Knee Joint Anatomy, Biomechanics and Development of Knee Molds
Info: 4858 words (19 pages) Dissertation
Published: 16th Dec 2019
Tagged: Physiology
1.0 Introduction
The knee joint is the largest and one of the most complex joints in the human body. The knee joint is very susceptible to injury, due to the huge amount of stresses and strain it experiences.
2: Literature Review
2.1 Knee Anatomy
The knee joint is the largest and one of the most complex joints in the human body. The knee joint is very susceptible to injury, due to the huge amount of stresses and strain it experiences. The knee is made up of four different bones, ligaments, muscles and tissues. The knee is a modified hinge joint that must allow flexion and rotation, but must still provide complete stability and control under a great range of loading conditions (Goldblatt and Richmond 2003).
The bones which join together to make up the knee joint are the thigh bone (femur), which is the largest bone in the human body, to the shin bone (tibia). A smaller bone that runs alongside the tibia (fibula) and the patella (commonly known as the kneecap). These bones are connected by supporting and guiding muscles, tendons, ligaments, menisci, the joint capsule, bursae and infrapatellar fat body. (SHENG, 2008)
The knee consists of 2 joints: the femorotibial joint and the patellofemoral joint. The bony architecture of the femur, tibia, and patella contribute to the stability of the knee joint, along with static and dynamic restraints of the ligaments, cap- sule, and musculature crossing the joint (Goldblatt and Richmond 2003).
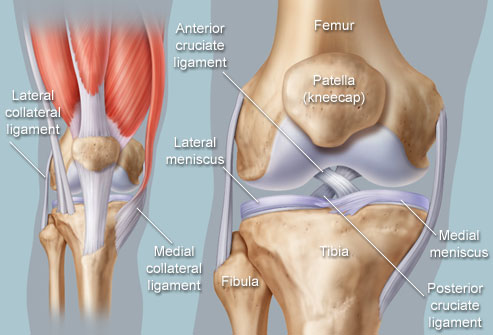
The femur is the large bone of the thigh. The bone is the longest and strongest bone in the human body. On the distal end (lower end), the femur forms the knee joint with the tibia of the lower leg. The lower end of the femur divides into two condyles, termed the medial condyles and the smaller of the two, the lateral condyles. These condyles contain a smooth articular surface that rests on the upper tibia condyles to form the knee joint (Clippinger 2007).
These two condyles are separated by the intercondylar fossa (notch). Intercondylar fossa is a notched area between the condyles on the posterior surface. The cruciate ligaments, which help bind the femur to the tibia, have their proximal attachment in this notch (Patton 2015).
The main purpose of the condyles is to assist the knee when it is rotating and improve overall performance of the joint. Condyles are cam shaped in the side profile. The medial condyle is the larger condyle and is located on the inside of your leg the medial is larger because there is more weight on it than the lateral.
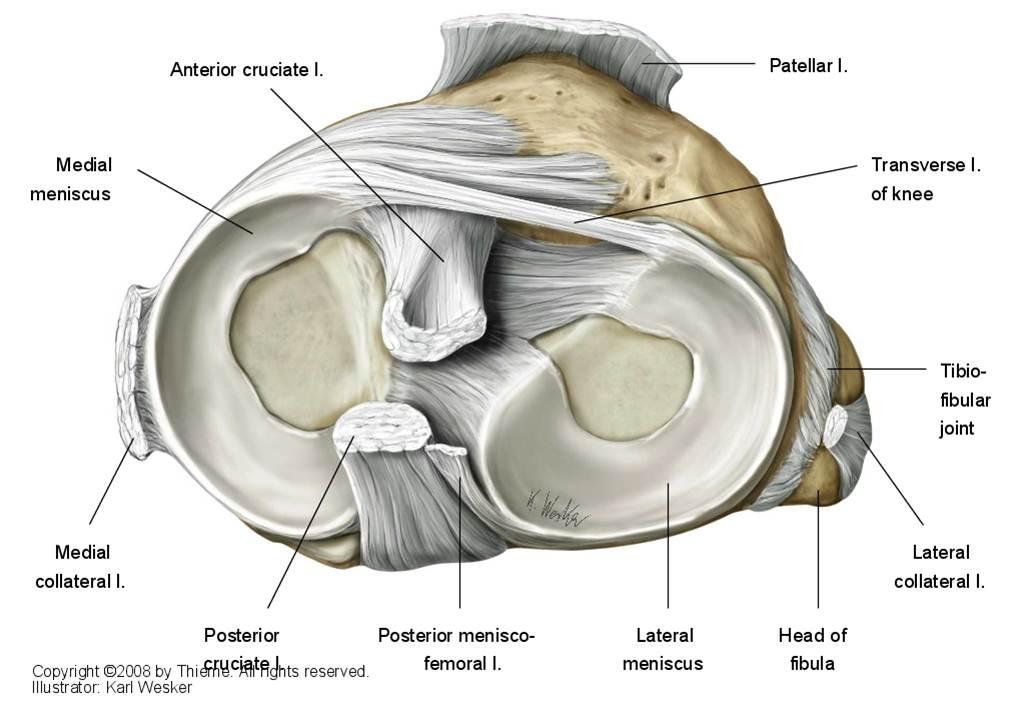
The tibia bone is the long bone of the shin, which has a thickened proximal end which contains two condyles, known as the medial condyle and the lateral condyle. These are separated by an intercondylar eminence. The cartilage of the menisci attaches in this region and also the anterior and posterior ligaments attach in this region. The superior surface of the tibia is known as the tibial plateau. This is where meniscus is found, the meniscus is on both the medial and lateral side. They are also known as semilunar cartilages because of their moon like structures. Their function is to act as shock absorbers and accommodate changes of movement of bones at the joint. (???)
The third component of the bone structure in the knee joint is the patellofemoral joint. This consists of the patella (commonly known as the knee cap) and the femur. The patella is a sesamoid bone, meaning a bone that is imbedded in a tendon, which sits in front of the femur. It is the largest sesamoid bone in the body (Pastides,Shenoy and Nathwani 2013).
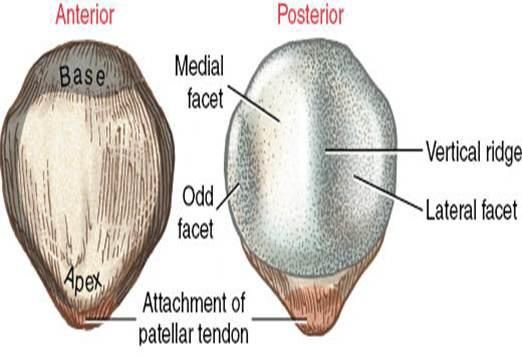
The patella is totally embedded within the tendon. The front face of the patella is convex in shape and is divided up into 3 parts. The top surface is where the patella and the quadriceps tendon intersect and this lightly covers the anterior surface of the patella and forms a deep fascia, which acts as a supporter to the bone. The middle part of the patella has a very high amount of vascular openings, which are very tiny in size. The last third of the patella is the intersection of the patellar ligament (Pastides,Shenoy and Nathwani 2013).
The posterior surface of the patella is divided into an inferior and superior parts. The inferior portion of the patella is non-articulating and represents roughly a quarter of the patellar height. The rest of the surface forms the superior portion, the articulating surface, which is covered in hyaline cartilage. The cartilaginous posterior surface is further divided by a rounded vertical ridge. It has a larger lateral portion for articulation with the lateral condyle of the femur and a smaller medial portion for articulation with the medial condyle of the femur. The medial and lateral facets are divided into superior, middle and inferior facets. There is a seventh facet termed the ‘odd facet’ located towards the medial facet. This does not articulate with the femur until flexion goes past 90° (Pastides,Shenoy and Nathwani 2013).
The fibula is the smaller shin bone; it is located lateral to the tibia. The superior end of the fibula meets with the posterior aspect of the lateral condyle of the tibia. The fibula is considered to be part of the knee joint, but the tibio-fibular joint is not (Sheng 2008).
This concludes Anatomy of the Knee section, for the next part of this thesis the biomechanics of the knee will be examined and discussed in detail.
2.2Biomechanics
2.2.1 Kinematics
Kinematics is a division of mechanics which describe the motions of points, objects and system of objects without the orientation to the forces producing them (Sheng 2008)
The knee is locked in full extension by the “screw-home mechanism”, which allows maintenance of this position with a small amount of energy used. The knee allows up to 160° of flexion and from up to five degrees of hyperextension (Shenoy,Pastides and Nathwani 2013)
“The amount of flexion required varies from about 60° needed for normal walking, 80° to climb stairs, 90° to descend down stairs, 115° to sit down on a toilet seat and up to 130° to squat.”
This flexion is a combination of rolling and gliding. In early flexion, up to 20°, a rolling movement takes place that translates the point of tibiofemoral contact posteriorly. If flexion is continued, there is a gliding movement, with a greater posterior translation of the lateral tibiofemoral contact point in relation to the medial contact point. Along with flexion and extension the knee allows 25°–30° of rotation, 6°–8° of valgus and varus in extension. The knee joint can be regarded as a joint that allows movement with six degrees of freedom (Shenoy,Pastides and Nathwani 2013).
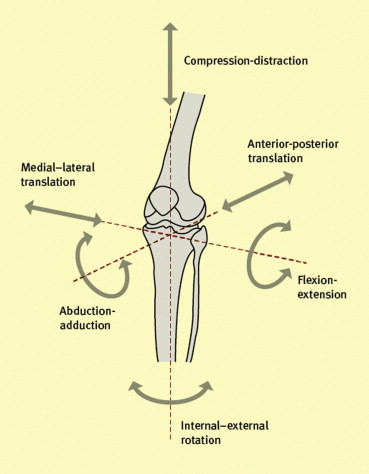
The most frequent knee movement occurs during gait (walking). Knee motion is dictated by the consideration of energy that requires the centre of gravity of the body to move forward with as little upper body movement as possible, and the ability to absorb the impact at heel strike. During the swing phase of gait, the knee flexes to roughly 60° so the toe of the swinging leg does not be dragged on the ground. Also during gait, as the swinging leg passes the standing leg and just before heel strike, the quadriceps muscle contracts which brings the knee to full extension and the foot forward. Flexion isn’t the only rotation that takes place during the gait cycle, as the knee extends 30° to 0°, the tibia externally rotates up to 30° before heel strike. The term used to describe this is “screw-home mechanism”. This mechanism occurs to tighten the soft tissue structures as well as locking the knee geometry before the impact load of weight bearing (Masouros,Bull and Amis 2010).
Movement in the knee joint is mainly guided by the shape of the joint surfaces of the femur and of the tibia, and by the way the major ligaments of the knee joint are orientated. The 4 main ligaments play a big role in the dynamic stability during movement of the knee. The 4 main ligaments are the anterior cruciate ligament (ACL), posterior cruciate ligaments (PCL), the medial collateral ligament (MCL) and the lateral collateral ligaments (LCL). (sheng)
Cruciate ligaments are made up of two ligaments, the anterior (ACL) and posterior (PCL), these are very much the most recognizable of the ligaments because they are very much injury prone. They are very important in the function of the knee as they allow the joint both to slide and roll, but at the same time maintaining stability. Their names are given for which the site of attachment to the femur and tibia and they cross each other indirectly.
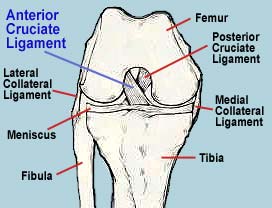
Cruciate ligaments: The ACL is the main restraint to anterior tibial movement. It also acts against hyperextension, acts as a secondary restraint to internal and valgus movement when at full extension. The ACL controls the “screw-home motion” of the knee joint (Masouros,Bull and Amis 2010).
“Sectioning the ACL produces a significant increase in anterior knee instability. The greatest amount of anterior translation after isolated ACL sectioning occurs between 15° and 45°. The ACL reaches ulitimate stress at approximately 15% strain, and gross failure is expected to occur when strain exceeds 15% to 30%, or displacement of about 1 cm.” (JOHN P. GOLDBLATT, MD, and JOHN C. RICHMONd)
The (PCL) posterior cruciate ligament is the main restraint to posterior tibial translation and is most effective in mid to deep flexion. Working together, the ACL and PCL control the anterior posterior rolling and sliding kinematics of the TF joint during flexion and extension (Masouros,Bull and Amis 2010).
Medial collateral ligament: the medial collateral ligament (MCL) is the main restraint to valgus angulation and internal tibial rotation and is a secondary restraint to external tibial rotation. It is also a secondary restraint to anterior tibial translations when the tibia is externally rotated (Masouros,Bull and Amis 2010).
Lateral collateral ligament: the lateral collateral ligament (LCL) is the main restraint to varus angulation, but it has less of an effect with knee joint flexion, which reduces its restraining capability. It is a secondary restraint to posterior translations when those are large and, combined with the posterolateral corner (PLC), is a primary restraint to external tibial rotation (Masouros,Bull and Amis 2010).
2.2.2 Loading
The loads that the joints of the knee experience are a result of external forces, for example ground reaction forces and the muscle forces that are required to maintain posture and help body movement. Body weight passes along the mechanical axis, which is an imaginary line, of the lower limbs of the body. The line goes from the centre of the hip to the centre of the ankle, passing through the middle part of the knee joint. Variation outside this line can show up a deformity in the knee, known as either valgus or varus deformities. One of the goals in knee surgery is to restore the normal alignment and mechanical axis to normalize the knee during gait. (sheng)
Because of the complexity of the knee joint, forces within the different structures of the knee cannot be measured accurately during daily activities of the knee. Research has esti-mated that the TF joint experiences 3.4 times body weight when walking, 4.3 times body weight when ascending stairs and 4.0 times when descending a ramp (Masouros,Bull and Amis 2010).
In the PF joint, when the knee is in extension as shown (reference figure) in the lines of action, the patellar tendon and the quadriceps muscle are almost linear in the sagittal plane and result in a small force (Masouros,Bull and Amis 2010).
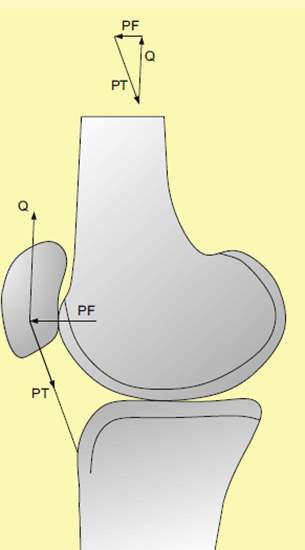
(reference fig) shows the PF joint at 90° flexion, as the knee flexes the angle between the lines of action of the patellar tendon and the quadriceps muscles reduces down. This increases the PF joint force to approximately 70° knee flexion.
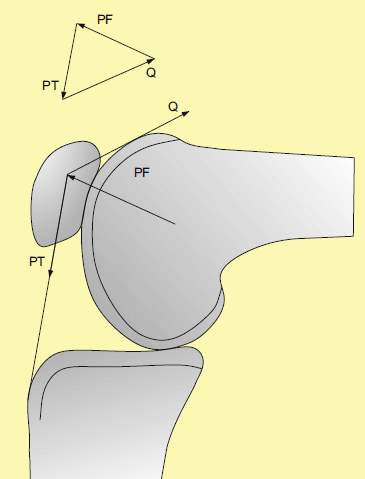
The area between the patella and femur increases contact with increasing flexion, this maintains physiological contact stresses. When knee flexion increases over 70° the quadriceps muscles wrap around the trochlea so the stress doesn’t increase. When rising from a chair it re-quires 100° of knee flexion to bring the body to the upright position which creates maximum quadriceps tension (Masouros,Bull and Amis 2010).
When walking a major portion of the load is transmitted through the menisci. The menisci in-crease the contact area between the rounded femoral condyles and its tibial plateau on the medial side, and the convex tibial plateau on the lateral side. This plays an important role in loading in healthy joints. (sheng)
2.3 Knee Angular Deformities
Angular Deformities to do with the knee are common during early childhood and can usually be put down to variations in the normal growth pattern and development of a child. Angular deformity varies with a child’s age.
Genu Valgum/Varum:
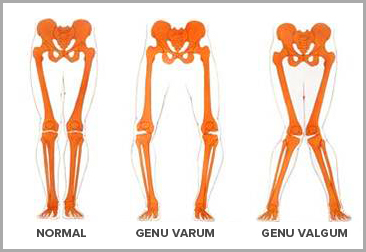
Genu Valgum (knock-kneed): The head of the tibia (not the actual joint itself) is inclined away from the medial (midline) of the body.
Genu Varum (bow-legged): The head of the tibia is inclined toward the medial of the body.
Genu valgum and genu varum are common frontal plane deformities. Physiologic forms are the most common; however, pathological forms (those occurring outside the normal range of the mean) are important to distinguish. New-born’s normally have a tibiofemoral angle of 10°-15° of varum angulation. This inherent varum is lost and the knee progressively moves in a valgum direction, straightening out at about two years of age and reaching a maximal valgum angulation of 10°-15° at age 3. The normal knee then gradually resolves to the qhysiologic knee valgum of 7°-8° by age 10 or 11 (Scuderi and Tria 2010).
Mechanical axis: A line drawn from the centre of the femur head to the centre of the proximal end of the tibia, should fall through the middle of the knee. Lateral position to the centre of the knee indicates valgum angulation, while, medial position to the centre of the knee indicates varum angulation. The angle id described by the line bisecting the distal end of the femur and the line bisecting the proximal end of the tibia. The normal angle is between 6°± 2° (Crim,Manaster and Rosenberg 2017).
Genu valgum (knock knees)
This disorder of the knee position is characterized by the closeness to one another of the two condyles. The result is an imbalanced distribution of weight on the knee joint and extra loads and wear on the lateral aspect of the joint. The cause of genu valgum is usually structurally natural, but it may also be part of a chain reaction to foot eversion (Solberg 2007).
Genu varum (bowlegs)
More commonly known as bow-legged, genu varum is very common in early childhood. If a child has genu varum one or both of the child’s legs curve outwards. This disorder is characterized by a greater than normal distance between the knee in the erect (straight up) position. Here, weight distribution on the tibia surface is imbalanced, with the medial aspect of the knee bearing the main load. In addition to structural causes, genu varum is often the result of inverted foot position (Solberg 2007).
Causes of genu valgum:
Genu valgum usually is part of the normal growth and development of the lower extremities. Some cases, especially in a child who’s 6 years or older, may be a warning sign of an underlying bone disease, such as osteomalacia or rickets. Obesity can be a big contributor to genu valgum or can cause gait (walking) problems that resemble, but aren’t, genu valgum. The condition can occasionally result from an injury to the growth area of the shin bone (tibia), which may result in just one knee having genu valgum. During the development of normal alignment of their lower extremities, all young children have genu valgus to some degree for a period of time. At the age of 3, more than 20 percent of children have at least a 5-centimeter gap between their ankles. By the age of 7, only 1 percent of children have this gap.
Idiopathic: Idiopathic genu valgum occurs when normal physiological variants fail to resolve. Valgum deformity with an intermalleolar distance exceeding 8-10 cm is most common. Other risk factors include flat feet and ligamentous laxity. The deformity is mainly cosmetic but cases where the intermalleolar distance is >8cm or the tibiofemoral angle is greater than 15°-20° should be evaluated with radiographs, as there is an increased risk of lateral compartment arthritis. In most cases the distal femur is the source of the deformity (Scuderi and Tria 2010).
Posttraumatic: Trauma is the most common cause of nonidiopathic genu valgum, a form that is either congenital or that has no known cause. Distal femur or proximal tibia epiphyseal fractures can lead to growth arrest. Genu valgum can also be caused by a fracture at the medial proximal tibial metaphysis, termed a cozen fracture. The possible cause of this deformity includes stimulation of the proximal tibia physis due to fracture hyperaemia, tethering of the intact lateral periosteum interposition of the medial soft tissue. Fortunately, genu valgum after a Cozen fracture typically resolves itself after time (Scuderi and Tria 2010).
Metabolic: Renal osteodystrophy, this is a bone disease that occurs when your kidneys fail to maintain proper levels of calcium and phosphorus in the blood, which causes genu valgum because the tibiofemoral angle is usually in valgus when the disease begins to manifest itself. Once the disease starts, it leads to a progression of genu valgum deformity (Scuderi and Tria 2010).
Neuromuscular: Genu valgum can occur in a patient with neuromuscular disorders. Patients usually have pes valgum (deformity of the foot) and external tibial torsion which results in a different loading on the lateral compartment of the knee. After contiuued growth and weight bearing, valgum deformity of the ankle and knee will occur. Patients with paralytic disorders can develop genu valgum from the contraction of the IT and abnormal gait patterns.
Infection: Osteomyelitis (inflammation of bone or bone marrow) can destroy or stimulate the growth plate and therefore can cause genu valgum and genu varum.
Causes of genu varum:
Physiological genu varum: Most children below the age of two have signs of bow leggedness, as part of a normal physiological process. Normally the bowing will correct itself by the age of three or four and the legs will have a normal appearance.
Blount’s disease: Blount’s disease is an abnormality of the growth plate at the proximal portion of the tibia. This disease can be recognized into two types based on age: infantile and juvenile. The infantile form usually occurs on both legs. A metaphyseal – diaphyseal angle of less than 11° is most likely varum, while those with an angle greater than 16° have a very high incidence of progressive deformity. Using a brace is most effective in children under three years of age with a metaphyseal – diaphyseal angle greater than 16°. Juvenile Blount’s disease is less severe than infantile. Although the etiology of infantile and juvenile Blount’s disease is unknown, mechanical factors are more likely the cause in the juvenile form. Nearly all children with juvenile Blount’s disease have a previous history of varum deformity, which was never completely corrected. The deformity than worsens as they reach their growth spurt. There is no role for bracing in this form of Blount’s disease (Scuderi and Tria 2010).
Rickets: This is a bone disease that occurs in children due to a lack of vitamin D, calcium or phosphorus that are essential for the growth of healthy bones.
Congenital Deformations: Achondroplasia is the most common genetic cause of bowing. This autosomal dominant disease is characterized by a defect in the endochondral bone formation. Typically, overgrowth of the fibula is seen. Bracing is ineffective and only surgical correction is an option if the deformity is painful or progressive (Scuderi and Tria 2010).
The main symptom is the obvious bowing of the legs that can be seen when a child is standing straight up and walking. Some other common symptoms are turning in of the feet and an awkward walking pattern. Genu varum does not usually cause any pain, but during adolescence, discomfort in the hips, knees, and or ankles may occur.
2.4 Knee Simulators
Knee simulators are quite a commonly used for testing wear in knee implants. Knee simulators have been used because of their ability to replicate realistic joint motion, force and environmental conditions. There are a number of these simulators produced by various companies and institution’s, they also have different in range of motion and degrees of freedom. The multi axial wear simulators are being used to give a more accurate simulation of the knee in motion. There are two types of wear test equipment.
3.0 Materials & Methods
The overall rig was of an existing project so no major manufacturing has been done to date which is a big advantage as it allows more time to focus on the literature review.
The overall structure is made from mild steel plates; these plates wear then welded to form the rig
The design of the knee rig consists of two pneumatic actuators, the top one been a rotary actuator and the bottom one a linear actuator. Both of these actuators wear sourced from the pneumatics lab within GMIT. The two actuators connect to the knee molds with a 6mm steel bar. The bottom actuator is designed to mimic the pressure acting upwards from the tibia while the rotary actuator is designed to mimic the degree of a person during walking.
This design also saved a lot of time as the overall rig structure was of an existing project so no welding had to be done.
The control of this rig is done through a PLC, the housing for this PLC is suited on the door, and the door also houses the switch. The whole programming system is housed on the front door of the rig structure. Putting these components on the front door gives this rig an overall safety feature.
The polyester resin was not sourced within GMIT it was sourced off a private vendor for €28.50
The PLC was sourced within GMIT; the type of PLC used was a Mitsubishi FX1s-14MT. This PLC was powered by 24v; it was decided to have an on/off switch and an emergency stop button also. General specifications can be seen in Appendix. The PLC in use had 7 inputs and 5 outputs
The test rig is essential controlled by the sensors on each actuator, the linear actuator has a sensor that is located near the top. So when the cylinder reaches the top, the sensor would detect it, then the sensor would send a signal back to the input of the plc. The signal would then travel through the PLC to its output. The output of the PLC IS connected to a solenoid valve. The object of the solenoid IS to regulate which valve of the rotary actuator will receive air so as to allow movement in the correct direction thus creating the movement needed for the knee. The rotary actuator has two sensors positioned so when the actuator rotates to the sensor it then sends a signal back to the PLC thus sending a signal to the solenoid closing one valve.
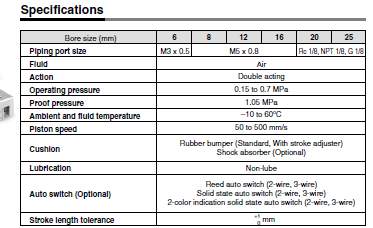
Pneumatic Actuators: As stated previously the test rig uses two pneumatic actuators, one rotary and one linear. These two actuators were sourced within GMIT. Both of these actuators were made by SMC pneumatics. The general specifications of both actuators can be seen in Appendix? The maximum operating pressure of both actuators is 0.7 Mpa, while the minimum operating pressure for the linear actuator is 0.15Mpa and the rotary actuator is 0.2Mpa. The stroke distance of the linear actuator is 100mm.
Future Work
There is a lot of work to be done on this project in the coming months.
- Readjusting the knee molds at different angles so as to recreate genu valgum and varum effect of the knee. This will be difficult to get right as results will not be completely accurate due to different variants such as the weight of a human acting done on the tibia.
- Creo drawing – I will draw up the individual parts of the rig on Creo
- Testing –
- ANSYS: Finite element analysis
- Poster
- Video
- Completion of thesis
- Completion of final presentation
This is a force sensitive resistor with a round, 0.5″ diameter, sensing area. This FSR will vary its resistance depending on how much pressure is being applied to the sensing area. The harder the force, the lower the resistance. When no pressure is being applied to the FSR its resistance will be larger than 1MΩ. This FSR can sense applied force anywhere in the range of 100g-10kg.
Two pins extend from the bottom of the sensor with 0.1″ pitch making it bread board friendly. There is a peel-and-stick rubber backing on the other side of the sensing area to mount the FSR.
https://www.sparkfun.com/products/9375?_ga=2.89048603.1022470302.1516275677-245011016.1516275677
Discussion
Conclusions of Mid-Module Report
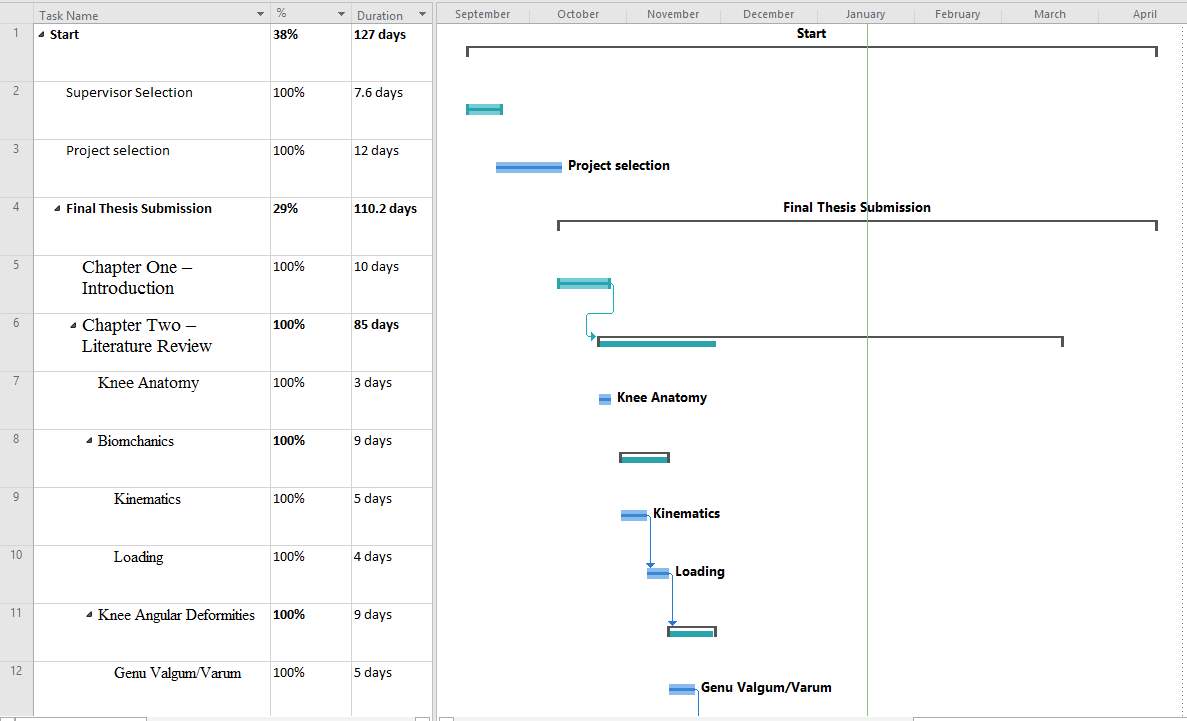
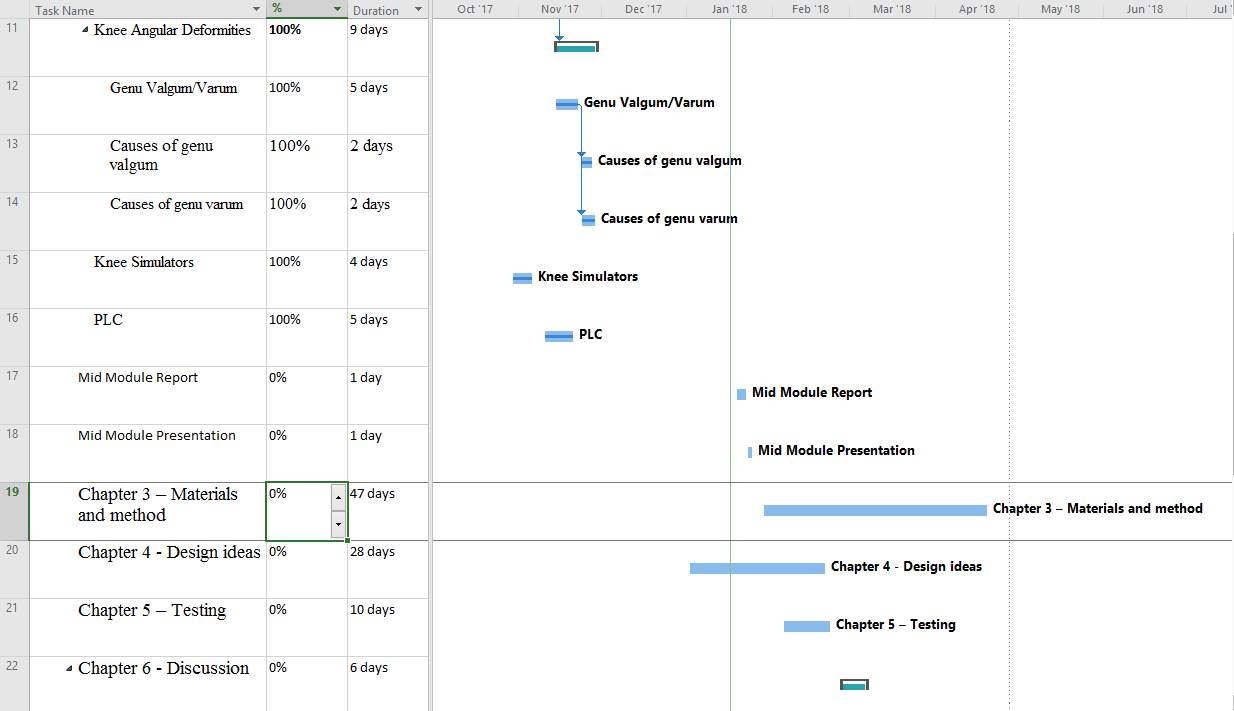
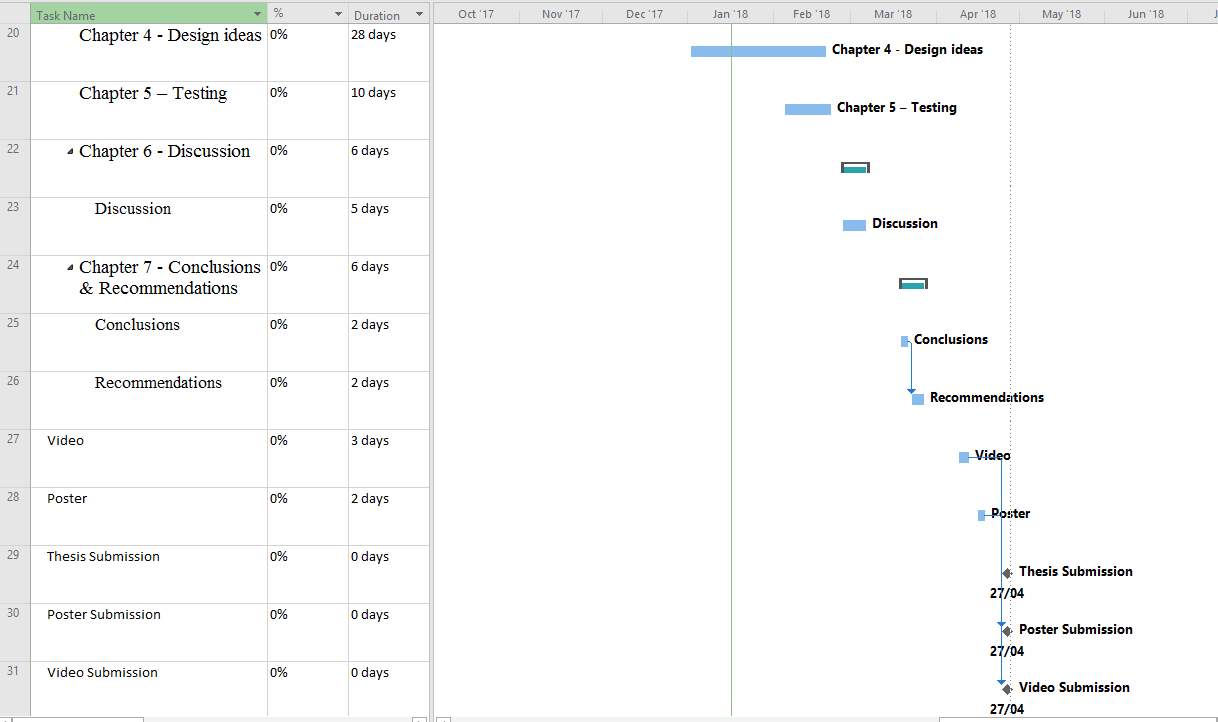
Gantt Chart and project plan
Appendices
Actuator Specifications
Rotary Actuator
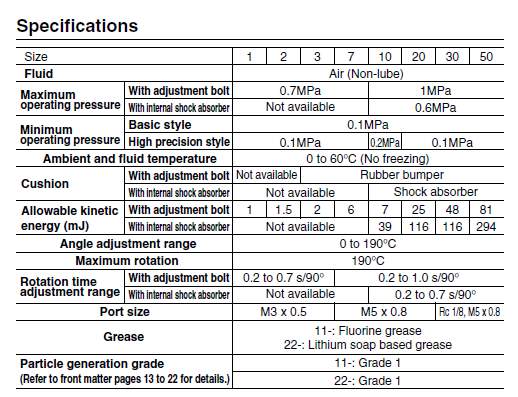
Linear Actuator
References
CLIPPINGER, K.S., 2007. Dance anatomy and kinesiology. Human Kinetics.
CRIM, J.R., MANASTER, B. & ROSENBERG, Z.S., 2017. Imaging Anatomy: Knee, Ankle, Foot E-Book. Elsevier Health Sciences.
GOLDBLATT, J.P. & RICHMOND, J.C., 2003. ‘Anatomy and biomechanics of the knee’. Operative Techniques in Sports Medicine, 11 (3), pp. 172-186.
MASOUROS, S., BULL, A. & AMIS, A., 2010. ‘(i) Biomechanics of the knee joint’. Orthopaedics and Trauma, 24 (2), pp. 84-91.
PASTIDES, P., SHENOY, R. & NATHWANI, D., 2013. ‘(iv) The patella in total knee replacement’. Orthopaedics and Trauma, 27 (6), pp. 372-378.
PATTON, K.T., 2015. Anatomy and Physiology-E-Book. Elsevier Health Sciences.
SCUDERI, G.R. & TRIA, A.J., 2010. The knee: a comprehensive review. World Scientific.
SHENOY, R., PASTIDES, P. & NATHWANI, D., 2013. ‘(iii) Biomechanics of the knee and TKR’. Orthopaedics and Trauma, 27 (6), pp. 364-371.
SOLBERG, G., 2007. Postural disorders and musculoskeletal dysfunction: diagnosis, prevention and treatment. Elsevier Health Sciences.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Physiology"
Physiology is related to biology, and is the study of living organisms and how they function. Physiology covers all living organisms, exploring how the body performs basic functions in relation to physics and chemistry.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




