Evaluation of Mindful Eating and Eating Pathology
Info: 7758 words (31 pages) Dissertation
Published: 6th Jan 2022
Tagged: PsychologyFood and Nutrition
MINDFUL EATING AND EATING PATHOLOGY: CORRELATION BETWEEN THE MINDFUL EATING QUESTIONNAIRE AND EATING DISORDER INVENTORY-3RD EDITION
Literature Review
Recently, several mindfulness-based interventions have been developed and tested to treat eating disorders, and eating-related psychological problems, and to aid in weight loss (L. Hulbert-Williams, Nicholls, Joy, & N. Hulbert-Williams, 2013). However, there is limited research on the relationship between mindful eating and eating pathology. Mindful eating is defined as the non-judgmental awareness of physical and emotional sensations associated with eating (Framson et al., 2009). Previous studies have focused on the relationship between mindful eating and weight-related issues and the development and validation of the Mindful Eating Questionnaire. The present study seeks to examine the relationship between mindful eating and eating pathology.
Eating Disorders
According to the National Eating Disorder Association, approximately 20 million women and 10 million men suffer from a clinically significant eating disorder at some point during their lifetimes (Wade, Keski-Rahkonen, & Hudson, 2011). The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (5th ed.; DSM-5; American Psychiatric Association, 2013) states that the lifetime prevalence of Anorexia Nervosa (AN) is approximately 0.4%, Bulimia Nervosa (BN) is approximately 1% to 1.5%, and Binge Eating Disorder (BED) is 1.6% (American Psychiatric Association, 2013). Despite the small point-prevalence of the aforementioned eating disorders, related symptoms such as disordered eating and disordered body image affect a growing number of individuals, particularly young women (Mantinolli et al., 2016).
AN and BN share characteristics such as avoiding weight gain and having a strong desire to maintain control over eating-related behaviors, urges, thoughts, and feelings (Butryn et al., 2013). BED is characterized by having recurrent episodes of binge eating occurring once a week for at least three months, lack of control over eating during an episode, marked distress during an episode, and feelings of disgust, depression, or guilt after an episode (APA, 2013). Additionally, all eating disorders are associated with extreme emotions, attitudes, and behaviors; thus, they can result in many psychological and life-threatening medical consequences (Fan et al., 2010).
Anorexia Nervosa
According to the DSM-5, there are three diagnostic criteria for Anorexia Nervosa (AN). The first criterion states that an individual’s caloric intake is significantly below the daily caloric requirement, leading to a considerably low body weight based on age, gender, development, and physical health condition (American Psychiatric Association, 2013). A body mass index (BMI) below 18.5 kg/m2 is considered a low body weight (APA, 2013).
The second criterion states that an individual must experience extreme fear of gaining weight and must engage in behaviors that help him or her avoid weight gain, despite being dangerously underweight (APA, 2013). Additionally, weight loss in these individuals does not decrease the intense fear of weight gain; instead it may increase it (APA, 2013).
The third criterion involves an individual’s indifference to his or her significantly low body weight and distortion of how he or she views and understands body weight or shape (APA, 2013).
These individuals believe they are overweight and can be concerned with specific body parts such as the abdomen, buttocks and thighs (APA, 2013). They engage in behaviors such as constantly weighing themselves, frequently looking in mirrors or measuring different body parts, and excessively worrying about feeling fat (APA, 2013). Their self-esteem is significantly dependent on their perceptions of their bodies. These individuals perceive weight loss as a great achievement and indicative of self-control (APA, 2013). These criteria must be met to be diagnosed with AN.
In addition, there are two subtypes within the diagnosis of AN, Restricting type and Binge-Eating/Purging type (APA, 2013).
Individuals with Restricting type do not engage in binge eating or purging behavior (APA, 2013). Their weight loss is through dieting, fasting, and/or excessive exercise (APA, 2013). Binge eating occurs when an individual consumes an amount of food that exceeds what most individuals consider normal in a given period of time, such as two hours. Purging behavior includes self-induced vomiting, or misuse of laxatives, diuretics, or enemas (APA, 2013).
Individuals with Binge-Eating/Purging type engage in recurrent episodes of binge eating or purging behaviors. The distinction between AN Binge-Eating/Purging subtype and Bulimia Nervosa is that individuals within this subtype of AN are significantly below normal body weight (APA, 2013).
Bulimia Nervosa
Individuals with Bulimia Nervosa (BN) commonly fall within the normal weight or overweight range (BMI ≥ 18.5 and < 30 in adults; APA, 2013). According to DSM-5, there are five diagnostic criteria for BN. The first criterion states that an individual must have recurrent episodes of binge eating (APA, 2013). An episode of binge eating is not restricted to one setting (APA, 2013). An individual may begin a binge in a public place and continue eating upon returning home (APA, 2013). During episodes, individuals believe that they lack control over their eating and have an inability to avoid eating or stop eating once started (APA, 2013). Binge eating is not restricted to certain types of food, but individuals most commonly binge on foods that they may avoid at other times (APA, 2013).
The second criterion states that an individual engages in recurrent inappropriate compensatory behaviors to avoid weight gain such as: self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise (APA, 2013).
The third criterion states that, on average, the binge eating and compensatory behaviors must occur at least once a week for three months (APA, 2013).
The fourth criterion states that the individual’s self-esteem is negatively influenced by body shape and weight (APA, 2013).
Finally, the fifth criterion states that these disturbances do not exclusively occur during episodes of Anorexia Nervosa. This is because individuals with BN are similar to individuals with AN in that they fear weight gain, desire to lose weight, and are dissatisfied with their bodies (APA, 2013).
Binge Eating Disorder
Individuals with Binge-Eating Disorder (BED) fall within the normal-weight, overweight, and obese ranges BMI (≥ 18.5, < 30 and > 30 in adults; APA, 2013). According to the DSM-5, there are five diagnostic criteria for BED. The first criterion states that an individual must have recurrent episodes of binge eating and experience a loss of control over eating during the episodes (APA, 2013).
The second criterion states that the binge-eating episodes must fall within three or more of the following categories: eating significantly faster than normal; eating even when feeling very full; eating large amounts of food despite not feeling hungry physically; eating alone to avoid the feeling of embarrassment by the amount of food eaten; and feeling disgusted, depressed, or extremely guilty with oneself after eating (APA, 2013).
The third criterion states that the individual experience marked distress regarding binge eating (APA, 2013).
The fourth criterion states that the binge eating, on average, occurs at least once a week for three months (APA, 2013).
Lastly, the fifth criterion states that the binge eating must not be associated with the recurrent use of improper compensatory behaviors seen in Bulimia Nervosa, and does not exclusively occur during a period of Bulimia Nervosa or Anorexia Nervosa (APA, 2013).
Eating Disorder Not Otherwise Specified
This category includes individuals who have symptoms of eating disorders that cause clinically significant distress or impairment in social, occupational, or other important areas of functioning; however, they do not meet the full criteria for any of the specific eating disorders (APA, 2013). The DSM-5 provides five examples of the otherwise specified category. The first type is Atypical Anorexia Nervosa (AN), in which all the criteria for AN are met, except significant weight loss (APA, 2013). Individuals in this category fall within the normal or above normal weight range (APA, 2013).
The second type is Bulimia Nervosa (of low frequency and/or limited duration), in which all of the criteria for BN are met, except that binge eating and improper compensatory behaviors occur less than once a week and/or for less than three months (APA, 2013).
The third type is Binge-Eating Disorder (of low frequency and/or limited duration), in which all criteria for BED are met, except binge eating occurs less than once a week and/or for less than three months (APA, 2013).
The fourth type is Purging disorder, in which recurrent purging behaviors such as self-induced vomiting and misuse of laxatives, diuretics, or other medications are used to influence weight or shape without binge eating (APA, 2013).
The fifth type is Night Eating Syndrome, which involves recurrent episodes of night eating. Individuals with this disorder consume excessive amounts of food after the evening meal or eat after awakening from sleep (APA, 2013). Individuals are aware of and can recall eating (APA, 2013). The night eating is not better explained by external factors such as changes in sleep-wake cycle or by local social norms (APA, 2013). Also, the night eating must cause significant distress and/or impairment in the functioning of the individual (APA, 2013). Additionally, the disordered pattern of eating is not better explained by BED or other mental disorders, medical disorders, or effects of medication (APA, 2013).
Problems Associated with Eating Disorders
There are several medical and psychological problems associated with eating disorders. Some of the known medical consequences associated with eating disorders include, but are not limited to, amenorrhea, loss of bone mineral density, hypertrophy (enlargement) of salivary glands, dental erosion, scars or calluses on the dorsal surface of the hand, lack of nutrients, abdominal pain, esophageal tears, gastric rupture, lanugo (soft, downy hair), hypotension, and hypertension (APA, 2013).
Psychological problems associated with eating disorders include, but are not limited to depressed mood, social withdrawal, irritability, insomnia, and anxiety (APA, 2013). Furthermore, AN has the highest mortality rate among psychiatric disorders (Arcelus, Mithchell, Wales, & Nielsen, 2011). Individuals with AN have an elevated suicide risk, with approximately 12 suicides per 100,000 cases of AN per year (APA, 2013).
Additionally, eating disorders cause significant impairments in cognitive functioning, judgment, emotional stability, and ability to engage in daily life activities (Wagner et al., 2016). Approximately one third of past patients relapse or develop another eating disorder diagnosis (Nyman-Carlsson, Engstrom, Norring, & Nevonen, 2014). These individuals have a high level of co-morbidity of both psychological and physiological problems, such as depression and anxiety disorders, and sleep deprivation and cardiovascular and gastrointestinal complications (Nyman-Carlsson et al., 2014).
Mindfulness
Mindfulness is defined as an “awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to the unfolding experience moment by moment” (Kabat-Zinn, 2003, p.145). In other words, the general emphasis of mindfulness is focusing on the present moment, and acknowledging and accepting one’s feelings, thoughts, and bodily sensations (Khan & Zadeh., 2014). Furthermore, mindfulness is associated with many positive health outcomes, such as decreasing depression, anxiety, and chronic pain, and increasing in immune functioning (Framson et al., 2009).
Research on Mindfulness and Eating Disorders
What is the connection between eating disorders and mindfulness? Research has shown that individuals with eating disorders have deficits in emotion recognition and emotional awareness, two concepts that are emphasized in mindfulness (Butryn et al., 2013). As a result, mindfulness-based treatments can be useful in treating eating disorders. Mindfulness-based treatments for eating disorders are developed using cognitive-behavioral, dialectical behavior, and acceptance and commitment approaches (Kristeller, Baer & Quillian-Wolever, 2006).
Research has examined the relationship between mindfulness and eating disorder symptomatology. A study by Butryn, Juarascio, Kerrigan, Clark, O’Planick, and Forman (2013) studied this relationship in women receiving residential treatment. The sample consisted of 105 patients who were diagnosed with either Bulimia Nervosa, Anorexia Nervosa, or Eating Disorder Not Otherwise Specifiedaccording to the DSM-IV. The patients were given several measures that included the Eating Disorder Examination-Questionnaire (EDE-Q; Fairburn &Beglin, 1994), the Eating Disorders Inventory-3rd edition (EDI-3; Garner, 2004), the Body Image Acceptance and Awareness Questionnaire (BI-AAQ; Sandoz, 2010), the Philadelphia Mindfulness Scale (PHLMS; Cardaciotto, Herbert, Forman, Moitra, & Farrow, 2008), the Emotional Avoidance Questionnaire (EAQ; Taylor, Laposa, & Alden, 2004), and The Eating Attitudes Thoughts and Defusion Scale (EATDS; Shaw, Butryn, Juarasico, Kerrigan, & Matteucci, unpublished manuscript).
Participant responses to the measures were evaluated at pre-treatment and post-treatment. The researchers found that eating disorder symptomatology was associated with lower awareness, acceptance, and cognitive defusion. Additionally, they found that eating disorder symptomatology was associated with higher emotional avoidance. The researchers concluded that improvements in these variables were related to improvements in eating disorder symptomatology (Butryn et al., 2013). This study provides evidence that practicing mindfulness can be beneficial for patients suffering from eating disorders.
A systematic review by Olson and Emery (2015) examined the effectiveness of mindfulness training in weight loss programs. The researchers searched for published studies through online databases, and reviewed and evaluated them for methodological strengths and weaknesses. The search yielded a total of 19 studies on the effects of mindfulness-based-interventions on weight loss. The studies included 13 randomized controlled trials and six observational. From the 19 articles, six randomized controlled trials showed significant weight loss among individuals in the mindfulness condition. Overall, 13 of the 19 studies found a relationship between significant weight loss and mindfulness interventions. However, there was no clarity regarding the degree to which mindfulness is responsible for weight loss. The researchers concluded that further research is needed to determine the relationship between mindfulness and weight loss (Olson et al., 2015).
Therapeutic Interventions Using Mindfulness
Mindfulness-based interventions are commonly used to address different types of dysregulation disorders, such as anxiety, depression, and addictions (Kristeller, Wolever & Sheets, 2013). A variety of mindfulness-based approaches have been used to treat clinical eating disorders. These approaches include Dialectical Behavior Therapy to treat BED and BN (DBT; Linehan, 1993), Mindfulness-Based Cognitive Therapy to treat BED (MBCT; Segal, Williamns, & Teasdale, 2002), Acceptance and Commitment Therapy to treat AN (ACT; Hayes, Strosahl & Wilson, 1999), and Mindfulness-Based Eating Awareness Training to treat BED (MB-EAT; Kristeller & Hallett, 1999). Mindfulness-based interventions are believed to result in improvements in eating pathology by allowing individuals to choose to respond to distress in a positive manner instead of engaging in negative eating behaviors or restricting eating (Prowse, Bore & Dyer, 2013).
Despite its origin in treating personality disorders, DBT has recently been used to treat individuals with BED and BN. Both BED and BN are associated with emotional regulation; therefore, DBT is a good solution because it focuses on improving an individuals’ ability to manage negative emotions adaptively by using skill modules that focus on mindfulness, emotional regulation, and distress tolerance (Kristeller et al., 2006). The mindfulness skills in particular are used to teach increased nonjudgmental awareness of one’s emotional states in the present moment without immediate behavioral reaction (Kristeller et al., 2006). This promotes emotional regulation because it teaches individuals to identify their emotions without focusing on changing or criticizing them, and engaging in impulsive reactions (Kristeller et al., 2006).
MBCT can be used to treat individuals with BED. These individuals typically avoid self-awareness and experience frequent negative thoughts and emotions due to not meeting their own personal standards (Kristeller et al., 2006). The focus of MBCT is to help individuals develop nonjudgmental and nonreactive recognition and acceptance of their bodily sensations, perceptions, cognitions, and emotions (Kristeller et al., 2006). There are four key purposes of this training in treating BED: 1) to improve individuals’ ability to identify hunger and satiety (feeling full) cues, 2) to increase willingness to experience negative emotional experiences related to the triggers of binge eating, 3) to decrease focus on negative thoughts, and 4) to train individuals to engage in positive behaviors in stressful situations (Kristeller et al., 2006).
ACT can be used to treat individuals with AN. Act is focused on mindfulness and acceptance-based strategies, and can be used to help individuals with AN address fat-related thoughts, body image issues, and fears of being overweight (Kristeller et al., 2006). ACT uses various analogies to help individuals visualize their thoughts and feelings as physical objects they can see and manipulate. One analogy used is called “thought parade,” which teaches individuals to observe thoughts nonjudgmentally and accept them, rather than acting on them by engaging in negative eating behaviors (Kristeller et al., 2006).
In this analogy, individuals are asked to imagine their “fat-related” thoughts written on cards and carried by participants in a parade. Their goal is to observe the parade of thoughts without believing or reacting to them (Kristeller et al., 2006). Another strategy used is called “bus driver,” which teaches individuals to experience “fat-related” thoughts in the present without acting towards them, and work towards their most valued goals (Kristeller et al., 2006). In “bus driver”, individuals are asked to imagine that they are bus drivers driving towards their most valued goals while their thoughts act as the passengers (Kristeller et al., 2006). In this case, their goal is to experience these thoughts and continue driving towards to their most valued goals, instead of changing directions based on their thoughts (Kristeller et al., 2006).
MB-EAT was specifically developed to treat BED (Kristeller et al., 2006). MB-EAT includes traditional mindfulness meditation techniques and guided meditation, which focuses on specific issues regarding shape, weight, and eating-related self-regulatory processes (Kristeller et al., 2006). MB-EAT sessions encourage individuals to use eating-related meditations, which help individuals develop nonjudgmental attention to sensations, thoughts, and emotions related to binge triggers, hunger, and satiety (Kristeller et al., 2006). The overall goal is to increase psychological and physiological self-regulation (Kristeller et al., 2006).
A study by Wallace (2017) examined the effectiveness of an intervention using techniques from ACT in addition to activities from The Body Project to decrease negative body image concerns and increase mindfulness skills in college females. The Body Project is a program designed for adolescent females that involves using dissonance-based activities and discussions to decrease eating disorder symptomology and prevent the development of future symptoms. Interventions used from ACT focused on teaching individuals how to separate who they are or their core beliefs from their maladaptive thoughts. Participants completed The Body Assessment (BA; Lorenzen, Grieve, & Thomas, 2004) and The Five Facet Mindfulness Questionnaire Short Form (FFMQ-SF; Bohlmeijer, ten Klooster, Fledderus, Veehof, & Baer, 2011) both before and after the combined ACT and The Body Project intervention. Results from this study revealed a significant difference in body image in participants after receiving the combined intervention. The researcher concluded that using specific ACT techniques and The Body Project activities can help reduce and prevent negative body image.
Mindful Eating
Mindful eating is defined as the non judgmental awareness of physical and emotional sensations associated with eating (Framson et al., 2009). Mindful eating was originally introduced to dieting for weight management; however, the focus of mindful eating is not on what is being eaten. Instead, the focus is on the process of eating (Khan & Zadeh, 2014). According to Albers (2008), the first step of mindful eating is to notice the taste, smell, and texture of the food being eaten. The second step is to identify daily habits such as eating while multitasking or eating subconsciously (Albers, 2008). The third step is to be aware of triggers that both initiate and stop eating (Albers, 2008). Mindful eating may help individuals use mindfulness-based strategies to identify and respond to hunger and satiety (Clementi, Casu & Gremigni, 2017). Mindful eating-based interventions have been effective in decreasing obesity-related behaviors, promoting weight loss, and reducing psychological distress in patients with BED (Clementi et al., 2017).
Results from a recent study by Prowse et al (2013) on mindfulness and eating disorder symptomatology indicated that the mindfulness skill described as “observing” was associated with higher reports of eating disorder symptoms. Furthermore, results indicated that the mindfulness skills of “acceptance without judgement” and “acting with awareness” were associated with lower levels of eating disorder symptoms (Prowse et al., 2013). Additionally, there was evidence that these skills are associated with greater resiliency against eating pathology. Another study by Khan and Zadeh (2014) revealed that mindful eating was positively correlated with overall mental well-being. The results of this study were consistent with previous research findings that individuals with high scores in psychopathology have lower levels of mindfulness skills, with the exception of skills related to “observing” (Baer, Smith, Hopkins, Krietemeyer, & Toney., 2006).
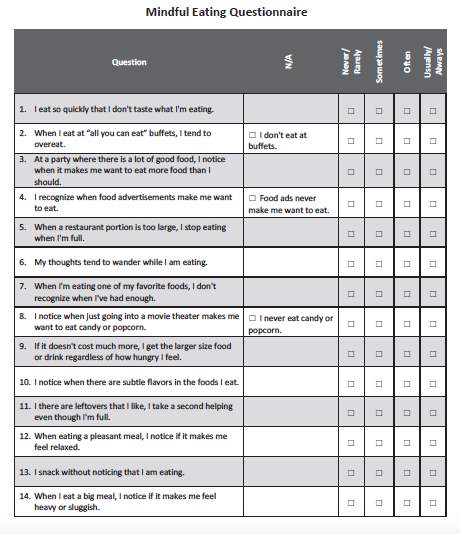
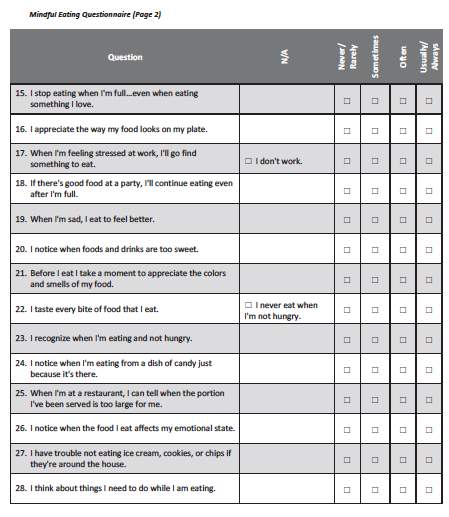
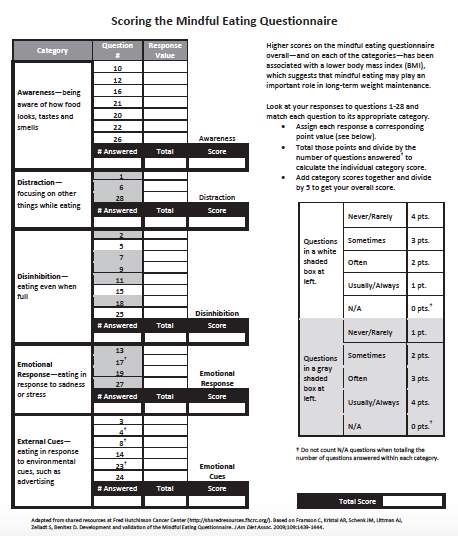
Mindful Eating Questionnaire
Previous studies have investigated both the development and validation of the Mindful Eating Questionnaire (MEQ; Framson et al., 2009). The MEQ has five indices, which are Disinhibition, Awareness, External Cues, Emotional Response, and Distraction (Framson et al., 2009). The Disinhibition index examines the inability to stop eating even when one is full (Framson et al., 2009). The Awareness index examines the ability to be aware of how the food looks, tastes, and smells (Framson et al., 2009). The External Cues index evaluates eating in response to environmental cues (Framson et al, 2009). The Emotional Response index examines eating in response to negative emotional states (Framson et al., 2009). The Distraction index examines the inability to focus on eating and being distracted by other things (Framson et al., 2009).
A study by Framson et al. (2009) evaluated the development and validation of the MEQ. The researchers selected a list of constructs for the MEQ through previously published studies on both eating behavior and mindfulness. Based on the results, they selected the Disinhibition index, External Cues index, and Emotional Response index. The final questionnaire included 28 items and five subscales. The questionnaire was distributed by mail to 510 participants who came from seven different convenience samples. Samples included 200 individuals from a yoga studio, 100 students from a university fitness facility, 40 individuals from a weight loss program, 40 individuals from a women’s weight loss and fitness facility, 40 individuals from a software development company, 40 individuals from a non-profit company, and 50 teachers and administrators from a preparatory school.
Participants were also required to self-report their weight, height, age, sex, race/ethnicity, highest level of education achieved, yoga practice, walking for exercise or transportation, and whether they took part in moderate or strenuous exercise. The researchers examined the MEQ in relation to demographic characteristics, and concluded that the MEQ had good measurement characteristics. The subscales in the MEQ had good internal consistency reliability, ranging from r = .64 to r = .83. The reliability of the MEQ summary score (mean of 5 subscale scores) was r = .64. The correlations among all the subscales ranged from r = .14 to r = .47. The correlations between subscales and the MEQ summary scores ranged from r = .57 to r = .71.
A recent study by Clementi et al. in Italy (2017) also assessed the psychometric properties of the MEQ. In this study, 15 experts evaluated the 28 items and the fives indices of the MEQ. The sample consisted of 1,067 Italian adults of which 61.4% were women. The participants completed the MEQ and the Freiburg Mindfulness Inventory (FMI; Buchheld, Buttenmuller, Kleinknecht, & Schmidt, 2006), and reported their gender, age, education, height and weight. Additionally, 62 participants completed a four-week test-retest. The content analysis limited the MEQ to 20 items. The researchers found adequate internal consistency, and test-retest reliability. The researchers concluded that there is good validity and reliability for the 20-item MEQ, and that this questionnaire can be used for evaluating eating-related issues. This study and the previously discussed study both show that the MEQ is a valid measure to examine eating-related issues such as eating behaviors and eating pathology.
Limitations of Existing Research
Research has been conducted to evaluate the development and validation of the Mindful Eating Questionnaire (MEQ). Studies have shown that there is a relationship between mindfulness and eating disorder symptoms. However, most studies have focused on the effectiveness of mindfulness-based interventions for treating eating disorders. There is a lack of research in examining whether deficits in the various indices of the MEQ are correlated with the risk of developing an eating disorder. Improving clinicians’ ability to identify those at risk for eating disorders would allow them to recognize and eradicate negative eating behaviors before the development of an eating disorder.
The Current Study
The purpose of the present study is to examine the relationship between mindful eating and eating pathology and to determine whether a mindful-eating questionnaire is a good predictor for eating disorder symptomology and disordered eating behavior. The current study will examine the correlations between the MEQ (MEQ; Framson et al., 2009) and the EDI- 3rd Edition (EDI-3; Garner, 2004). The study will specifically focus on examining the correlations between the overall MEQ score and the Eating Disorder Risk Composite score (EDRC) from the EDI-3rd Edition.
The EDRC is a global measure of eating and weight-related concerns. The EDRC score is comprised of three scales, which are Drive for Thinness (DT), Bulimia (B), and Body Dissatisfaction (BD). The DT scale assesses an individual’s desire to be thin, concern with dieting, preoccupation with weight, and an intense fear of weight gain. The B scale assesses an individual’s tendency to think about or engage in overeating. The DB scale assesses an individual’s dissatisfaction with overall shape and size of different areas of the body (i.e., stomach, hips, and thighs).
As discussed in the previous sections, individuals with AN are preoccupied with an intense fear of gaining weight and engage in bheaviors that help them avoid weight gain (APA, 2013). Individuals with BN lack control over their eating and engage in dangerous compensatory behaviors (APA, 2013). Indivdiauls with BED also have a loss of control over eating and they are unaware of hunger or satiety cues (APA, 2013). With this knowledge, it is evident that these individuals are not focused on the process of eating which is the essential feature of Mindful Eating.
The primary hypothesis is that there will be a negative correlation between the MEQ overall score and the EDI-3 eating disorder risk composite score. The secondary hypotheses are that there will be a negative correlation between MEQ overall score and Drive for Thinness, a negative correlation between MEQ overall score and Bulimia, and a negative correlation between MEQ overall score and Body Dissatisfaction.
Method
Participants and Design
Participants from this study will consist of male and female undergraduate students. Participants will be at least 18 years old and will vary in ethnicity, year in college, and age. A power analysis using nine studies found a mean effect size (Cohen’s d) of 0.63, which is a medium effect size. Using a within-subjects design, 80 participants per group yields a power of 88, which means that a true difference can be detected, if one is present, 88 percent of the time. There is one group in this study; therefore the total number of participants should be at least 80.
Measures
Demographics: Participants will be asked to report their age, gender, race/ethnicity, year in college, height, and weight. The height and weight will be used to calculate the participant’s body mass index (BMI). See appendix A.
Mindful Eating Questionnaire (MEQ; Framson et al., 2009): The MEQ consists of 28 items that assess Mindful Eating. The 28 items are divided into five subscales: Disinhibition, Awareness, External Cues, Emotional Response, and Distraction. Each subscale has three to eight questions. The five subscales evaluate an individual’s ability to stop eating when full; awareness of how the food looks, tastes, and smells; inclination to eat in response to external cues; tendency to eat in response to negative emotional states; and level of distraction while eating (Framson et al., 2009). An example item consists of, “I eat so quickly that I don’t taste what I’m eating.”
The 28 items are rated on a four-point Likert-type scale ranging from 1 (never/rarely) to 4 (usually/always). Specific items are reversed before scoring (1, 6, 28, 2, 5, 7, 9, 11, 18, 13, 17, 19, 27 ). Scores from each subscale are determined by dividing the sum of the response value by the number of questions answered. The MEQ overall score is determined by calculating the mean of the five subscale scores. Higher scores indicate more mindful eating. The MEQ has moderate reliability. Each subscale has good internal consistency reliability: Disinhibition (.83), Awareness (.74), External cues (.70), Emotional response (.71), and Distraction (.64) (Framson et al., 2009). See Appendix B.
Eating Disorder Inventory 3rd Edition (EDI-3; Garner, 2004): The EDI-3 assesses the behavioral and psychological traits commonly found in individuals with Bulimia Nervosa, Anorexia Nervosa, Other Specified Feeding and Eating Disorder, and Binge Eating Disorder. The EDI-3 consists of 91 items organized into 12 primary scales, which are as follows: Drive for Thinness (DT), Bulimia(B), Body Dissatisfaction(BD), Low Self-Esteem(LSE), Personal Alienation(PA), Interpersonal Insecurity(II), Interpersonal Alienation(IA), Interoceptive Deficits(ID), Emotional Dysregulation(ED), Perfectionism(P), Asceticism(A), and Maturity Fears(MT). An example item says “I exaggerate or magnify the importance of weight.”
The items are rated on a six-point Likert-type scale from Always to Never. While the participants will complete the entire EDI-3, for the purposes of the current study, only the DT, B, and BD scales will be considered. Scores for these three subscales are calculated by summing the response value for the questions answered in that subscale. Each subscale raw score is translated into a T-score. The three T-scores summed will provide an Eating Disorder Risk Composite score.Higher scores indicate higher levels of eating disorder symptomology and higher risks of developing an eating disorder. The EDI-3 has good internal consistency reliability ranging from .80 to .90 and test-retest reliability ranging from .93 to .98 (Garner, 2004). See Appendix C.
Procedure
After receiving Institutional Review Board approval, participants will be recruited at Western Kentucky University through the Department of Psychology Study Board system. The Study Board is an online program that allows participants to schedule to participate in active research studies. The recruiting message will inform participants that they must at least be 18 years old to participate. Upon arrival to the lab, participants will be given an informed consent form to complete, which will notify them of the confidentially of their results and their right to discontinue their participation at any time. Participants will receive a brief description of the study. Participants will also be made aware of any potential benefits or harms in this study, and in this case, there is minimal harm. Additionally, participants will be given a list of mental health resources available to help them in the event that they should experience any difficulties after the study.
The participants will complete the demographics questionnaire, the MEQ, and the EDI-3. The last two measures will be counterbalanced to avoid order effects. The study will take between 30 to 45 minutes to complete. These questionnaires will be scored and stored safely in a filing cabinet in Dr. Grieve’s office where only the research investigators will have access. After completing this study, the participants will be debriefed and sincerely thanked for their participation.
Proposed Data Analysis
Data will be analyzed and interpreted using the IBM’s SPSS 24 software. To calculate the MEQ subscale scores, questions answered within each subscale will be added according to the response value and the total sum for each scale will be divided by the number of questions answered. The MEQ overall score will be determined by adding all the subscale scores together and dividing it by 5. To calculate the Eating Disorder Risk composite score, the scores for the DT, B, and BD scales have to be calculated. The DT, B, and BD scores will be calculated by summing the response value for the questions answered in each subscale. The raw score from each subscale will be translated into T- scores. The three T-scores summed will provide an Eating Disorder Risk composite score.
Hypothesis Testing
The primary hypothesis states that there will be a negative correlation between the overall MEQ score and the Eating Disorder Risk composite score. To test this hypothesis, a correlation and a regression analysis will be conducted. The bivariate Pearson correlation coefficient (r) will help determine and measure the strength of the linear relationship between the two questionnaires used in the study. The regression analysis will examine if scores from one variable can be predicted by the scores on a second variable. A 1 X 3 one-way Analysis of Variance (ANOVA) will be conducted to determine whether there are any statistically significant differences in the MEQ overall scores between participants who have elevated clinical, typical clinical, and low clinical Eating Disorder Risk composite scores. A 1 X 3 ANOVA will be conducted to determine whether there are any statistically significant differences in the Eating Disorder Risk composite scores between participants who have high, medium, and low MEQ overall scores.
The secondary hypotheses states that there will be a negative correlation between MEQ overall score and Drive for Thinness, a negative correlation between MEQ overall score and Bulimia, and a negative correlation between MEQ overall score and Body Dissatisfaction. To test these hypotheses a correlation and a regression analysis will be conducted.
References
Albers, S. (2008). Eat, drink, and be mindful: How to end your struggle with mindless eating and start savoring food with intention and joy. Oakland, CA: New Harbringer Publications.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Arcelus, J., Mitchell, A. J., Wales, J., & Nielsen, S. (2011). Mortality rates in patients with Anorexia Nervosa and other eating disorders. Archives of General Psychiatry, 68, 724- 731
Baer, R.A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 12, 27-45. doi: 10.1177/1073191105283504
Bohlmejer, E., ten Klooster, P. M., Fledderus, M., Veehof, M., & Baer, R. (2011). Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment, 18, 308-320.
Buchheld N, Grossman P, Walach H. Measuring mindfulness in insight meditation (Vipassana) and meditation-based psychotherapy: the development of the Freiburg Mindfulness Inventory (FMI). J Medit Medit Res. 2001; 1:11-34
Butryn, M. L., Juarascio, A., Shaw, J., Kerrigan, S. G., Clark, V., O’Planick, A., & Forman, E. M. (2013). Mindfulness and its relationship with eating disorders symptomatology in women receiving residential treatment. Eating behaviors, 14, 13-16. doi: 10.1016/j/eatbeh.2012.10/005
Cardaciotto, L., Herbert, J. D., Forman, E.M., Moitra, E., & Farrow, V. (2008). The assessment of present-moment awareness and acceptance: The Philadelphia mindfulness scale. Assessment, 87, 116-117.
Clementi, C., Casu, G., & Gremigni, P. (2017). An abbreviated version of the mindful eating questionnaire. Journal of Nutrition Education and Behavior, 49, 352-356. doi: 10.1016/j.jneb.2017.01.016.
Fairburn, C. G., & Beglin, S. J. (1994). Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders, 16, 363-370.
Fan, Y., Li, Y., Liu, A., Hu, X., Ma, G., & Xu, G. (2010). Associations between body mass index, weight control concerns and behaviors, and eating disorder symptoms among non-clinical Chinese adolescents. BMC Public Health, 10, 314. doi: 10.1186/1471-2458-10-314
Framson, C., Kristal, A., Schenk, J., Littman, A., Zeliadt, S., & Benitez, D. (2009). Development and validation of the mindful eating questionnaire. Journal of the American Dietetic Association, 109, 1439-1444. doi: 10.1016/j.jada.2009.05.006
Garner, D. M. (2004). The Eating Disorder Inventory-3: Professional manual. Odessa, FL: Psychological Assessment Resources, Inc.
Hayes, S. C., Strosahl, K. D., & Wilson, K.G. (1999). Acceptance and commitment therapy: An experimental approach to behavior change. New York: Guliford Press.
Hulbert-Williams, L., Nicholls, W., Joy, J., & Hulbert-Williams, N. (2013). Initial validations of the mindful eating scale. Mindfulness, 5, 719-729. http://dx.doi.org.libsrv.wku.edu/10.1007/s12671-013-0227-5
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: Past, present and future. Clinical Psychology: Science and Practice, 10, 144-156. doi: 10.1093/clipsy.bpg016
Khan, Z., & Zadeh, Z. F. (2014). Mindful eating and its relationship with mental well-being. Procedia-Social and Behavioral Sciences, 159, 69-73 https://doi.org/10.1016/j.sbspro.2014.12.330
Kristeller, J. L., Baer, R. A., & Quillian-Wolever, R. (2006). Mindfulness-based approaches to eating disorders. In R. A. Baer, R. A. Baer (Eds.), Mindfulness-based treatment approaches: Clinician’s guide to evidence base and applications, 75, 76-91. San Diego, CA, US: Elsevier Academic Press. doi: 10.1016/B978-012088519-0/50005-8 http://dx.doi.org.libsrv.wku.edu/10.1016/B978-012088519-0/50005-8
Kristeller, J L., & Hallett, C. B. (1999). An exploaratory study of a meditation-based intervention for binge eating disorder. Journal of Health Psychology, 4, 357 – 363. doi:10.1177/135910539900400305
Kristeller, J., Wolever, R.Q., & Sheets, V. (2013). Mindfulness based eating awareness training (MB-EAT) for binge eating; A randomized clinical trial. Mindfulness, 5, 282-297. doi: 10.1007/s12671-012-0179-1
Linehan, M. M. (1993). Cognitive-bheavioral treatment of borderline personality disorder. New York: Guliford.
Lorenzen, L. A., Grieve, F.G. & Thomas, A. (2004). Exposure to muscular male models decreases men’s body satisfaction. Sex Roles, 51, 743-748.
Mantinolli, H.M., Mannisto, S., Siploa-Leppanen, M., Tikanmaki, M., Heinonen, K., Lahti, J., … & Lano, A. (2016). Body image and eating behavior in young adults born preterm. International Journal of Eating Disorders., 49, 572. doi:10.1002/eat.22553
Nyman-Carlsson, E., Engstrom, I., Norring, C., & Nevonen, L. (2015). Eating Disorder Inventory-3, validation in Swedish patients with eating disorders, psychiatric outpatients and normal control sample. Nordic Journal of Psychiatry, 69, 142 doi:10.3109/08039488.2014.949305
Olson, K. L., & Emery, C. F. (2015). Mindfulness and weight loss: A systematic review. Psychosomatic medicine, 77, 59-67. http://dx.doi.org.libsrv.wku.edu/10.1097/PSY.0000000000000127
Prowse, E., Bore, M., Dyer, S. (2013). Eating disorder symptomatology, body image, and mindfulness: Findings in a non-clinical sample. Clinical Psychologist, 17, 77-87. doi: 10.1111/cp.12008
Sandoz, E. K. (2010). Assessment of body image flexibility: An evaluation of the body image acceptance and action questionnaire. (unpublished doctoral dissertation.) University of Mississippi, Oxford, Mississippi.
Segal, Z. B., Williams, J.M. G., & Tesdale, J.D. (2002). Mindfulness-based cognitive therapy of depression: A new approach to preventing relapse. New York: Guliford.
Shaw, J., Butryn, M. L., Juarascio, A. J., Kerrigan, S. G., & Matteucci, A. J. (unpublished). Eating attitudes thoughts and defusion scale.
Taylor, C. T., Laposa, J. M., & Alden, L.E. (2004). Is avoidant personality disorder more than just social avoidance? Journal of Personality Disorders, 18, 571 – 594.
Wallace, S. (2017). Acceptance and commitment therapy as an eating disorder intervention. (unpublished master’s thesis.) Western Kentucky University, Bowling Green, KY.
Wade, T. D., Keski-Rahkonen A., & Hudson J. (2011). Epidemiology of eating disorders. In M. Tsuang & M. Tohen (Eds.), Textbook in psychiatric epidemiology (3rd ed.) (pp. 343-360). New York: Wiley.
Wagner, R., MacCaughelty, C., Rufino, K., Pack, T., Poplack, J., George, K., & Ruscitti, C. (2016). Effectivenes of a track-based model for treating eating disorders in a general psychiatric hospital. Bulletin of the Menninger Clinic, 80, 49-59. doi: http://dx.doi.org/101521bumc201680149
Appendices
Appendix A: Demographics
1. Age: _______________
2. Race/Ethnicity:
a. African American
b. Asian American
c. White, non-Hispanic
d. White, Hispanic
e. Middle Eastern
f. Other: _______________
3. Current Academic Status:
a. First-year college student
b. Second-year college student
c. Third-year college student
d. Fourth-year college student
e. Fifth (or higher)-year college student
4. College Academic Major: _______________
5. Weight: _________
6. Height: __________
7. Gender:
a. Male _______
b. Female _____
c. Other ________
Appendix B: The Mindful Eating Questionnaire
Appendix C
The Eating Disorder Inventory-3 (EDI-3) is not attached to this document due to copyright issues. The publishing company states that the EDI-3 may not be reproduced in whole or in part in any form.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Food and Nutrition"
Food and Nutrition studies deal with the food necessary for health and growth, the different components of food, and interpreting how nutrients and other food substances affect health and wellbeing.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




