy or amusement), I change what I’m thinking about. | |
| 2. I keep my emotions to myself. | |
| 3. When I want to feel less negative emotion (such as sadness or anger), I change what I’m thinking about. | |
| 4. When I am feeling positive emotions, I am careful not to express them. | |
| 5. When I’m faced with a stressful situation, I make myself think about it in a way that helps me stay calm. | |
| 6. I control my emotions by not expressing them. | |
| 7. When I want to feel more positive emotion, I change the way I’m thinking about the situation. | |
| 8. I control my emotions by changing the way I think about the situation I’m in. | |
| 9. When I am feeling negative emotions, I make sure not to express them. | |
| 10. When I want to feel less negative emotion, I change the way I’m thinking about the situation. |
J. Beliefs about Emotions scale
Please tick the column that best describes how you think. Please note that because people are different, there are no right or wrong answers to these statements. To decide whether a given answer is typical of your way of looking at things, simply keep in mind how you think most of the time.
| Totally agree | Agree very much | Agree slightly | Neutral | Disagree slightly | Disagree very much | Totally disagree | |
| It is a sign of weakness if I have miserable thoughts. | |||||||
| If I have difficulties I should not admit them to others. | |||||||
| If I lose control of my emotions in front of others, they will think less of me. | |||||||
| I should be able to control my emotions. | |||||||
| If I am having difficulties it is important to put on a brave face. | |||||||
| If I show signs of weakness then others will reject me. | |||||||
| I should not let myself give in to negative feelings. | |||||||
| I should be able to cope with difficulties on my own without turning to others for support. | |||||||
| To be acceptable to others, I must keep any difficulties or negative feelings to myself. | |||||||
| It is stupid to have miserable thoughts. | |||||||
| It would be a sign of weakness to show my emotions in public. | |||||||
| Others expect me to always be in control of my emotions. |
K. The Forms of Self-Criticizing/Attacking and Self-Reassuring Scale
When things go wrong in our lives or don’t work out as we hoped, and we feel we could have done better, we sometimes have negative and self-critical thoughts and feelings. These may take the form of feeling worthless, useless or inferior etc. However, people can also try to be supportive of them selves. Below are a series of thoughts and feelings that people sometimes have. Read each statement carefully and circle the number that best describes how much each statement is true for you.
Please use the scale below.
| 1. | When things go wrong for me…
I am easily disappointed with myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 2. | When things go wrong for me…
There is a part of me that puts me down |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 3. | When things go wrong for me…
I am able to remind myself of positive things about myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 4. | When things go wrong for me…
I find it difficult to control my anger and frustration at myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 5. | When things go wrong for me…
I find it easy to forgive myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 6. | When things go wrong for me…
There is a part of me that feels I am not good enough |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 7. | When things go wrong for me…
I feel beaten down by my own self-critical thoughts |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 8. | When things go wrong for me…
I still like being me |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 9. | When things go wrong for me…
I have become so angry with myself that I want to hurt or injure myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 10. | When things go wrong for me…
I have a sense of disgust with myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 11. | When things go wrong for me…
I can still feel loveable and acceptable |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 12. | When things go wrong for me…
I stop caring about myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 13. | When things go wrong for me…
I find it easy to like myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 14. | When things go wrong for me…
I remember and dwell on my failings |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 15. | When things go wrong for me…
I call myself names |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 16. | When things go wrong for me…
I am gentle and supportive with myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 17. | When things go wrong for me…
I can’t accept failures and setbacks without feeling inadequate |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 18. | When things go wrong for me…
I think I deserve me self-criticism |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 19. | When things go wrong for me…
I am able to care and look after myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 20. | When things go wrong for me…
There is a part of me that wants to get rid of the bits I don’t like |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 21. | When things go wrong for me…
I encourage myself for the future |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 22. | When things go wrong for me…
I do not like being me |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
L. The Functions of Self-Criticizing/Attacking Scale
There can be many reasons why people become critical and angry with themselves. Read each statement carefully and circle the number that best describes how much each statement is true for you.
Use the scale below.
| 1. | I get critical and angry with myself…
To make sure I keep up my standards |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 2. | I get critical and angry with myself…
To stop myself being happy |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 3. | I get critical and angry with myself…
To show I care about my mistakes |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 4. | I get critical and angry with myself…
Because if I punish myself I feel better |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 5. | I get critical and angry with myself…
To stop me being lazy |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 6. | I get critical and angry with myself…
To harm part of myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 7. | I get critical and angry with myself…
To keep myself in check |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 8. | I get critical and angry with myself…
To punish myself for my mistakes |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 9. | I get critical and angry with myself…
To cope with feelings of disgust with myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 10. | I get critical and angry with myself…
To take revenge on part of myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 11. | I get critical and angry with myself…
To stop my getting overconfident |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 12. | I get critical and angry with myself…
To stop me being angry at others |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 13. | I get critical and angry with myself…
To destroy a part of me |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 14. | I get critical and angry with myself…
To make me concentrate |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 15. | I get critical and angry with myself…
To gain reassurance from others |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 16. | I get critical and angry with myself…
To stop me becoming arrogant |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 17. | I get critical and angry with myself…
To prevent future embarrassments |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 18. | I get critical and angry with myself…
To remind me of my past failures |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 19. | I get critical and angry with myself…
To keep me from making minor mistakes |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 20. | I get critical and angry with myself…
To remind me of my responsibilities |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
| 21. | I get critical and angry with myself…
To get at the things I hate in myself |
0 | Not at all like me |
| 1 | A little bit like me | ||
| 2 | Moderately like me | ||
| 3 | Quite a bit like me | ||
| 4 | Extremely like me |
If you can think of any other reasons why you become self-critical please write them in the space below:
………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………….
Appendix 6. Participant feedback questionnaire
| Question | Type of response | Scoring |
|
Open-ended | |
|
Options: 0; 10; 20; 30; 40; 50; 60; 70; 80; 90; 100% | |
|
Open-ended | |
|
Options: Not at all; a little; somewhat; quite a lot; very much; N/A – didn’t try at all | Not at all = 0; a little = 1; somewhat = 2; quite a lot = 3; very much = 4 |
|
Open-ended | |
|
Open-ended | |
|
Open-ended | |
|
Options: Strongly disagree; Disagree; Neither agree or disagree; Agree; Strongly agree | Strongly disagree = 1; Disagree =2; Neither agree or disagree = 3; Agree = 4; Strongly agree = 5 |
|
Options: Strongly disagree; Disagree; Neither agree or disagree; Agree; Strongly agree | As above |
|
Options: Strongly disagree; Disagree; Neither agree or disagree; Agree; Strongly agree | As above |
|
Options: Strongly disagree; Disagree; Neither agree or disagree; Agree; Strongly agree | As above |
|
Options: Strongly disagree; Disagree; Neither agree or disagree; Agree; Strongly agree | As above |
|
Open-ended |
Appendix 7. Measure of frequencies of use of specific intervention techniques since end of treatment collected at two-month follow-up appointment
| Not at all | Once or twice | Several times | Once a week | Several times a week | Every day | |
| Scoring | 0 | 1 | 2 | 3 | 4 | 5 |
| Compassionate reframe | ||||||
| Decentring | ||||||
| Changing the context | ||||||
| Abdominal breathing | ||||||
| Progressive muscle relaxation | ||||||
| Compassionate other imagery | ||||||
| Compassionate self imagery | ||||||
| Guiding your day with self-compassion | ||||||
| Loving-kindness meditation | ||||||
| Compassionate behaviours |
Appendix 8. Flow chart to show participants’ journey and involvement of therapists
Interested individuals responded to online advertisement

Email response with link to screening questionnaires sent by Therapist 1








Interested individuals completed screening questionnaires
Therapist 1 (n=34) & Therapist 2 (n=34) contacted those who completed questionnaires to either offer screening or signpost to alternative sources of support
Therapist 1 (n=24) & Therapist 2 (n=23) completed telephone screening to assess eligibility
Telephone screenings discussed with study supervisor
Individuals informed of decision through email or telephone contact
Eligible individuals who wished to take part completed Participant Consent Form and received treatment straight away or put on waiting list
Started treatment with either Therapist 1 or Therapist 2
Therapist 2
n=12
n=12
Participants completed weekly questionnaires and face-to-face appointments across 5 weeks
n=11
n=12
Participants completed online questionnaires 2-months post-intervention
n=12
n=11
Participants attended 2-month telephone follow-up appointment
n=10
n=12
Therapist 1 (author)
First face-to-face appointment: Qualitative interview for analysis by therapist 2 for her thesis, followed by Session 1 of intervention for current study
Qualitative analysis for thesis of therapist 2 (n=24)
Feasibility, acceptability & quantitative pre and post outcome data (n=23)

Analysis of
Appendix 9. Online recruitment advertisement
| Self-criticism: Development of a new intervention
Advertisement for use for recruitment of volunteers for study ref: [PNM/14/15-33], approved by the Psychiatry, Nursing and Midwifery Research Ethics Sub-Committee (PNM RESC). This project contributes to the College’s role in conducting research, and teaching research methods. You are under no obligation to reply to this email, however if you choose to, participation in this research is voluntary and you may withdraw at any time. ARE YOU VERY SELF-CRITICAL?
Would you like to take part in research into a new method aimed at reducing unhelpful self-criticism? We are carrying out a research study, where you could be invited to take part in an interview/assessment plus 5 individual sessions to help you develop strategies to reduce self-critical thinking. The first session will last 1-2 hours and subsequent sessions will take 1 hour. The sessions will take place on a weekly basis, unless you would prefer otherwise. We plan for the sessions to be held at the Denmark Hill, the Strand or Guy’s campus of King’s College London, however, alternative arrangements may be possible depending on what is convenient for you. In order to check whether you are suitable for the study, you would be asked to complete some questionnaires and talk to one of us on the telephone. You could be eligible to take part in our study, if you:
For further information about the study (with no obligation to take part), please contact alexandra rose (alexandra.a.rose@kcl.ac.uk) or ruth mcintyre (ruth.r.mcintyre@kcl.ac.uk). |
Appendix 10. Participant information sheet
INFORMATION SHEET FOR PARTICIPANTS
YOU WILL BE GIVEN A COPY OF THIS INFORMATION SHEET
Self-criticism: Development of a new intervention
We would like to invite you to participate in this postgraduate research project. You should only participate if you want to; choosing not to take part will not disadvantage you in any way. Before you decide whether you want to take part, it is important for you to understand why the research is being done and what your participation will involve. Please take time to read the following information carefully and discuss it with others if you wish. Ask us if there is anything that is not clear or if you would like more information.
What is the purpose of this study?
This study is investigating a new intervention for students who are looking for help to reduce their self-critical thinking. This study is part of a doctoral research project. This study is being conducted by Alexandra Rose and Ruth McIntyre, clinical psychologists in training at the Institute of Psychiatry, Psychology and Neuroscience, together with Dr Katharine Rimes and Dr Patrick Smith, honorary consultant clinical psychologists and senior lecturers at King’s College London.
Why have I been invited to take part?
We are recruiting KCL undergraduate and postgraduate students who have respondent to advertisements for the study.
Am I eligible to take part?
You may be eligible to take part if you tend to be self-critical and you want help to reduce this, because it causes you distress or other problems. This will be assessed by your scores on questionnaires and a discussion with one of the researchers over the telephone.
Self-criticism can affect various different areas of our lives including work, studying and relationships. Participants must be aged at least 18 years of age and be an undergraduate or postgraduate student at KCL. There are certain reasons why people may not be suitable. This includes having current problems that would interfere with one’s ability to benefit from such help, for example, substance dependence and anorexia nervosa. If you are not eligible to take part in the study the researcher will explain this to you at the time of the telephone screening.
If you take part in this study you would need to be available to take part in an in-depth interview and 5 individual sessions.
Do I have to take part?
It is up to you whether or not you take part. If you do decide to take part, you will be asked to sign a consent form. Having signed the consent form, you are still free to withdraw your participation without giving a reason, up until the point the data has been analysed. For information from your interview, this will be a month after the interview, whereas the questionnaire data can be withdrawn up until December 2015. A decision to withdraw, or a decision not to take part, will not affect any other care that you may receive, such as through the NHS or the student support services.
What will happen to me if I take part?
The first thing you will be asked to do will be to take part in a brief telephone screening; prior to the telephone call you will be emailed a link to complete some brief questionnaires about your style of thinking and the impact this has on your life. The purpose of this is to determine whether this intervention would be helpful for you. Your answers to these questionnaires will be scored and based on this you will be invited to take part in the intervention. During the telephone screening you will have the opportunity to ask any questions that you might have about the project. We will also ask for you to provide your GP details. Your GP will only be contacted if the clinicians feel concerned that there is a risk to your safety or the safety of other people. The brief telephone screening may take up to 45 minutes.
Once you are invited to take part in the intervention, you will be asked to sign and return the consent form. Prior to the first session you will be emailed a link to a set of questions, which you will be asked to complete in your own time. During the first session you come to you will be asked a number of questions about your experiences of self-criticism. This will help to inform subsequent sessions. The content of this session will be audio-recorded and transcribed onto a password-protected computer. It will also be anonymised and combined with other people’s responses to help us better understand the experience of self-criticism. The focus of the five subsequent sessions will be on developing strategies to better manage your self-critical thoughts drawing on techniques from self-compassion training. These sessions will also be audio-recorded. You will also be asked to complete a series of questionnaires at different time-points during the intervention, including mid-way, at the end and two months after the intervention.
New intervention to reduce self-criticism
The help provided will take your preferences into account and will draw on elements of cognitive behaviour therapy and self-compassion training.
Being self-compassionate means adopting the qualities of kindness, warmth, strength and non-judgement and directing them towards the self. Self-compassion is a skill that we can develop further.
You will be taught a range of exercises and strategies to reduce your self-critical thinking and increase your self-compassion. These sessions will help you to become aware of and to understand why your self-criticism has developed. You will be given information about the benefits of self-compassion.
The benefit of having individual sessions is that the intervention will be targeted to suit your individual needs. You will also be able to troubleshoot any difficulties you may encounter in a safe and confidential space. You will only be encouraged to use methods that feel ok for you. As this is a new intervention we are keen to receive feedback at all stages.
Data and audio-recording
In order to be able to analyse the data from the study, we will ask for your consent for members of the research team to have access to your questionnaire responses. All of your completed questionnaire responses will be anonymised by labelling them with a number rather than with your name. They will be stored securely at Kings College London. We will also ask your permission to audio record the sessions, for supervision purposes and so that we can check that the sessions were being run according to the research protocol. The audio-recording of the first interview session will be transcribed and stored electronically on a password-protected computer. All audio-recordings will be deleted once they have been transcribed or used for supervision purposes. Interview content will be analysed to identify any common themes that emerge. In reporting the findings, quotes may be used, however, these written/spoken reports will not contain any identifying information about those who take part.
Confidentiality – who will know that I am taking part in this study?
All information relating to you participating in this study will be securely stored, either on a password-protected computer at King’s College London, or locked in a filing cabinet. No completed questionnaires will be labelled using your name or any other identifiable information. Instead, each questionnaire will be labelled with a unique identification number. The only people who will have access to your data from the study will be the research team.
Other forms of help for self-criticism
We ask that you do not have any other form of help (e.g. counselling) for your self-criticism during the time that you are attending the intervention sessions, otherwise we will not be able to tell whether there has been any impact of the help that we have provided. If you take part, you can continue taking any medication. If you are taking antidepressant medication, you need to have been on a stable dose for at least three months before starting this study.
You are free to choose not to participate in this research trial. If you do not want to participate in the trial, you will continue to be able to seek other available help.
What are the possible risks or disadvantages of taking part?
As with any form of help that focuses on psychological issues, you may sometimes feel emotionally distressed. The clinicians have experience in delivering one-to-one therapy and will help you to develop methods for managing distress.
A possible disadvantage is the inconvenience of the questionnaires and interviews. These have been kept to a minimum and will be done in a way that is as convenient for you as possible. It is also possible, though unlikely, that you might experience some emotional distress as a result of completing some of the questionnaires. Support will be available to you in this event.
What are the potential benefits of taking part?
If you decide to take part than you will be offered help for negative effects of self-criticism. Whilst we expect this form of help to be of benefit to you, we cannot guarantee this. If of interest, we can send you a copy of the final report on the research study.
What will happen to the results of the study?
The results of the study will be written up as part of the researchers’ theses, and submitted to a peer reviewed journal and a conference.
What will happen if I don’t want to carry on with the study?
You are able to withdraw from treatment or the study at any stage. You may decide that you would like to continue with the intervention, but not complete the questionnaires and interviews. If you withdraw from treatment, with your permission, we would also like you to complete post-intervention questionnaires despite you not completing the individual sessions. However, you will retain the right not to do this if you so choose.
If you withdraw from the study, you may also request that your interview data is removed from this study; this will be possible until one month after the interview.
Ethical Approval
This study has been approved by King’s College London Psychiatry, Nursing and Midwifery Research Ethics Subcommittee (PNM RESC) – Reference number [PNM/14/15-33]
For further information
If you have any questions or would like any further information about the study, please do not hesitate to contact Alexandra Rose (Alexandra.a.rose@kcl.ac.uk), Ruth McIntyre (ruth.r.mcintyre@kcl.ac.uk), Dr Katharine Rimes (katharine.rimes@kcl.ac.uk) or Patrick Smith (Patrick.Smith@kcl.ac.uk). If this study has harmed you in any way, you should contact any of the above-named people. If you remain unhappy, you have the right to complain to King’s College London about any aspects of the way you have been approached or treated during the course of this study.
It is up to you to decide whether to take part or not. If you decide to take part you are still free to withdraw from the study at any time and without giving a reason.
Thank you for taking time to read this information pack.
Summary
- Participation is voluntary. You have the right to choose not to participate, or to stop participating in the trial at any point and without consequence.
- All the information you provide throughout the trial will be completely confidential. However, if a member of the team is given reason to believe that your health may be at risk or you may harm yourself or others, we may contact your GP or other relevant parties.
- This information sheet is for you to keep. If you decide to participate, you will also be provided with a copy of the signed consent form.
- For any further information, please contact Alexandra Rose (Alexandra.a.rose@kcl.ac.uk), Ruth McIntyre (ruth.r.mcintyre@kcl.ac.uk) or Dr Katharine Rimes (katharine.rimes@kcl.ac.uk).
Appendix 11. Participant consent form
CONSENT FORM FOR PARTICIPANTS IN RESEARCH STUDIES
Please complete this form after you have read the Information Sheet and/or listened to an explanation about the research.
Title of Study: Self-criticism: Development of a new intervention
Please tick or initial
King’s College Research Ethics Committee Ref: PNM/14/15-33
Thank you for considering taking part in this research. The person organising the research must explain the project to you before you agree to take part. If you have any questions arising from the Information Sheet or explanation already given to you, please ask the researcher before you decide whether to join in. You will be given a copy of this Consent Form to keep and refer to at any time.
I confirm that I understand that by ticking/initialling each box I am consenting to take part in the study. I understand that it will be assumed that unticked/initialled boxes mean that I DO NOT consent to take part in the study.
*I confirm that I have read and understood the information sheet dated for the above study. I have had the opportunity to consider the information and asked questions which have been answered satisfactorily.
*I understand that my participation is voluntary and that I am free to withdraw at any time without giving any reason. Furthermore, I understand that I will be able to withdraw my questionnaire data up to December 2015 and my interview data up to one month after the interview.
*I consent to the processing of my personal information for the purposes explained to me. I understand that such information will be handled in accordance with the terms of the UK Data Protection Act 1998.
*I understand that my information may be subject to review by responsible individuals from the College for monitoring and audit purposes.
I understand that confidentiality and anonymity will be maintained and it will not be possible to identify me in any publications
I agree that the research team may use my data for future research and understand that any such use of identifiable data would be reviewed and approved by a research ethics committee. (In such cases, as with this project, data would/would not be identifiable in any report).
I understand that the information I have submitted will be published as a report and I could ask to receive a copy if I wish.
I consent to my interview being audio/video recorded.
__________________ __________________ _________________
Name of Participant Date Signature
Appendix 12. Session protocols
| Session content | |
| Session 1 |
|
| Session 2
|
|
| Session 3
|
|
| Session 4
|
|
| Session 5
|
|
| Session 6
|
|
| Follow-up appointment |
|
Appendix 13. Blank participant formulation worksheet
| Early Influences | Key fears
External fears
Internal fears
|
Coping strategies | Intended consequence | Unintended consequences |
Appendix 14. Participant booklets
A. Session 1 Booklet
What is self-critical thinking?
Someone who is self-critical will tend to judge themselves in a very harsh way. They might become disappointed with themselves when they make mistakes, or spend lots of time going over things they don’t like about themselves in their head. Although we all have self-critical thoughts from time to time, someone who is very self-critical has such thoughts more often and their view of themselves may be particularly negative.
Can self-criticism ever be helpful?
Some people think that self-critical thinking is useful, for example, if we make a mistake a self-critical thought might help us to identify what we could do differently in the future. However, it would be more accurate to call this ‘self-corrective’ thinking, rather than self-critical thinking. Self-corrective thinking tends to be very focused on a specific event or issue rather than being about our characteristics or general worth as a person. Self-corrective thinking tends to focus on a specific mistake or issue that needs to be addressed, while maintaining an overall view of oneself as an acceptable person with strengths and weaknesses.
Are there more unhelpful forms of self-criticism than others?
For highly self-critical individuals, self-critical thinking is often triggered by a specific event but quickly becomes generalised to overall characteristics. For example, we may quickly conclude from a single mistake that “I am a failure” or “I am not good enough” and feel low or ashamed. Sometimes self-critical thinking is associated with self-hatred and self-contempt e.g. “I am a disgusting person”. Self-critical thinking may also focus on one’s ability to cope with stress e.g. “I should be able to cope with this” which may be related to frustration. It might lead us to behave in impulsive or unhelpful ways in order to deal with the distressing feelings. These forms of self-criticism can have particularly negative consequences for us.
What are some common triggers of self-criticism?
Self-critical thinking can affect many different areas of our lives, or may be focused on one or two particular areas. Here are some common areas in which self-criticism could develop:
- Work / Study
- Housework / Cleaning / Tidiness
- Close relationships (e.g. partner, family, friends)
- Eating / weight / shape
- Appearance / Grooming / personal hygiene
- Sport / Health & Fitness
What does self-criticism look like?
Self-criticism doesn’t just affect the way we think. Self-critical thoughts can also have a negative impact on the way we feel and the way we behave. See below for common examples of each
Thoughts
- “I’m stupid”
- “Mistakes are not acceptable”
- “I should have tried harder”
- “I’m useless”
- “If I don’t achieve 100%, then I have failed”
- “Everyone will think badly of me”
- “No-one will ever want to be my partner”
- “I’ve messed things up again”
- “I’m not good enough”
Feelings that may arise with self-criticism
- Bad about oneself
- Ashamed
- Low in mood
- Anxious about not getting things right
- Tired
- Worried about details
- Guilty
- Angry at mistakes
- Upset at self
- Critical of other people too
- Difficulty feeling calm and content
Behaviours that may occur in relation to self-criticism
- Put in extra effort or time trying to reach high standards
- Try to do too many things at once
- Give up trying
- Avoid situations where one might be judged
- Find it difficult to let others help
- Struggle to make decisions
- Compare self to others
- Do things at the last minute (procrastinate)
- Always keep busy
- Seek reassurance from others
- Repeatedly check for mistakes
- Over-analyse things that have happened
- Reduce social activities
- Criticise others, perhaps about characteristics we don’t accept in ourselves
- Hide feelings from others
- Overuse certain coping strategies to block out difficult feelings (e.g. food, alcohol, drugs, internet use, exercise, shopping, helping others)
Functions of self-criticism
Self-criticism often develops early in life. As a result people may believe that they deserve their self-criticism or that it’s an intrinsic part of them. They may also feel that self-criticism serves an important function for them. Here are some possible functions:
- As a warning of threat
- To push us on to self-correct, improve or achieve
- As a response to a memory
- As a habit
- To avoid aggression from others
- To criticise ourselves before others do
- To avoid rejection
- To reinforce a sense of identity as a humble and unselfish person
- To get rid of the bad or unwanted feelings inside
- To bring down positive feelings (e.g. pride) that make us feel uncomfortable
- As a response to errors or losses driven by panic or frustration
- To stop us from doing things that could result in harm
- To protect someone else
All of these functions of self-criticism can be understood as an understandable and protective response of the self to something that is perceived as a threat, from either an internal or external source.
Self-criticism as a habit
As self-criticism is often acquired early in life it can easily become a habit. If others have been critical of us in the past we may take their views as accurate without questioning them. We just go along with their criticisms of us, as one often does as a child, and never stop to think if they are accurate or reasonable. Over time, we internalise the criticism of the other person, so that in their absence, we learn to criticise ourselves.
A habit is formed when people repeatedly respond in a particular way to specific contexts with the aim of achieving a specific goal. Contexts can include physical settings (e.g. classroom), time of day, the people, behaviours performed prior to (e.g. making a mistake) and internal states (e.g. feeling anxious). For example, a person may respond with self-criticism when they feel anxious about making a mistake while doing their homework.
For a habit to be learnt the context and the response need to occur close together in time. Over time, a habit is laid down in our memory system so that we always respond in the same way to the same context. When there are few alternative options available to us the habit is more likely to become ingrained. In this way, the habit (e.g. self-criticism) can occur without any direct intention or without requiring any particular effort. The habit may be furthered strengthened when someone sees it to serve a positive function.
Where has self-criticism come from?
Old and new brain
Paul Gilbert, a leading figure in the field of compassion-focused therapy, makes a distinction between our ‘old brain-mind’ and our ‘new brain-mind’. Our brains are the source of our many different feelings, desires, fantasies and motivations. The basic emotions of anger, anxiety and pleasure have been part of the human experience for a very long time. They are even ones that we share with other species on our planet. Our emotions serve a dual purpose, to enrich our lives through the experience of pleasure and joy and to protect us when we experience threat. In modern times, these emotions can bring challenges for us, when they interfere in our daily lives. For example, people may experience anxiety when there is no apparent threat. Our ways of relating socially have also been part of the human experience for a very long time. Looking to chimpanzees, a close relative of ours, we can see how they too engage in social activities and form relationships. As with our emotions, this social way of relating has both positive and negative elements. For example, we form close bonds and care for children and each other but we also fight and challenge each other for social position and resources. Both our basic emotions and social-relating styles are part of our ‘old-brain/mind’ characteristics. They are ancient motives that guide us in our lives. We do not choose this way of being but rather it has been decided for us by evolution.
As humans, we are also very different to other species on our planet and have characteristics that represent a ‘new-brain/mind’. These characteristics are due to changes in our physical brain, which has evolved to become bigger overall and in certain important areas. For example, the size of the front part of our brain has increased, which has enabled us to have an imagination and to empathise with how others are thinking and feeling. We also have more capacity to think, learn, use symbols and language and sustain activity, requiring multiple competencies for hours at a time. The modern brain also has the ability to be creative. It is because of our new brains that we have witnessed advances in agriculture, science, technology, medicine, culture and psychology.
The problem is when ‘old-brain/mind’ emotions, desires and motives clash with ‘new-brain/mind’ characteristics. For example, our desire for pleasure may lead us to imagine how our lives might be, free from tiredness, self-doubt, irritability and so on. When we compare our fantasies to the reality of our lives we may be sorely disappointed. If we hear a noise during the night and imagine there is a burglar in our house, we may also feel fear and anxiety, whether there is a burglar there or not. Our ‘new-brain/mind’ also means that we can ruminate and mull over what has happened to us, which may then drive us into a spiral of depression and anxiety.
From Gilbert*
The three emotion-regulation systems in the brain
Gilbert outlines three of the major types of emotion regulation systems. These are designed to interact and counterbalance each other. The three systems are outlined below, and the diagram shows how they interact with each other.
- Threat-protection system: to keep us protected and safe
- Drive-motivation system: to help us feel driven, excited, activated
- Contentment-soothing-safeness system: to help us feel content, at peace, connected with others
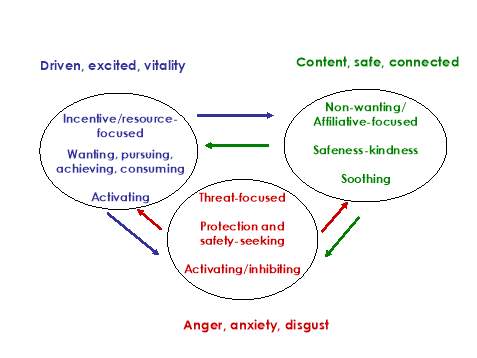
From Gilbert*
1) Threat-protection system
This system is like an alarm system to detect and pick up on threats quickly. When threat has been detected, this system is triggered. This then leads to feelings such as anxiety, anger and disgust, which alert us to the threat. In turn this then urges us to do something to protect ourselves or others, and leads to behaviours to address the threat e.g. avoiding danger.
This system is designed to protect us, and in many contexts the emotion and associated behaviour may be helpful. For example, if we detect danger when walking alone late at night, feeling anxious and compelled to run to a safer place might be an appropriate way of keeping safe. Or if we have an impending exam, some degree of anxiety can help motivate us to revise. The brain region called the amygdala is involved, which is capable of very quick, pre-conscious detection of threat. The stress hormone cortisol is released, which helps us to respond to threat.
However, sometimes this system can cause problems, if it is too easily triggered or difficult to turn off. Sometimes cortisol production can be over- or under-active. We may become anxious, or angry, or feel that we should avoid situations, even though those emotions and behaviours are not helpful in that particular context. For example, if we feel too anxious, we might find it difficult to sleep or concentrate before an exam.
2) Drive-motivation system
This system helps us to feel sufficiently activated to achieve things and get things done. It leads to our desires by driving us to behave in way to satisfy these. We are motivated by things such as food, sex, friendships, comfort, status and recognition. When these positive things happen, this system gives us a sense of pleasure. Dopamine is one brain chemical involved in this system.
However, if we are over-busy, or push ourselves too hard, this system can get exhausted and we can start to lose feelings of motivation and interest. This can happen if we have been over-using this system for a prolonged period. Or if the demands of the situation seem overwhelming, or we face the loss of a significant relationship or life goal, we can lose motivation and energy.
3) Contentment-soothing-safeness system
This system regulates the experience of contentment, things being sufficient for us. These peaceful and calm pleasant sensations are very different to the more excited feelings associated with striving and succeeding in the drive-motivation system. This system can help to restore our balance. This system is evolutionarily important because it underlies our attachments to other people. These connections are often important for our survival, especially if we are very young or old or ill or vulnerable in some way. At first our mother soothes us, but over time we can learn ways of soothing ourselves and others. Humans value and look for kindness in our partners because kindness from others this is a key way of feeling safe and content. Kindness also underlies trust, which is another fundamental aspect of feeling safe in our connections with other people. This system is related to brain chemicals such as endorphins and a hormone called oxytocin.
Self-criticism and the three emotion-regulation systems
When self-critical thinking has become a problem, typically the threat-protection system and the drive-motivation system are highly activated, but the contentment-soothing-safeness system is under-used. So the overall system becomes unbalanced. According to Gilbert*, someone who is very self-critical may find it difficult to access feelings of (self) warmth, compassion and reassurance.
For example, although most people get stressed by exams, for someone who is very self-critical and believes that anything less than top exam marks would mean failure or being not good enough as a person, this will be especially threatening. Someone who is very self-critical might also tend to worry a lot about a future exam, and/or ruminate about past mistakes.
Despite what some may believe, self-criticism does not help us to feel motivated or enthusiastic – instead it just adds to the sense of threat. Similarly, although worrying or ruminating might sometimes give a sense of control with regards to pre-empting future problems or understanding past issues, these processes also keep the threat-protection system active. So these responses have a high cost.
We may have learnt the sense of purpose or achievement of striving towards our goals. This is not necessarily problematic unless we rely so much on this strategy that we find it difficult to switch out of Achievement / Striving mode. For example, someone may criticise themselves and then feel guilty if they spend any time where there is not some kind of ‘achievement’ at the end. Relaxing, having fun, and spending ‘unproductive’ time with friends or family, can get neglected.
Sometimes if we are not feeling enough sense of achievement in one area (e.g. work), we have learnt that focusing on another area of achievement can give us the positive feeling. For example, we might find that striving towards being very physically fit, or keeping our possessions very tidy and in order, or keeping to a strict form of diet, or having an immaculate clothes / make-up, or looking after other people, or maintaining standards in another area, helps us to feel better about ourselves or more in control. These are not necessarily problematic but if someone tends to experience lots of self-critical thoughts, we have to be careful that we do not pursue them inflexibly or spend too much time on them. Otherwise, we can lose sight of what is really more important to us, in terms of our values and health, in the long-term.
Striving towards achievement in these ways can sometimes make us feel temporarily better but does not address an underlying sense of not being ‘good enough’, so this remains vulnerable to getting triggered off again. Although achievement is an important part of feeling good about ourselves, no-one can be successful all the time. When things go wrong or we make mistakes or fail, often the most effective way of coping is to be able to be kind and supportive to ourselves, and / or to seek support and connection with others. When we are feeling calmer, we are in a better position to take stock, look at the bigger picture and make a wise decision about where to focus our efforts in the future.
Some of us are not confident in our ability to soothe ourselves or seek care and connection and support from others. This is usually because past circumstances have not provided that opportunity. However, it is never too late to learn ways to be more self-compassionate and kind towards ourselves and to develop and maintain warm and supportive relationships with other people.
Someone who is very self-critical may experience a sense of resistance when they hear this. For example, it may sound self-indulgent or unnecessary. This is not self-indulgence, it is about treating the mind wisely with what it need to function at its best. Developing the flexibility to switch between these systems will result in better health and functioning than spending too much time with the Threat system activated.
Effects of self-criticism
Our thoughts and images can have a very powerful effect on our brains and bodily systems. Imagine that you are very hungry and you sit down to eat your favourite dinner. What is the effect of this on your body? When you see the food in front of you, an area of your brain is stimulated, which sends messages to your body so your mouth will start to produce saliva and your stomach will start to produce digestive juices. This has the effect of making your mouth water and your stomach rumble. Imagine now that you are really hungry but you have no food left in your house, so you close your eyes and imagine your favourite dinner. What is the effect of this on your body? The same as what happened when you actually had your favourite dinner in front of you. Your mouth starts to water and your stomach starts to rumble, even though this time you are only imagining your favourite food. The image in your mind is so powerful that it can stimulate the same physiological systems in your body.
Now think about what happens in your body when you are under threat. For example, if you are being bullied emotionally or physically by another person, or are being criticised or having your mistakes pointed out to you in a harsh manner, you are likely to feel threatened. Being threatened stimulates the stress system and your body produces the stress hormone cortisol. This can cause physical symptoms such as muscle tension, nausea and sweaty palms. It also makes people feel anxious and upset. This happens because the threat emotion systems in the brain have been triggered. If the threat persists, for example, if you are constantly being bullied every day, you may become very distressed, unhappy and depressed. This makes a lot of sense. The very same effect can also occur in response to threatening thoughts and images in our minds. So, if you are constantly putting yourself down or being self-critical, your stress system will be activated triggering the emotional systems in your brain that make you feel anxious, angry and down. It will also have the effect of curbing positive feelings. Thus, for those people who tend to be self-critical, their threat systems are frequently being stimulated and they understandably feel more anxious, angry or depressed.
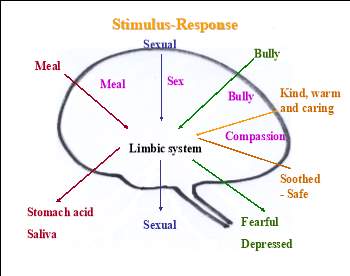
From Gilbert *
Below are some further examples of possible effects of self-criticism:
- Feeling anxious, angry and down
- Physical exhaustion from constantly feeling under threat
- Feeling disgusted and ashamed of oneself
- Rarely feeling safe, happy or relaxed
- Setting unattainable standards for oneself
- Comparing oneself to others in a negative manner
- Never feeling satisfied with oneself
- Ruminating on perceived flaws and mistakes
- Difficulties forming and maintaining relationships
- Psychological problems such as depression, eating disorders and self-harm
Starting to become aware of self-critical thinking (self-criticism monitoring)
When someone experiences lots of self-critical thoughts, this way of thinking will start to become a habit. This means that the self-critical thoughts will become so automatic that we might not even realise that we are having them. Greater awareness of a habit is the first step in changing it. The Self-Critical Monitoring Form on the next page will help you do this. We will use this form to write down the following:
Context and triggers: Are there particular contexts where self-critical thinking is more likely, for example certain times of day or situations? Is it more likely after certain triggers such as having made a mistake or having said something you regretted or feeling evaluated or criticised by others?
Feelings: How were you feeling before the self-criticism started?
Duration: How long did the self-critical thinking last?
Content: What were you thinking about? Try and write down exactly what the self-critical thoughts were.
Consequences: What were the consequences of the self-criticism? Self-critical thoughts can have a negative impact on our mood and on our behaviour. How did you feel after the self-critical thoughts occurred? Did you do anything in response to these thoughts?
What stopped the self-criticism? Did you try anything to stop the self-criticism? Was this useful? Or did it stop due to external factors?
Self-critical monitoring form
Please could you fill in details about TWO examples of you being self-critical. There are no right or wrong answers – it’s just a way of gathering helpful information about your thinking.
| What happened just before the self-criticism started? | How did you feel before? | Duration | What were you thinking about? | What were the consequences of the self-criticism – on mood and actions? | What stopped the self-criticism? What did you do to try to stop it? Was it useful? |
Understanding your self-criticism
Once you have become more aware of the self-critical thinking, it can be useful to summarise what you noticed by filling in the Self-Criticism Summary form on the next page. A couple of examples are also included on the following pages.
| Self-Criticism Summary
Themes Common examples When does it happen? What stops / interrupts? Aims of the self-criticism (e.g. how is it intended to help keep you safe?) Aims and possible advantages: Disadvantages: Can the self-criticism lead to things being avoided? How did self-criticism develop into a habit? Any times or situations when you are less self-critical? What helps? |
Matt’s example
Themes
Common examples
When does it happen?
What stops / interrupts?
Aims of the self-criticism (e.g. how is it intended to help keep you safe?) Aims and possible advantages:
Disadvantages:
Can the self-criticism lead to things being avoided?
How did self-criticism develop into a habit?
Any times or situations when you are less self-critical? What helps?
|
Sophie’s example
| Self-Criticism Summary
Themes
Common examples
When does it happen?
What stops / interrupts?
Aims of the self-criticism (e.g. how is it intended to help keep you safe?) Aims and possible advantages:
Disadvantages:
Can the self-criticism lead to things being avoided?
How did self-criticism develop into a habit?
Any times or situations when you are less self-critical? What helps?
|
Acknowledgement:
The content of this booklet drew on the following resources:
Books
*Gilbert, P. (2009). The Compassionate Mind. Constable: London.
*Gilbert, P. (2010). Compassion Focused Therapy. Routledge: London, New York.
*Gilbert, P. (2010). An Introduction to the Theory and Practice of Compassion Focused Therapy and
Compassionate Mind Training for Shame Based Difficulties. Downloaded from
www.compassionatemind.co.uk/resources/training_materials.htm
*Gilbert, P. & Choden, P. (2014). Mindful Compassion: how the science of compassion can help you understand your emotions, live in the present, and connect deeply with others. New Harbinger Publications, Inc: Canada.
Welford, M. (2012). The Compassionate Mind Approach To Building Your Self-Confidence.
Robinson: London.
Articles
*Gilbert, P. (2009). Introducing compassion-focused therapy. Advances in Psychiatric Treatment, 15, 199-208.
*Gilbert, P. (2010). An introduction to compassion focused therapy in cognitive behavior therapy. International Journal of Cognitive Therapy, 3, 97-112.
B Session 2 Booklet
Self-compassion as an alternative to self-criticism
In order to change a habit it is helpful to have an alternative option to turn to and cultivate. The self-compassion approach helps us to recognise our self-critical tendencies, respond to them with understanding and kindness, while moving us towards more helpful self-correction. Compassionate self-correction focuses on the desire to improve ourselves or our situation. It is focused on the future and is given in the context of encouragement, support and kindness. It is in contrast to self-criticism focuses on the desire to attack or punish ourselves and is often focused on past mistakes. Self-criticism is usually in the context of anger, annoyance and frustration (Gilbert, 2010, P. 106).
Self-compassion helps people to recognise self-criticism as a component of the threat system. It also helps people to become aware of the emotions associated with self-criticism and to understand the function, possible origins and the reasons why one might agree with their self-criticism. Self-compassion can help people to move out of the threat system by evaluating the legitimacy of the self-critical self-attacks.
The Teacher Metaphor
One way to think about the differences between the two approaches is to consider the ‘teacher metaphor’ in relation to a child who is struggling in class. Imagine one teacher who is encouraging and supportive of the child and rewards the child for what s/he has done well. How might this child feel? Now imagine another teacher who is critical and harsh with the child and punishes the child for the mistakes s/he has made. How might this child feel? Which style of teaching is likely to develop the child’s confidence, enthusiasm and happiness? Which way would you prefer to treat yourself?
What is self-compassion?
Self-compassion involves directing compassion, which may be defined “as a sensitivity to the suffering of self and others with a deep commitment to try to relieve it” (Dalai Lama), towards ourselves. In this way, we learn to move out of the threat-focused system and into the soothing/compassion-focused system. This can help us to balance our emotions and enable us to experience a much greater sense of wellbeing.
Gilbert* has distinguished between compassionate attributes and compassionate skills. By developing these attributes and skills, we can helpfully manage the negative impact self-criticism has on our thoughts, feelings and behaviours.
Compassionate Attributes (adapted from Welford* P. 73-76):
Warmth, gentleness and kindness
All of the attributes listed below are “experienced in the context of emotional warmth” (Welford*, P 73).
- Care for well-being
This means having the intention, motivation and commitment to care about the welfare of yourself and of other people.
- Sensitivity to distress
This involves being aware of when you or others are experiencing distressing or difficult emotions, and being open to such experiences.
- Sympathy
This means being emotionally touched by what is happening in our lives or other people’s lives and connecting with whatever pain is present.
- Empathy
This means having an understanding of our minds and the minds of others, and being able to consider things from various perspectives. It allows us to think about what one might need.
- Acceptance and non-judgement of emotions
This means recognising the complexity of human experience and doing our best not to judge or condemn what happens in our lives as well as our thoughts, feelings and behaviours.
- Distress tolerance
This means being able to tolerate or feel difficult emotions, memories or situations even when we would rather avoid them.
Compassionate Skills:
As well as the compassionate attributes, Gilbert* has also identified a number of skills – these are things that we can learn to do:
- Compassionate attention
This involves noticing when things have gone well, or if things don’t go as we would like, learning from this, rather than dwelling on the negative.
- Compassionate reasoning
This involves bringing balance to our thinking by considering all the evidence and reducing any unhelpful thinking patterns that we might use.
- Compassionate sensations
This involves noticing feelings in our bodies when we focus on being compassionate.
- Compassionate imagery
This involves developing images in our mind that are “supportive, understanding, kind and encouraging” (Welford*, P. 76) and using these images to help us.
- Compassionate behaviour
This involves behaving in a caring and supportive manner that, at times, may require courage.
- Compassionate emotions
This involves developing an emotional tone that emphasises support, warmth and kindness.
Common fears & blocks to self-compassion
Below are some common fears and blocks to compassion that Gilbert* has identified:
- Feeling like you don’t deserve it.
- Thinking that self-compassion is self-indulgent or selfish.
- Seeing self-compassion as a weakness.
- Feeling sad and tearful when you try to be self-compassionate.
- Having unpleasant associations with kindness.
- Feeling angry and thinking that compassion won’t help you.
- Thinking that compassion means you have to be a “nice person” all the time.
- Thinking that compassion allows you to go easy on yourself.
When we are trying to change an old habit and introduce a new one, things can sometimes get in the way of us making the change. It is normal to face some barriers along the way. Sometimes we can be actively resistant to change and other times the new way of doing things just seems a bit strange. This may be true even if we believe that the change we are hoping to make is an important one. It is not unusual to feel a sense of resistance or discomfort about the idea of treating oneself with self-compassion. For example, we may have thoughts that we don’t deserve it, or that we shouldn’t have to do that or that it’s ‘wet’ or weak. It may sound impossible. We may have concerns that it will make us too complacent, but self-compassion includes acknowledging mistakes in a constructive way. We can worry that being self-compassionate will make us selfish. However, it is often more difficult to care for others well and be accepting of them if we are treating ourselves harshly. People often report that when they are kinder to themselves, they feel more positively towards other people too.
People who are not self-critical often automatically treat themselves kindly without even thinking about it – it has become a habit in the same way that self-critical thinking has become a habit for others. We can all learn to be more self-compassionate but it takes practice. It can be helpful to think about it in terms of your physical health. If you hurt your arm in an accident and suspected you had pulled a muscle, you wouldn’t tell yourself you don’t deserve for it to get better. Instead, you would take yourself to the doctor and do the recommended physiotherapy exercises to build your arms strength back up again. It might take some time and effort but you know that it will be worth it in the end. The same is true when we have been hurt internally by our own self-critical thinking. Once, you have developed the skills of self-compassion you can then decide if it is a helpful approach for you or not.
Dealing with Mistakes and Failure
Sometimes people who are highly self-critical might worry about what will happen if they do not criticise themselves strongly if they make mistakes or fail. For example, they may be concerned that they will become arrogant, selfish, lazy or uncontrolled. However, there are ways of dealing with mistakes and failure in a compassionate way that allows for self-correction and self-improvement without being so hard on ourselves. Differences between compassionate self-correction and fear-based self-criticism are shown in the table below.
| Compassionate self-correction | Fear-based self-criticism |
|
|
(Adapted from Gilbert, 2010, p. 106)
It is compassionate to take ourselves seriously and acknowledge our feelings of fear, anger and shame. It’s not so much whether we have any of these feelings but rather how we relate to them and what we do about them. For example, if you have a fear of going outside, it might feel nice to stay indoors and watch television, but this will not help you in the long run. Compassion helps us to develop the courage to face our fears whatever they might be.
Helpful questions to learn more about your potential barriers to self-compassion
As you practice engaging in a more compassionate way of thinking, notice if there are any barriers stopping you. Here are some questions you might ask yourself as you try to understand these more:
- Did anything go through your mind that made you want to stop?
- Did you think you weren’t doing the exercise properly?
- Did you think it was pointless because it wasn’t going to help you anyway?
- Was there a voice in your head saying you don’t deserve kindness?
- Did your emotions become too intense?
- Were you feeling scared or vulnerable?
- Did you start to feel sad or lonely?
- Were you feeling angry?
- Did any feelings of shame come up for you?
- How was your body feeling as you were doing the exercise?
- Did you have difficulty finding a soothing breath?
- Did you become dizzy or shaky?
- Did you feel really tired?
Self-compassionate thought record
Compassionate thinking and reasoning is an important skill to develop. Our brains have evolved in such a way that our anxieties and fears often control how we think about certain things. This is understandable as at even the slightest sign of threat our minds step in to protect us. This, however, can be unnecessary and may have the unfortunate effect of making us feel anxious, depressed, angry and paranoid. One helpful thing to bear in mind is that no thought or feeling that you have has not already been experienced by another human being.
The purpose of completing a self-compassionate thought record is, therefore, to help you to identify a more balanced and helpful way of thinking about a situation. Why we do this is because we know that generating alternatives can help us to flourish, grow and develop wisdom.
Please take a look at the examples of completed thought records on the following pages. You will see that the function of the self-criticism is purely threat-focused, over-general and catastrophic e.g. avoiding losing friends or academic failure. The self-compassionate approach does not ignore the possibility that something does need to change. However, the self-compassionate approach is more specific about exactly what happened, identifying with kindness why it might have happened, and what specifically you might need to do differently in the future. Crucially, the self-compassionate approach also addresses how to deal with how you are feeling.
Here are some questions you might ask yourself as you complete your compassionate thought record:
|
| Triggering Events, Feelings or Images | Self-critical thoughts | Feelings | Compassion-focused Alternatives to Self-Critical Thoughts | Understanding and change in feelings |
| Key questions to help you identify your thoughts.
What actually happened? What was the trigger? |
What went through your mind?
What are you thinking about others, and their thoughts about you? What are you thinking about yourself, and your future?
|
What are your main feelings and emotions?
|
What would you say to a friend?
What compassionate alternatives might there be? What is the evidence for new view? (How) are these examples of compassion, care and support? Can you think these through with warmth?
|
Write down any change in your feelings.
|
| Having lunch with my friends. They were talking about their weekend plans. I was very quiet and didn’t join in the conversation. | Self-critical thoughts:
I have nothing interesting to say. I’m really boring. I seem really rude. I’m not a very good friend.
Key feared Consequences: People will think I’m rude. They will get sick of me and won’t want to be friends with me anymore. Function of the self-criticism: To try to avoid losing my friends |
Annoyed (at myself), anxious, worried, irritated
|
Compassionate alternative:
It’s ok to be quiet sometimes in conversations – they are my friends and understand when I’m not feeling chatty. Sometimes other people are quiet and I don’t think badly of them. I had a busy morning and was still thinking about things that had been going on. It’s understandable then that I was quiet. The self-criticism is just my threat-system talking Any compassionate actions needed? (If so, what?) I feel better about this but if the thoughts come back I can remind myself that my friends accept me whether I’m chatty or quieter. Now I can focus on addressing what happened this morning rather worrying about what my friends think of me** Function of the self-compassionate approach: To address my concerns about what other people think of me in a kind and balanced way, and identify anything I need to do to feel better |
I feel less annoyed and irritated. I feel more understanding of why I might have been quiet. My anxiety has reduced. |
**It’s ok to have thoughts about how you come across to other people – we all do – but we must try to deal with these thoughts kindly and think about both sides rather than just being focused on the threat. Another time the conclusion in this example might have been that the person does need to join in more, e.g. if this is a repeated pattern of behaviour and they’re not joining in out of fear of what others think. If that was the case the person would need to come up with a self-compassionate understanding of the avoidant behaviour and how to deal with it in a compassionate way.
| Triggering Events, Feelings or Images | Self-critical thoughts | Feelings | Compassion-focused Alternatives to Self-Critical Thoughts | Understanding and change in feelings |
| Key questions to help you identify your thoughts.
What actually happened? What was the trigger? |
What went through your mind?
What are you thinking about others, and their thoughts about you? What are you thinking about yourself, and your future?
|
What are your main feelings and emotions?
|
What would you say to a friend?
What compassionate alternatives might there be? What is the evidence for new view? (How) are these examples of compassion, care and support? Can you think these through with warmth?
|
Write down any change in your feelings.
|
| I logged on to look at my mark for my last essay. I got 56%. | Self-critical thoughts:
It’s not good enough. I didn’t work hard enough. I’m stupid. I’m useless.
Key feared Consequences: If I don’t work hard enough I might fail my course. Function of the self-criticism: To try to avoid academic failure. |
Anger, annoyed, upset, disappointed, sad
|
Compassionate alternative:
A friend might remind me that although I rushed the essay I did work hard on it. I tried my best. It was a topic I find quite difficult. My tutor’s comments have some useful pointers for next time. Next time I could spend more time planning the structure. Or I could ask someone to read through it. It’s only one essay and I have done well on other essays. My grade doesn’t mean I’m stupid. Any compassionate actions needed? (If so, what?) I know what I’m going to do next time – allow more time on essays on this topic and get more help. No need to go over this any more so now I am just going to call a friend and talk about other things.
Function of the self-compassionate approach: To help identify specific things that will support me achieving my academic potential, plus anything I need to do to feel better now. |
I still feel a bit disappointed but I’m not so angry and annoyed at myself. |
| Triggering Events, Feelings or Images | Self-critical thoughts | Feelings | Compassion-focused Alternatives to Self-Critical Thoughts | Understanding and change in feelings |
| Key questions to help you identify your thoughts.
What actually happened? What was the trigger? |
What went through your mind?
What are you thinking about others, and their thoughts about you? What are you thinking about yourself, and your future?
|
What are your main feelings and emotions?
|
What would you say to a friend?
What compassionate alternatives might there be? What is the evidence for new view? (How) are these examples of compassion, care and support? Can you think these through with warmth?
|
Write down any change in your feelings.
|
| Seeing someone really attractive at Uni, on the street or watching television | Self-critical thoughts:
I’m really ugly. I have a weird body. Maybe there is no point trying to meet a partner.
Key feared Consequences: Nobody will ever be attracted to me so I will end up alone. Function of the self-criticism: To try to protect me from the pain of rejection. To try to motivate me to try to improve my appearance. |
Shame, sadness, hopeless, anxiety
|
Compassionate alternative:
Lots of people have concerns about their appearance; magazines and television make it seem like everyone should look a certain way. It’s not surprising I’d compare myself to others and then feel bad about myself. It would be better for me to accept myself as I am. Plus, I’m not completely ugly, I’ve been told that that I have a nice eyes and a pretty smile. Even if I don’t meet someone romantically my friends and family will still love me so I won’t be alone. Any compassionate actions needed? (If so, what?) I can increase the chances of meeting someone by being proactive about dating rather than avoiding it. This may take some time (for anyone!) so I need to be very self-compassionate if there are unsuccessful dates before I finally meet a potential partner
Function of the self-compassionate approach: To help me maximise my chances of meeting a partner |
Calmer, more accepting and more hopeful |
Blank copy – Thought record from Gilbert*
| Triggering Events, Feelings or Images | Self-critical thoughts | Feelings | Compassion-focused Alternatives to Self-Critical Thoughts | Understanding and change in feelings |
| Key questions to help you identify your thoughts.
What actually happened? What was the trigger? |
What went through your mind?
What are you thinking about others, and their thoughts about you? What are you thinking about yourself, and your future?
|
What are your main feelings and emotions?
|
What would you say to a friend?
What compassionate alternatives might there be? What is the evidence for new view? (How) are these examples of compassion, care and support? Can you think these through with warmth?
|
Write down any change in your feelings.
|
| Self-critical thoughts:
Key feared consequences:
Function of the self-criticism: |
Compassionate alternative:
Any compassionate actions needed? (If so, what?)
Function of the self-compassionate approach: |
Acknowledgement:
The content of this booklet drew on the following resources:
Books
*Gilbert, P. (2009). The Compassionate Mind. Constable: London.
*Gilbert, P. (2010). Compassion Focused Therapy. Routledge: London, New York.
*Gilbert, P. (2010). An Introduction to the Theory and Practice of Compassion Focused Therapy and
Compassionate Mind Training for Shame Based Difficulties. Downloaded from
www.compassionatemind.co.uk/resources/training_materials.htm
*Gilbert, P. & Choden, P. (2014). Mindful Compassion: how the science of compassion can help you understand your emotions, live in the present, and connect deeply with others. New Harbinger Publications, Inc: Canada.
Welford, M. (2012). The Compassionate Mind Approach To Building Your Self-Confidence.
Robinson: London.
Articles
*Gilbert, P. (2009). Introducing compassion-focused therapy. Advances in Psychiatric Treatment, 15, 199-208.
*Gilbert, P. (2010). An introduction to compassion focused therapy in cognitive behavior therapy. International Journal of Cognitive Therapy, 3, 97-112.
Appendix 13. Participant booklets
C. Session 3 Booklet
Compassionate alternatives to self-criticism
In order to turn self-compassion into a new habit we have to practice it as much as we can. Once you have practiced the Self-Compassionate Thought Record a number of times, try focusing on these key columns.
| Self-critical thoughts | Compassion-focused Alternatives to Self-Critical Thoughts | Any compassionate actions needed? (If so, what?) |
| What went through your mind?
What are you thinking about others, and their thoughts about you? What are you thinking about yourself, and your future?
|
What would you say to a friend?
What compassionate alternatives might there be? What is the evidence for new view? (How) are these examples of compassion, care and support? Can you think these through with warmth?
|
|
| Self-critical thoughts: | Compassionate alternative: |
Decentre: Change how you relate to the self-critical thoughts
Self-critical thoughts may pop into your head even if you have made a decision not to elaborate on them or develop them further. We cannot control the thoughts that pop into our head, only what we do next.
Alternatives to getting caught up in the content of overthinking:
|
Change the context
You may be more likely to be self-critical in certain situations. Changing aspects of the context could help reduce excessive self-critical thinking. Different strategies work for different people and you may need to try a few things before finding what is most effective. There are some examples listed below but you may find it helpful to talk to your therapist about your own situations.
Examples of changing the context to reduce self-critical thinking
| Situation where self-critical thinking is more likely to occur | Examples of changes to the situation |
| “Before I get up I lie in bed over-thinking things; especially at the weekend” | Getting up straight away. Some people find it can help to have a specific activity to get up for e.g. exercise class , meeting friend for breakfast. |
| “When I’m in the shower or travelling to or from Uni / work” | Listening to cheerful music or interesting radio programme or podcast. |
| “When I get home in evening, I’m tired and collapse in front of tv but often end up going over things that have happened that day, over-analysing what people might have thought of me or things I should have done differently” | Getting on with preparing dinner instead, or watching something that you have recorded / on internet that you particularly enjoy, or doing some yoga or a relaxation exercise (see later in booklet), or another absorbing activity such as phoning friend. |
| “When I’m alone at home. This happens particularly at the weekend which I try to keep free for studying. I don’t actually end up studying all weekend but then miss out on seeing other people or doing fun things”. | Planning social and enjoyable activities at the weekend too, as well as specific times for studying if needed. |
| “At the gym. I don’t really enjoy the gym anyway but want to be healthy”. | Going to a different gym or going with a friend or a different time of day. Switching to a different form of exercise where you can relate to other people in a more positive way (e.g. team sport, exercise class that’s not competitive) or exercising on your own (e.g. walking, running, swimming). |
| “Talking to my Mum. It’s important to me that I do speak to her once a week but I always feel self-critical afterwards” | Phoning at a different time of day when you’ll be busy afterwards or not on your own. Having a planned activity to do straight afterwards – something that will absorb your attention. |
Change your Physiology: Dampen down the Threat System
Self-critical people often have difficulty fully relaxing. Dampening down the Threat system can not only make you feel calmer and more relaxed, it can also have a positive impact on your thinking style. You will probably find it easier to access more balanced ways of relating to yourself and the situation.
There are a wide range of relaxation exercises – here are a couple of examples:
Controlled abdominal breathing (adapted from http://psychology.tools/relaxation.html)
|
Progressive Muscle Relaxation
Progressive muscle relaxation (PMR) is a technique that was developed by Dr. Edmund Jacobson in the 1920s. Jacobson highlighted that anxiety and stress lead to muscle tension, which then further increases feelings of anxiety. On the other hand, when the body is relaxed there is less muscle tension, leading to less anxiety.
Muscle tension is usually an automatic process and therefore not something we tend to notice. The aim of PMR is to help you identify tension in your body and your muscles, and ultimately become more relaxed.
There are a number of physical changes and sensations that occur in the body when we are stressed or anxious, including:
- Increased blood flow to the muscles
- Tight muscles
- Rapid and shallow breathing
- Increased heart rate
- Slow digestive functioning
PMR can counter these physical changes to achieve a “relaxation response” by calming your body. When relaxed, your breathing becomes slower, and your heart rate and blood pressure decrease. When your muscles are relaxed, they do not need as much oxygen as when they are tense. This causes redirection of blood flow from the tense muscles to other areas of the body, which then reduces a lot of the unpleasant physical sensations associated with anxiety.
How to do Progressive Muscle Relaxation?
PMR involves tensing and relaxing various muscle groups in your body in a systematic way.
Progressive Muscle Relaxation Exercise for 16 Muscle Groups
If you would like to try this, you could choose 1-2 times during your day when you can spend 15-30 minutes alone, uninterrupted and in a quiet room. PMR can be done sitting or lying down – whatever is most comfortable.
Before you begin, try some deep breathing; inhale slowly and deeply through your nose and exhale through your mouth. Then repeat this as many times as feels comfortable.
After you have done some deep breathing tense each of the muscles in the following muscle groups for about 7-10 seconds (or what feels comfortable), release the muscles, and then concentrate on the pleasant sensations of relaxation for the about 20-30 seconds. You can repeat the same muscle group and then go on to the next muscle group once the previous group feels completely relaxed.
Muscle Groups to Use
|
Below are some example PMR audio-recordings:
http://services.unimelb.edu.au/__data/assets/mp3_file/0003/965442/PMR.mp3
http://www.mentalhealth.org.uk/help-information/podcasts/progressive-relaxation-sleep/
Compassionate imagery
One technique that can be used to develop self-compassion is imagery. The purpose of imagery is to stimulate positive feelings and to help you feel soothed. It also has a positive effect on our neuro-physiology by developing our soothing system.
In session 1 we described the effects of self-criticism. We described our thoughts and images can have a very powerful effect on our brains and bodily systems.
We described that if we are criticised by another person for a mistake we have made, we are likely to feel threatened. Being threatened stimulates the stress system and your body produces the stress hormone cortisol. This can cause physical symptoms such as muscle tension, nausea and sweaty palms. It also makes people feel anxious and upset. This happens because the threat emotion systems in the brain have been triggered. If the threat persists, for example, if you are constantly being bullied every day, you may become very distressed, unhappy and depressed.
We then said that the same effect can also occur in response to threatening thoughts and images in our minds. So, if you are constantly being hard on yourself or being self-critical, your stress system will be activated triggering the emotional systems in your brain that make you feel low, anxious, or even angry. It will also have the effect of curbing positive feelings. Thus, for those people who tend to be self-critical, their threat systems are frequently being stimulated and they understandably feel more anxious, angry or depressed.
However, if when we make a mistake somebody is very kind and understanding towards us, this will help reduce feelings of stress or anxiety. Therefore in the same way learning to generate compassionate images can help us feel calm, safe and soothed when we feel threatened. Also, by thinking about what you want from your compassionate image it starts the “begins the process of gearing your mind to what you really need” (Gilbert & Choden, 2014, P. 242).
Varieties of compassion focused imagery
There are a huge number of varieties of compassion focused imagery. During our sessions we’re going to focus on firstly developing a compassionate image and then using this to develop a more compassionate self.
Preparing for imagery
When you start to generate a compassionate image you may notice that your mind wanders away from the image. This is totally normal and not a problem at all. If you notice that your mind has wandered, gently and kindly bring your attention back to the image. You may want to use your breath as an anchor during the practice.
You might also struggle to develop an image at all – that’s ok too, just remember it’s your intention to develop more compassion that’s important rather than the clarity of the image.
Acknowledgement:
The content of this booklet drew on the following resources:
Books
*Gilbert, P. (2009). The Compassionate Mind. Constable: London.
*Gilbert, P. (2010). Compassion Focused Therapy. Routledge: London, New York.
*Gilbert, P. (2010). An Introduction to the Theory and Practice of Compassion Focused Therapy and
Compassionate Mind Training for Shame Based Difficulties. Downloaded from
www.compassionatemind.co.uk/resources/training_materials.htm
*Gilbert, P. & Choden, P. (2014). Mindful Compassion: how the science of compassion can help you understand your emotions, live in the present, and connect deeply with others. New Harbinger Publications, Inc: Canada.
Welford, M. (2012). The Compassionate Mind Approach To Building Your Self-Confidence.
Robinson: London.
Articles
*Gilbert, P. (2009). Introducing compassion-focused therapy. Advances in Psychiatric Treatment, 15, 199-208.
*Gilbert, P. (2010). An introduction to compassion focused therapy in cognitive behavior therapy. International Journal of Cognitive Therapy, 3, 97-112.
Appendix 13. Participant booklets
D. Session 4 Booklet
Creating a compassionate image
What do we mean by a compassionate image?
The compassionate image we are going to focus on is developing a ‘compassionate other’. There are many different terms to describe the ‘compassionate other’ – for example, Lee (2005) uses the term ‘perfect nurturer’ – this means that the image is perfect for us and looks to give us precisely what we might need. Welford (2012) describes it as a ‘compassionate coach’. The term we use isn’t important, just chose wording that feels most comfortable for you.
The actual image that we develop will also be different for different people. We will invite you to create and imagine your own ideal compassionate image. Some people prefer to think about a non-human image such as images of nature e.g. sunlight, a warm sea, a tree or a mountain, or other non-human images such as an animal or an angel. Other people may prefer to imagine a humanlike being, such as a very wise person.
As Gilbert & Choden (2014) explain, importantly, this image is completely focused on you and motivated by compassion to help you. The image knows how our brains can be quite tricky and how our early experiences can shape us. It helps you to feel understood. Your image is sensitive to your needs and feelings and has a deep desire to make you feel better.
Ultimately your compassionate image really wants you to be free from suffering and to flourish in life! (Gilbert, 2010, p. 191)
The physical qualities of your compassionate image
The following questions may help you to create your compassionate image:
| How would you like your compassionate image to look/appear – visual qualities/facial expressions/colour? |
| How would you like your compassionate image to sound (e.g., voice tone)? |
| What other sensory qualities would you like to give your compassionate image? |
| How would you like your compassionate image to relate to you? |
| How would like to relate to your compassionate image? |
From Gilbert (2010, p. 190)
Qualities of your compassionate image
This exercise will help you start to build and develop your own compassionate image. It is important that you do your best to give your image specific qualities associated with compassion. These are described further below. Think of these as “superhuman” – “complete and perfect compassionate qualities that never let you down” (Gilbert, 2010, p. 188). If at any point your image seems harsh or critical towards you, then refocus on these qualities.
- A deep commitment to you – your compassionate image wants to help you manage with any difficulties that you might be experiencing, and ultimately experience more joy.
- Wisdom – your compassionate image has wisdom which comes from understanding that we have to deal with a brain that we didn’t design and early experiences that we had no choice over. Your compassionate image also knows you and your own life experiences so understands why you are the way you are.
- Strength of mind – your compassionate image can hold and contain your pain and distress. It has the confidence and the strength to do this.
- Warmth – your compassionate image expresses warmth by caring for you in a kind and gentle way.
- Non-judgemental acceptance – your compassionate image is never harsh or critical about you or your experiences, it understands and accepts who you are.
Bringing the compassionate image to mind – a summary
|
Some ways of using your compassionate image
Imagine the voice of your compassionate image
As you develop your compassionate image, you might want to first focus on how it feels that your image cares about you in a kind and unconditional way. You may then want to imagine your compassionate image looking at you with kindness and warmth and says this (or something similar) to you:
- May you be well
- May you be happy
- May you be free of suffering
Generate compassionate-focused alternatives to self-critical thoughts
You may also want to use your compassionate image to help generate compassionate alternatives in response to self-critical thoughts. For example, you can imagine what your compassionate image would say when you notice that you are being self-critical.
Compassionate other imagery longer script
Below is a copy of the script you would have gone through in your treatment session. You could use it to read through again, or record yourself saying the words onto your phone.
Sitting posture
- Begin by settling into a position that is comfortable for you – with your feet flat on the floor; if it’s ok sitting with your back supporting itself, away from the back of the chair; placing your hands on your lap; then allowing the eyes to either shut, or for your gaze to fall unfocused on the floor.
- Embodying a position of wakefulness and dignity.
- Then focus briefly on your facial expression – if you can, relax your facial muscles and then turn your mouth upwards slightly, into a slight smile – try to create a facial expression that is gentle and friendly.
Rationale
- The aim of this exercise is to develop a compassionate other image – an image that you can work with and develop with time.
- Throughout the practice we will imagine receiving love and care from our compassionate other, so try to remember that your image really wants you to be free of suffering and flourish in life.
- However, we may find it hard to develop or keep a clear image in mind, or we may find it hard to create feelings of warmth of kindness – and that’s ok – this exercise is not about visual clarity of an image, but is about developing “the wish” or the intention to be compassionate towards ourselves.
Notice the breath
- Now, when you are ready, just begin to notice your breath.
- Each in breath, as air comes into the body.
- And each out breath, as air leaves the body.
- You may want to do some deep abdominal breaths
- Or you may want to develop what is called “soothing breathing rhythm” (Gilbert*) – where you breathe slightly more slowly and deeply than normal. To do this, you may want to try breathing a little faster and the a little slower until you find a pattern or rhythm of breathing that is gentle and comfortable and gives you the feeling of slowing down.
Mind wandering
- When you start to generate a compassionate image you may notice that your mind wanders away from the image. This is totally normal and not a problem at all. If you notice that your mind has wandered, gently and kindly bring your attention back to the image.
- Or you may want to use your breath as an anchor during the practice – so if your mind wanders, gently and kindly bring your attention to your breath for a moment before returning to the image.
Compassionate other
- So now let’s begin by focusing on what your compassionate image would look like
- You may want to imagine your image coming out of a mist and then stands in front of you.
- Or you may want to imagine your image as it walks slowly towards you.
Physical qualities of the compassionate other
- What does your compassionate image look like? If they are human are they a man or a woman? Are they old or are they young? What is their facial expression like? If they are non-human what form do they take – an animal or an angel? Or an image of nature such as sunlight, a warm sea, a tree or a mountain? Or maybe a simply a bright light?
- What colours are associated with your image?
- What does your compassionate image sound like? If it was to talk with you, what would it sound like? What tone of voice would it have?
- With these questions in mind, spend a few moments imagining your compassionate other.
Specific compassionate qualities of the compassionate other
- The image is your creation and so it embodies whatever you would like from feeling cared for.
- As well as this, it’s important that you try to give your image specific qualities associated with compassion.
- Think of these as “superhuman” – “complete and perfect compassionate qualities that never let you down” (Gilbert, 2010, P. 188).
- If at any point your image seems critical, then refocus on creating these qualities.
- Imagine that your compassionate image has a deep commitment to you – it wants to help you manage with any difficulties that you might be experiencing, and ultimately experience more joy. No matter what you say or do, your image is committed to supporting you. It gives support and kindness to you always. Spend a few moments imagining this commitment your image has for you.
- Now focus on wisdom – your compassionate image has wisdom which comes from understanding that we have to deal with a brain that we didn’t design and early experiences that we had no choice over. Your image also knows us and our own life experiences so truly understands why we are the way we are. It understands your hopes and fears and offers you wisdom. Spend a few moments imagining being in the presence of this wisdom.
- Your compassionate image has strength of mind – it can hold and contain your pain and distress. It has the confidence the strength to do this. Spend a few moments imagining being with this image.
- Now focus on warmth – your compassionate image expresses warmth by caring for us in a kind and gentle way. Spend a few moments imagining the warmth and affectionate feelings while with this image.
- Finally, think about the quality of non-judgemental acceptance – your compassionate image is never harsh or critical about you or your experiences; it understands and accepts who you are. Spend a few moments imagining this.
Speaking to you
- Now, if you would like, imagine your compassionate image looking at you with warmth, understanding and kindness.
- Imagine them saying:
- May you be well
- May you be happy
- May you be free of suffering
In the last few moments, imagine that you are with your compassionate image. Imagine that your image truly wants you to be well, happy and at peace.
Then, let your compassionate image fade, and bring your attention back to your breathing. When you are ready, open your eyes, and spend a few moments bringing yourself back into the room.
Problems with Compassionate Imagery
No clear image: It is rare to be able to generate a clear, sharp image. Images are usually fleeting and impressionistic. Getting a ‘sense of’ an image is good enough. Notice if there are any other sensory qualities. The quality of the image is not important but rather the feelings associated with it. You can also have more than one image that changes over time.
Image of a known person: Images of people we know may have unwanted associations, therefore, it is more helpful to create a unique compassionate image for yourself. Your image doesn’t even have to be a person, so long as it represents the qualities of strength, warmth and wisdom.
Critical voice: Some people notice their inner critic tells them their image is “not good enough” or “this is stupid”. See if you can be mindful of this critical voice and focus on non-judgement.
Fear of Compassion: Compassion may feel frightening or be associated with other unpleasant feelings. This may be because people have had negative experiences of being cared for or of feeling warmth and kindness.
Anger/Frustration: Developing compassion for oneself can also bring up feelings of anger, fear of anger and vengeful fantasies. Being self-compassionate is not about getting rid of anger but rather learning how to cope with it. It may require courage to face up to our anger.
Self-compassionate imagery is one of many ways of reducing self-critical thinking. Sometimes we may find another strategy more helpful to help manage the self-criticism. We might describe all of these strategies being part of our ‘toolbox’, and we can pick which strategy to use in different situations.
Acknowledgement:
The content of this booklet drew on the following resources:
Books
*Gilbert, P. (2009). The Compassionate Mind. Constable: London.
*Gilbert, P. (2010). Compassion Focused Therapy. Routledge: London, New York.
*Gilbert, P. (2010). An Introduction to the Theory and Practice of Compassion Focused Therapy and
Compassionate Mind Training for Shame Based Difficulties. Downloaded from
www.compassionatemind.co.uk/resources/training_materials.htm
*Gilbert, P. & Choden, P. (2014). Mindful Compassion: how the science of compassion can help you understand your emotions, live in the present, and connect deeply with others. New Harbinger Publications, Inc: Canada.
Welford, M. (2012). The Compassionate Mind Approach To Building Your Self-Confidence.
Robinson: London.
Articles
*Gilbert, P. (2009). Introducing compassion-focused therapy. Advances in Psychiatric Treatment, 15, 199-208.
*Gilbert, P. (2010). An introduction to compassion focused therapy in cognitive behavior therapy. International Journal of Cognitive Therapy, 3, 97-112.
Other
Lee, D. A. (2005). The perfect nurturer: A model to develop a compassionate mind within the context of cognitive therapy. In Gilbert, Paul (Ed), (2005). Compassion: Conceptualisations, research and use in psychotherapy. (pp. 326-351). New York, NY, US: Routledge.
E. Session 5 Booklet
The Compassionate Self
In order to develop the compassionate self we first need to decide that this is something we want to cultivate. We then need to practice becoming this person. This is true for whatever part of the self that we want to develop. For example, if someone wants to become a musician they will practice playing an instrument or if someone wants to be a tennis player they will practice playing the game. Ask yourself, “what or who do I want to become?” The way our brains our designed, we have the potential to form many different sides or parts of the ‘self’. Developing the compassionate self can help us to recognise all these different parts and respond to them with kindness and understanding.
So far we have used the thought record and the Compassionate Other to develop compassionate thinking. This booklet describes other ways to develop the compassionate self by focusing on compassionate feelings and behaviours.
Remember the four key qualities of self-compassion are: wisdom, strength, warmth and non-judgment.
Accessing and developing the Compassionate Self
Method acting
One way to develop the compassionate self is to think about it like being an actor. In order to get into a particular role an actor needs to immerse him/herself in the way that they imagine the character thinks, feels and acts. They would try and create certain feelings, thoughts and motives within themselves. They would try to be that person. They might consider the character’s tone of voice, posture, the kinds of things they say or the way they say them. So now, imagine that the character you want to play is your ideal compassionate self. Using your ‘My Compassionate Self: A summary’ (beginning of this booklet) to remind you of the qualities you are aiming for, practice acting in this way.
Accessing and Developing your Compassionate Self
| In this exercise you are going to spend some time accessing your Compassionate Mind and working on developing your compassionate self. You will bring to mind all aspects of your compassionate self, including how you might think, feel and behave. We have seen during the past sessions that you are able to access self-compassionate responses so the Compassionate Mind is already part of you, and we are now focused on accessing it and developing it further. This may feel strange and difficult at first but it may help to think about it like ‘method acting’ – to get into a role an actor would try to immerse themselves in that role, and try and actually create the associated thoughts, feelings and behaviours within themselves, and try to be that person. I will guide you through this and prompt you to access your compassionate mind and develop your compassionate self.
Sitting posture, facial expression and breathing
Your Compassionate Self
Compassionate Qualities
My compassionate attributes
Closing
|
You can use the results of this exercise to help complete the Compassionate Self Summary sheet on the next page.
It does not matter if you feel that you have these qualities or not, just imagining that you do will help. Gilbert speaks about ‘compassion under the duvet’ and suggests that a good time practice developing your compassionate self is when you wake up in the morning. You could experiment with different times of day to work on this. All you need to do is focus on your desire to be more compassionate and remember that you do have the capacity for strength and wisdom inside you.
This summary form will help you define what your compassionate self looks like in terms of the way you think, feel and behave.
| My Compassionate Self: A summary
Compassionate attitude towards myself Compassionate thoughts and thinking styles Compassionate feelings towards myself Compassionate approach to my distress or difficult emotions My compassionate behaviours Compassionate sensations in my body |
Compassionate Feelings
Our emotions make themselves known very quickly and can seem very powerful, even making us behave in certain ways. The emotions of anger and anxiety are directly linked with the threat-protection system and although they feel very unpleasant at times, we do not wish to condemn these emotions or aim to rid ourselves of them. Instead, the compassionate approach is about approaching these emotions with an open and accepting mindset so that we may learn to tolerate and work with them. The compassionate approach to difficult feelings such as anger, anxiety and disappointment is to accept these feelings as understandable responses to something that has threatened you. These feelings are all part of the human experience and are not something that we choose to feel, however, we recognise that underneath them the self-protection system is kicking into action and doing its best to make you feel safe again.
For people who are very self-critical, developing a sense of compassion towards this side of them may bring about a realisation that this is a part of them that is really very frightened. Some people may experience a sense of loss or grief as they direct compassion towards their self-criticism. This is because self-criticism often develops in an attempt to feel loved and included and it can move us to recognise how hard this has been for us. You might feel sad as you acknowledge all the little hurts and disappointments you have experienced. If this makes it seem like it is too much to bring compassion to this part of yourself, you don’t have to give up all your self-criticism but you can set the intention of moving towards a more compassionate way of being.
| Loving-kindness practice
There is a basic Buddhist meditation that involves sending compassionate good wishes towards others and oneself. Sometimes this is known as ‘loving-kindness’ or “metta bhavana” meditation. One wishes for yourself and others to prosper and be happy. One can also extend this to all living things in steps. This has been used in a lot of research studies (see website www.compassionatemind.co.uk for details) – with good evidence of brain and other changes. Many people find that it helps them to feel more kindly towards themselves and other people. There are lots of different variations of loving-kindness meditations, many of which you can find on the Internet E.g.
There is also an app called ‘The Mindfulness App’ (£1.49 to download) which has a variety of different meditation exercises. Alternatively there is an example script below, but it is important that you adjust this so that it feels right for you. For example you may prefer to use words such as ‘peaceful and ‘happy’ instead of ‘calm and content’. May you be safe from harm May you be as strong and healthy as is possible for you May you be calm and content May I be safe from harm May I be as strong and healthy as is possible for me May I be calm and content May we be safe from harm May we be as strong and healthy as is possible for us May we be calm and content |
Compassionate Behaviour
As actions speak louder than words, to be fully compassionate you need to translate your compassionate intentions into actions. Compassionate behaviour may require considerable courage and may involve learning to resist the desires of the old-brain. For example, it may seem like we are being kind to ourselves by sitting in front of the television and eating ice-cream but this may not be the best action for us if we learn to live a sedentary and unhealthy lifestyle. Self-compassion may involve saying ‘no’ to our desires and facing the disappointment that brings. Compassionate behaviour is not about being indulgent and succumbing to all our desires and fantasies. It is about protection and doing what’s best for ourselves and others.
One way to think about compassionate behaviour is to imagine a young child who is refusing to go to bed and is demanding to watch more television. As the child becomes more and more disruptive the parents of the child may find it very hard to say ‘no’ to their child and may be tempted to give in for an easier more peaceful evening. This may be even harder if they are feeling guilty about being home late and not spending much time with their child that day. It requires a lot of courage for a parent in this type of situation to stand true to their beliefs about what is in their child’s best interests and not to act out of guilt or frustration.
In order to behave in a compassionate way we first need to recognise that there is a problem. For example, if someone is bullying you and this is causing you distress, the compassionate thing to do would be take some form of action. This may mean removing yourself from the situation or it may mean facing the bully; either way you will be addressing the problem head-on rather than avoiding it.
In the same way it takes courage to stand up to a bully in our environment, it also takes courage to recognise when you are your own bully. Consider the next few sections to be a toolbox of compassionate behaviours and techniques that may help you to stand up to your self-critic.
Remember that no-one can behave in an ideal or self-compassionate manner all the time. It is important to bring self-compassion to those times when we behave in ways that we are less than ideal!
Avoidance
Self-critical thinking can often be associated with avoidant behaviours. There are many different types of avoidance. Common examples include:
- Procrastination over work
- Avoiding social situations that make us feel anxious, e.g. being with certain people, interviews, public speaking
- Avoiding other situations that make us feel anxious
- Avoiding expressing our opinions, feelings, preferences or needs
- Avoiding making decisions or taking responsibility
Although these behaviours may make us avoid perceived threat in the short-term, they can all have longer-term disadvantages. They can also fuel further self-criticism.
Over-controlled behaviours
Some of us try to deal with perceived threat by trying hard to control things. Examples of forms of attempts to control:
- Over-planning how we will cope with situations
- Over-preparing our work
- Perfectionist behaviours in relation to work, our diet, exercise, appearance etc.
- Over-thinking situations beforehand or afterwards
Such behaviours can help us to feel safe and may be very reinforcing if they seem to help us to avoid negative situations or outcomes. However, they often have unintended consequences. For example they can be very time-consuming so we miss out on other things. They can make us inflexible which other people can find difficult. We can become irritated if other people don’t fit in with our plans. Over-thinking before a situation has happened can make us feel more anxious as we remain focused on a potential negative outcome that we are trying to avoid. Over-analysing a situation afterwards can also make us feel more anxious or low. Sometimes we try so hard that our attempts can backfire and cause new problems that we hadn’t intended!
Reducing avoidant or over-controlled behaviours
If you want to try to reduce an avoidant or over-controlled behaviour, it can be helpful to plan specify ways of testing out new ways of doing things. Some people find it helpful to do this gradually in small steps. Others prefer to throw themselves in at the deep end and be open to learning from what happens in a self-compassionate manner
Show your feelings
People who are very self-critical often report that they find it difficult to express their opinions and needs to others. Remember that you have a right to your own values, opinions and feelings. Feelings are normal and helpful, even negative or difficult ones. An important role of emotions is the signals they send to oneself and to others. Therefore, these emotions are most useful when shared with others – when they can communicate our feelings and state of mind to others. Try not to suppress or hide your feelings – let them show in a useful way. Expressing feelings to other people, whether directly or in writing tends to make us feel better.
Be assertive
- Be specific – say how your feel or what you want specifically / directly
- Work out what the issues are rather than labelling or attacking the person or oneself
- Own the problem. A problem is yours whenever you are the person whose needs are not being met. By clearly telling others “I have a problem”, you lessen the chance that they will become defensive and increase the chance of resolving the conflict.
- If requesting change, briefly describe one behaviour is troubling you, and your feelings about the behaviour and its consequences: The formula is: “I have a problem. When you [describe the behaviour], [state the consequences] and I feel [describe your feelings]. For example: “I have a problem. When you drive so fast on this winding road, you put us in danger of going over the side and I feel afraid”.
- Aim for a workable compromise – assertiveness is not about winning, you need to find a true compromise that takes both parties’ needs into consideration
- If necessary, repeat in a calm manner – this can help you from getting distracted
- Anger at our own lack of assertiveness is common. This self-directed anger can be more damaging to us than the lack of assertiveness.
Make small behaviour changes
Try out a range of new behaviours over time rather than picking one new behaviour and sticking to it rigidly. This prevents you from becoming bored as you habituate to the new behaviour. Aim to incorporate these changes into your daily life and you will be taking positive action in your life.
Compassionate health behaviours
Research has shown that doing regular exercise can have a positive effect on our mood. Exercise is associated with release of endogenous opiates, and consequently is thought to improve mood. Note that if you tend to push yourself too hard with regards to exercise e.g. exercising strenuously every day and finding it difficult to have a day off, then a more self-compassionate approach may be to reduce the amount or intensity of exercise and ensure that you have days off to allow your body time to rest and repair. Similarly, being self-compassionate means taking a balanced and self-supportive approach to other health-related behaviours such as eating, drinking, drugs and sexual health. Either extreme – excessive or over-controlled behaviours – can have unintended adverse consequences.
Guiding your day with self-compassion
Here is another exercise to help you cultivate your Compassionate Self:
| Step 1: Take a breath to settle your mind and body
Step 2: Imagine your compassionate self or compassionate ideal Step 3: With warmth, ask your compassionate self or compassionate ideal “what can I do for myself today that will make it a better day?” Step 4: Remind yourself of your self-compassionate attitudes e.g. “I treat myself with kindness and respect; I look after my own needs (physical, psychological, social, spiritual etc)” or Make a positive statement about today e.g. “I will treat myself with kindness and respect, I will attend to my own needs” Step 4: Imagine how you will feel if you do the things you brought to mind in the previous step Step 5: Take a breath and notice how you feel Step 6: Be guided by your compassionate advice |
Acknowledgement:
The content of this booklet drew on the following resources:
Books
*Gilbert, P. (2009). The Compassionate Mind. Constable: London.
*Gilbert, P. (2010). Compassion Focused Therapy. Routledge: London, New York.
*Gilbert, P. (2010). An Introduction to the Theory and Practice of Compassion Focused Therapy and
Compassionate Mind Training for Shame Based Difficulties. Downloaded from
www.compassionatemind.co.uk/resources/training_materials.htm
*Gilbert, P. & Choden, P. (2014). Mindful Compassion: how the science of compassion can help you understand your emotions, live in the present, and connect deeply with others. New Harbinger Publications, Inc: Canada.
Welford, M. (2012). The Compassionate Mind Approach To Building Your Self-Confidence.
Robinson: London.
Articles
*Gilbert, P. (2009). Introducing compassion-focused therapy. Advances in Psychiatric Treatment, 15, 199-208.
*Gilbert, P. (2010). An introduction to compassion focused therapy in cognitive behavior therapy. International Journal of Cognitive Therapy, 3, 97-112.
Appendix 15. Post-intervention ratings of how useful participants found the intervention
| Feedback question | Strongly disagree,
n (%) |
Disagree,
n (%) |
Neither agree or disagree,
n (%) |
Agree,
n (%) |
Strongly agree,
n (%) |
Mean | Standard deviation |
| The intervention was useful | 0 | 0 | 0 | 9
(42.9) |
12
(57.1) |
4.6 | 0.49 |
| The intervention helped to reduce my self-critical thinking | 0 | 0 | 2
(9.5) |
10
(47.6) |
9
(42.9) |
4.3 | 0.64 |
| The intervention helped improve my ability to cope with my self-critical thinking | 0 | 0 | 1
(4.8) |
10
(47.6) |
10
(47.6) |
4.4 | 0.58 |
| The intervention helped me to improve my self-compassion | 0 | 1
(4.8) |
3
(14.3) |
9
(42.9) |
8
(38.1) |
4.1 | 0.83 |
| My facilitator understood my needs/ difficulties | 0 | 0 | 2
(9.5) |
6
(28.6) |
13
(61.9) |
4.5 | 0.66 |
| I would recommend the intervention to other people with high levels of self-criticism | 0 | 0 | 0 | 7
(33.3) |
14
(66.6) |
4.7 | 0.47 |
Notes: participants rated their agreement on a 5-point Likert scale: strongly disagree = 1; disagree =2; neither agree or disagree = 3; agree = 4; strongly agree = 5
Appendix 16. Post-intervention ratings of how useful participants found each technique
| Technique | Not at all,
n (%) |
A little,
n (%) |
Somewhat,
n (%) |
Quite a lot,
n (%) |
Very much,
n (%) |
N/A – didn’t try at all,
n (%) |
Mean | Standard deviation |
| Compassionate reframe | 0 | 3
(14.3) |
2
(9.5) |
8
(38.1) |
8
(38.1) |
0 | 3 | 1.02 |
| Decentering | 1
(4.8) |
2
(9.5) |
2
(9.5) |
4
(19.0) |
12
(57.1) |
0 | 3.1 | 1.21 |
| Changing the context | 1
(4.8) |
4
(19.0) |
2
(9.5) |
8
(38.1) |
6
(28.6) |
0 | 2.7 | 1.21 |
| Relaxation exercises | 0 | 4
(19.0) |
9
(42.9) |
0 | 8
(38.1) |
0 | 2.6 | 1.18 |
| Compassionate other imagery | 3
(14.3) |
4
(19.0) |
3
(14.3) |
5
(23.8) |
6
(28.6) |
0 | 2.3 | 1.43 |
| Loving-kindness meditation | 0 | 3
(14.3) |
4
(19.0) |
4
(19.0) |
7
(33.3) |
3
(14.3) |
2.8 | 1.12 |
| The compassionate self | 2
(9.5) |
4
(19.0) |
2
(9.5) |
3
(14.3) |
7
(33.3) |
3
(14.3) |
2.5 | 1.46 |
| Compassionate behaviours | 1
(4.8) |
4
(19.0) |
4
(19.0) |
5
(23.8) |
4
(19.0) |
3
(14.3) |
2.4 | 1.21 |
Notes: participants rated their agreement on a 5-point Likert scale: not at all = 0; a little = 1; somewhat = 2; quite a lot = 3; very much = 4
Appendix 17. Ratings of frequency of use for each technique since end of treatment collected at follow-up appointment
| Technique | Not at all,
n (%) |
Once or twice,
n (%) |
Several times,
n (%) |
Once a week,
n (%) |
Several times a week,
n (%) |
Everyday,
n (%) |
Mean | Standard deviation |
| Compassionate reframe | 1
(4.5) |
1
(4.5) |
7
(31.8) |
3
(13.6) |
8
(36.6) |
2
(9.1) |
3 | 1.28 |
| Decentering | 4
(18.2) |
0 | 3
(13.6) |
5
(22.7) |
2
(9.1) |
8
(36.6) |
3.1 | 1.82 |
| Changing the context | 7
(31.8) |
4
(18.2) |
3
(13.6) |
2
(9.1) |
2
(9.1) |
4
(18.2) |
2 | 1.88 |
| Abdominal breathing | 5
(22.7) |
4
(18.2) |
2
(9.1) |
3
(13.6) |
6
(27.3) |
2
(9.1) |
2 | 1.88 |
| Progressive muscle relaxation | 11
(50) |
1
(4.5) |
2
(9.1) |
3
(13.6) |
3
(13.6) |
2
(9.1) |
1.6 | 1.85 |
| Compassionate other imagery | 7
(31.8) |
6
(27.3) |
4
(18.2) |
1
(4.5) |
2
(9.1) |
2
(9.1) |
1.6 | 1.61 |
| The compassionate self | 9
(40.9) |
4
(18.2) |
2
(9.1) |
2
(9.1) |
4
(18.2) |
1
(4.5) |
0.6 | 1.19 |
| Guiding your day with self-compassion | 11
(50) |
0 | 2
(9.1) |
2
(9.1) |
2
(9.1) |
5
(22.7) |
1.6 | 1.70 |
| Loving-kindness meditation | 16
(72.7) |
2
(9.1) |
3
(13.6) |
0 | 0 | 1
(4.5) |
2 | 2.12 |
| Compassionate behaviours | 7
(31.8) |
0 | 0 | 3
(13.6) |
7
(31.8) |
5
(22.7) |
2.8 | 2.01 |
Notes: participants rated their agreement on a 6-point Likert scale: not at all = 0; once or twice = 1; several times = 2; once a week = 3; several times a week = 4; every day = 5
Appendix 18. Results of independent t-tests comparing the two therapists on participant measures across time points
| Measure | Time point | t (21) | p-value |
| Habitual Index of Negative Thinking (HINT) | Screening | .24 | .81 |
| Pre-intervention | .40 | .69 | |
| Post-intervention | -.26 | .80 | |
| Follow-up | .38 | .71 | |
| Self-Critical Rumination Scale (SCRS) | Screening | -.50 | .62 |
| Pre-intervention | -1.02 | .32 | |
| Post-intervention | -1.51 | .15 | |
| Follow-up | -.50 | .62 | |
| Work and Social Adjustment Scale (WASA) | Screening | -.62 | .54 |
| Pre-intervention | -1.40 | .18 | |
| Post-intervention | -.19 | .85 | |
| Follow-up | .17 | .86 | |
| Patient Health Questionnaire (PHQ-9) | Screening | 1.64 | .12 |
| Pre-intervention | 0.04 | .96 | |
| Post-intervention | -0.05 | .96 | |
| Follow-up | 0.35 | .73 | |
| Generalised Anxiety Disorder (GAD-7) | Screening | -.83 | .42 |
| Pre-intervention | -1.04 | .31 | |
| Post-intervention | .30 | .77 | |
| Follow-up | -.84 | .41 | |
| Rosenberg’s Self-Esteem Scale (RSES) | Screening | -1.28 | .21 |
| Pre-intervention | -1.10 | .28 | |
| Post-intervention | 0.52 | .61 | |
| Rosenberg’s Self-Esteem Scale (RSES) | Follow-up | -0.03 | .98 |
| Multi-Dimensional Perfectionism Scale (MDPS) | Pre-intervention | -.23 | .82 |
| Post-intervention | -1.14 | .27 | |
| Follow-up | -.09 | .93 | |
| Self-compassion Scale (SCS) | Pre-intervention | -.01 | .99 |
| Post-intervention | .06 | .95 | |
| Follow-up | .59 | .56 | |
| Emotion Regulation Questionnaire – Regulation | Pre-intervention | -.02 | .99 |
| Post-intervention | .32 | .75 | |
| Follow-up | .38 | .71 | |
| Emotion Regulation Questionnaire – Suppression | Post-intervention | -2.18 | .04 |
| Follow-up | -1.25 | .22 | |
| Beliefs about Emotions Scale (BES) | Pre-intervention | -1.46 | .16 |
| Post-intervention | -2.25 | .04 | |
| Follow-up | -1.38 | .18 |
Appendix 19. Results of linear regressions investigating relationship between (a) length of baseline (time between screening and pre-intervention), (b) time from screening to post-intervention and (c) time from pre to post intervention and change in study measures
| Dependent variable (i) | Independent variable | F value (1, 21) | p value |
| HINT-change | Length of baseline | .02 | .90 |
| Time from screening to post-intervention | .01 | .94 | |
| Time from pre to post-intervention | .42 | .53 | |
| SCRS-change | Length of baseline | .24 | .63 |
| Time from screening to post-intervention | .13 | .72 | |
| Time from pre to post-intervention | .27 | .61 | |
| WASAS-change | Length of baseline | 3.25 | .09 |
| Time from screening to post-intervention | 2.08 | .16 | |
| Time from pre to post-intervention | 1.90 | .18 | |
| PHQ-9-change | Length of baseline | 3.02 | .10 |
| Time from screening to post-intervention | 2.80 | .11 | |
| Time from pre to post-intervention | .30 | .59 | |
| GAD-7-change | Length of baseline | .66 | .43 |
| Time from screening to post-intervention | .75 | .40 | |
| Time from pre to post-intervention | .00 | .98 | |
| RSES-change | Length of baseline | .06 | .80 |
| Time from screening to post-intervention | .04 | .85 | |
| Time from pre to post-intervention | .05 | .83 | |
| MDPS-change | Length of baseline | .20 | .66 |
| Time from screening to post-intervention | 1.15 | .30 | |
| Time from pre to post-intervention | 3.51 | .08 | |
| SCS-change | Length of baseline | .33 | .57 |
| Time from screening to post-intervention | 1.35 | .26 | |
| Time from pre to post-intervention | 2.85 | .11 | |
| ERQ-R-change | Length of baseline | 1.57 | .22 |
| Time from screening to post-intervention | 2.48 | .13 | |
| Time from pre to post-intervention | .34 | .57 | |
| ERQ-S-change | Length of baseline | .78 | .39 |
| Time from screening to post-intervention | .08 | .78 | |
| Time from pre to post-intervention | 5.02 | .04 | |
| BES-change | Length of baseline | .08 | .78 |
| Time from screening to post-intervention | .50 | .49 | |
| Time from pre to post-intervention | 1.61 | .22 |
Notes: (i) Dependent variable computed by: post-intervention scores minus pre-intervention scores; HINT: The Habitual Index of Negative Thinking; SCRS: Self-Critical Rumination Scale; WASAS: Work and Social Adjustment Scale; PHQ-9: Patient Health Questionnaire; GAD-7: Generalised Anxiety Disorder; RSES: Rosenberg Self-Esteem Scale; MDPS: Multi-Dimensional Perfectionism Scale; SCS: Self-Compassion Scale; ERQ-R: Emotion Regulation Questionnaire-Reappraisal; ERQ-S: Emotion Regulation Questionnaire-Suppression; BES: Beliefs about Emotions Scale
Appendix 20. Line graphs for secondary outcome measures (PHQ-9, GAD-7, RSES and ‘maladaptive perfectionism) at main study time points
Line graph to show mean scores for the Patient Health Questionnaire (PHQ-9) at screening, pre-intervention, post-intervention & follow-up (one standard deviation error bars)
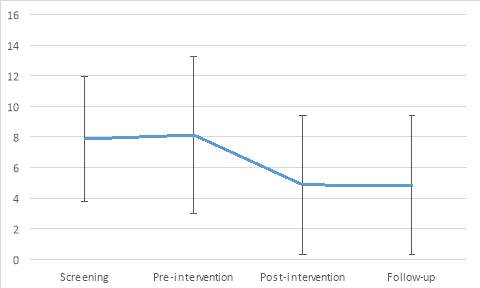
Line graph to show mean scores for the Generalised Anxiety Disorder (GAD-7) at screening, pre-intervention, post-intervention & follow-up (one standard deviation error bars)
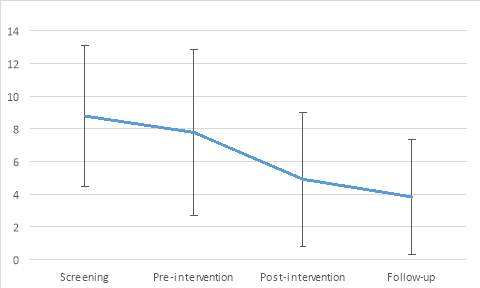
Line graph to show mean scores for the Rosenberg’s Self-Esteem Scale (RSES) at screening, pre-intervention, post-intervention & follow-up (one standard deviation error bars)
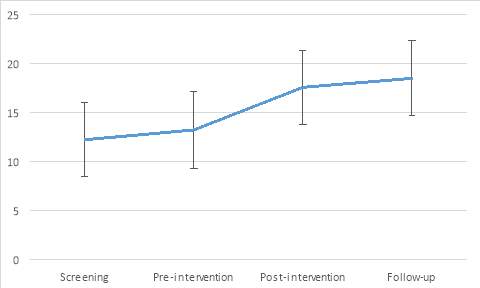
Line graph to show mean scores for ‘maladaptive’ perfectionism at pre-intervention, post-intervention & follow-up (one standard deviation error bars)
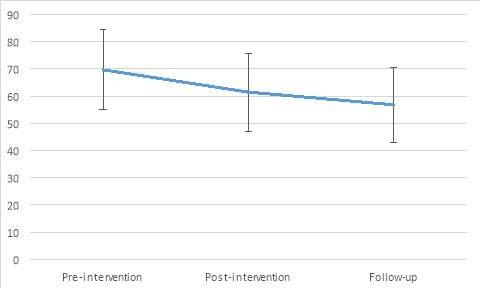
Appendix 21. Line graphs for process measures (SCS, ERQ-reappraisal, ERQ-suppression, and BES) at main study points
Line graph to show mean scores for the Self-Compassion Scale (SCS) at pre-intervention, post-intervention & follow-up (one standard deviation error bars)
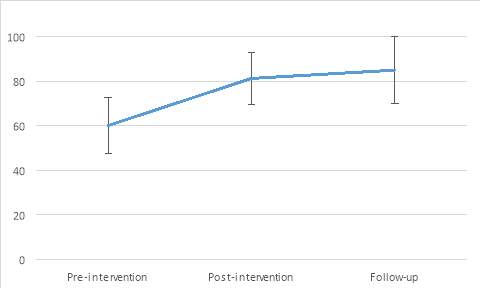
Line graph to show mean scores for the Emotion Regulation Scale (ERQ) Reappraisal at pre-intervention, post-intervention & follow-up (one standard deviation error bars)
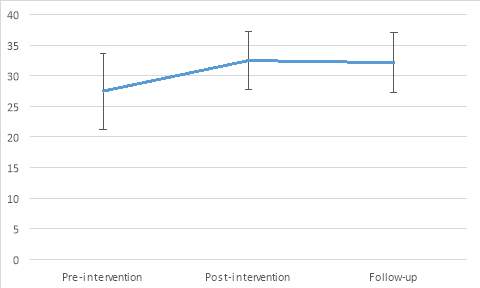
Line graph to show mean scores for the Emotion Regulation Scale (ERQ) Suppression at pre-intervention, post-intervention & follow-up (one standard deviation error bars)
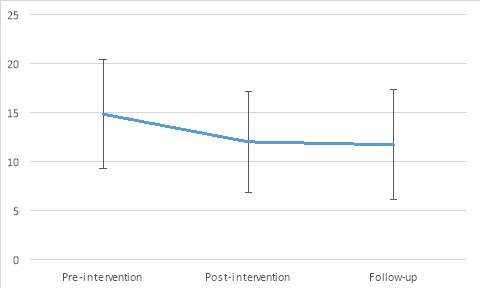
Line graph to show mean scores for the Beliefs about Emotions Scale (BES) at pre-intervention, post-intervention & follow-up (one standard deviation error bars)
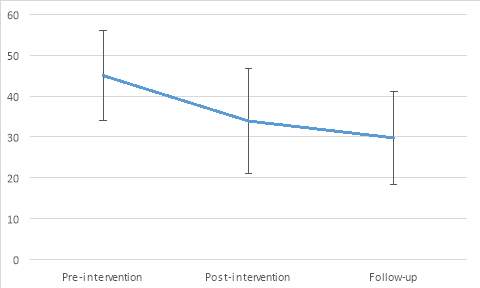
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Therapy"
Therapy is often thought of in relation to talk therapy, or psychotherapy, but therapy is simply a treatment not involving drugs or surgery that attempts to remedy a health problem, whether physical or mental.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




