Dissertation on Alcohol Screening of Acute Surgical Admissions
Info: 8896 words (36 pages) Dissertation
Published: 17th Nov 2021
Tagged: HealthHealth and Social Care
Introduction
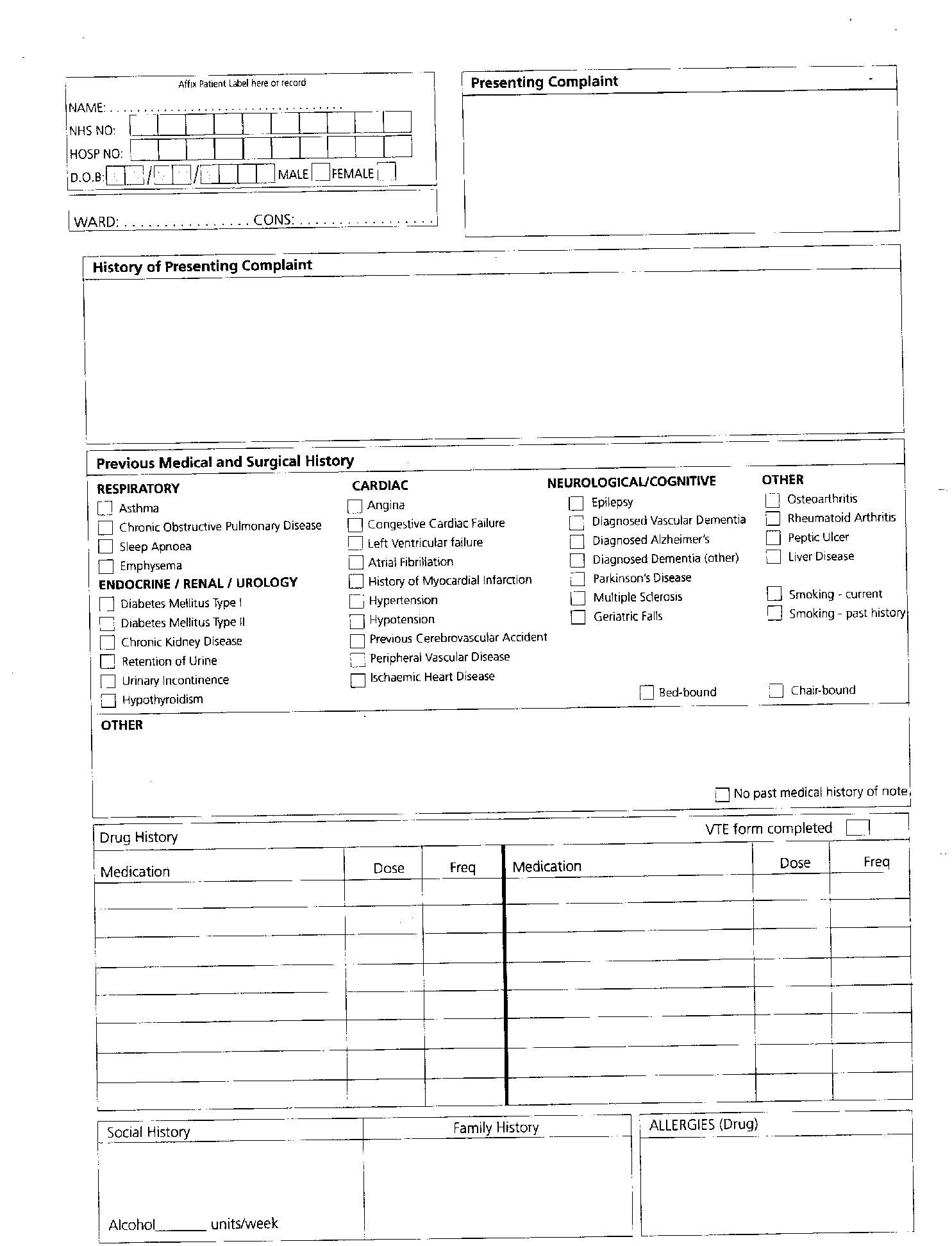
This paper will present a critical analysis of an alternative strategy for service delivery, relevant to the author’s area of practice as a Nurse Practitioner within an emergency on call surgical team in an Acute Hospital Trust. Within the Trust a large proportion of patients who are referred to the general Surgical Assessment Unit (SAU) are referred via their General Practitioner and attend directly to the unit, where the surgical on call team assess the patient using a general surgical proforma as a guide and an admission document.
Treatment plans are formed and implemented and interventions performed according to the differential diagnosis. The current proforma allows a general history to be taken from the patient but there is no formal alcohol screening tool, rather, the assessor writes the number of units in a simple box labelled alcohol (Appendix A).
This paper will discuss whether the alcohol screening and assessment process for acute surgical admission patients may be improved. It will consider an alternative strategy for alcohol screening in a Local Acute Hospital Trust rather than the current superficial screening process and develop a more comprehensive assessment. The aim will be to improve the alcohol screening and assessment process and further the provision of more effective care to those who misuse alcohol and further to identify health promotion opportunities.
In presenting this strategy, the paper considers the importance of leadership in challenging and enhancing healthcare service delivery. Continuous improvement, with the aim of achieving economy, efficiency, effectiveness and equity is an overarching focus within the NHS (The King’s Fund, 2016; NHS, 2017). Nurses and, in particular, those in senior roles, such as nurse practitioners have a responsibility to challenge, change and, ultimately, enhance service delivery through effective leadership.
Indeed, a variety of key documents including the Nursing and Midwifery Council (NMC) The Code (NMC), the Clinical Leadership Competency Framework (NHS Leadership Academy, 2011), the Five Year Forward View (NHS, 2014) and the Leading Change, Adding Value report (NHS England 2016) all emphasise nurses’ expanding leadership responsibilities.
Main Body
The health care needs of the United Kingdom (UK) have changed since the National Health Service’s (NHS) inception in 1948. The population is the largest it’s ever been at 65.6 million; people are living longer with 18% of the population being aged 65 and over and 2.4% of the population being aged 85 and over. (Office of National Statistics 2017). There is also a large number of people living with multiple co-morbidities and the Department of Health (DH) (2012) estimate that the number will rise from1.9 million in 2008 to 2.9 million in 2018, marking a large increase in the last 10 years. These all impact on increased pressure and cost to the NHS with estimates from the Department of Health that 70% of health and social care costs are attributed to people with long term conditions (DH 2012).
Traditionally, NHS leadership has been based on a paternalism with a hierarchical structure (Warriner 2009), however, the changing demographics have seen reforms and modernisation of the NHS and a gradual shift from the dominant theories and models associated with leadership in healthcare (Warriner 2009). Such changes have been driven by the recognition that traditional leadership theories may no longer be relevant in the current complex contemporary healthcare system (Warriner, 2009). Significant problems associated with poor quality care and leadership in the NHS have largely attributed to current policy changes. This was highlighted in the Mid-Staffordshire NHS Foundation Trust Public Inquiry (Francis 2013).
Contemporary leaders now utilise a more participatory leadership style (Giltinane, 2013). An example of such a leadership style is transformational leadership, where leaders seek to influence and inspire better levels of performance and subsequently the delivery of higher-quality care in those they lead (Frankel, 2008; Giltinane, 2013). The Royal College of Nurses (RCN) (2017) also highlight the importance of authentic and collective leadership theories and models in driving nurse-led quality improvements. In healthcare settings, contemporary leaders are expected to fulfil more advanced, diverse functions (Kelly, 2010), however, the author would suggest that leadership can be implemented at all grade levels as it incorporates a strive for high quality patient care that is safe and ensures that the patient remains at the centre of care, with innovation that is reactive to patients and the public’s needs (West et al 2015). Working within the NHS, it is paramount that all health care workers continually engage and challenge current services and strive to improve the quality of services and care to meet current and future demands
Alcohol Use Disorders (AUD) and misuse are a significant problem in the UK costing the NHS an estimated £3.5 billion per year (Public Health England (PHE) 2014), amounting to one of the largest contributing factors to ill health, disability and mortality with the World Health Organisation (WHO) (2014a) reporting that alcohol abuse is a causal factor in more than 200 injuries and diseases. In 2015 -2016 there were 1,119,020 admissions where alcohol was a primary or secondary cause of admission. Of these, 307,250 were wholly attributable to alcohol. A further 811,780 people were listed as having secondary conditions which included amongst others listed: cancer of the breast, oral cavity, oesophageal and bowel as well as hypertension and cardiovascular disease. Alcohol has a contributing effect to multiple conditions such as increasing the risk of heart disease, stroke and hypertension (Harrington-Dobinson and Blows 2007) and cancer has been directly linked to levels of alcohol consumption (Freedman 2007, WHO 2010a, Parkin 2011, WHO 2014b).
For the purpose of this paper and to clarify the classifications of AUD, the author will use the National Institute of Health and Care Excellence (NICE) (2010) which includes definitions for lower- risk, consuming 21units (men), 14 units (women) or less per week, increasing-risk drinking; consuming between 22–50 units per week (men), 15-35 units per week (women) and higher-risk drinking; consuming over 50 units per week (men) and 35 units per week (women). Hazardous, harmful and dependent patterns of drink are described by WHO (2007) as the following: Hazardous drinking where there is an increased risk of harm from increased alcohol consumption, Harmful drinking as a pattern of alcohol consumption that is causing mental or physical harm and dependence as continuing to drink despite harmful consequences and has a physiological and mental behavioural characteristics that include difficulty in controlling the use of alcohol and a strong desire to drink.
As well as having a significant impact on an individual’s physical and mental health, it also impacts on socioeconomic deprivation and social problems such as unemployment (Martineau 2013), family relationships (Babor et al 2010) and crime (Boden et al 2013). When loss of productivity and crime are considered, the cost to the UK from alcohol related harm according to Public Health England (2014) may be as high as £21 billion annually.
Given these figures, it is clear that the high amounts of patients admitted with AUD’s impacts heavily upon acute hospitals, already under immense pressure (Mandelberg et al 2000, NHS 2017) and, as such, have become a focus of key government programmes in reducing the impact of alcohol related health issues. It is evident that in addressing these issues there is scope to substantially reduce the cost to the NHS and wider community by providing a provision of evidence based assessment. There has been a plethora of research regarding the prevention of illness and alcohol consumption on individual and public health (Freedman 2007, WHO 1988, WHO 2014a, WHO 2014 b).
There are also other drivers of the need for improvement in the assessment of alcohol consumption in acute hospital trusts – in particular, the prevention of avoidable costs to the NHS. The King’s Fund (2015a) Better Value in the NHS report highlights the importance of continual improvements in the delivery of healthcare services in the UK.
In response, there are a number of key documents that support the need for alcohol screening/assessment in Acute Hospital Trusts. The NHS’ (2017) Next Steps on the NHS Five Year Forward View document requires provider trusts, from the period 2017/18, to screen, and deliver brief interventions and advice to people with “high alcohol consumption” and financially incentivise Trusts for doing so. The National Institute of Health and Care Excellence’s (NICE, 2011) Alcohol-Use Disorders: Diagnosis, Assessment and Management of Harmful Drinking and Alcohol Dependence guideline also highlights the importance of assessment for identification of high-risk alcohol consumption. More generally, the NICE’s (2012) Patient Experience in Adult NHS Services guideline emphasises the importance of comprehensive, individualised health needs assessment in delivering the best possible experience of care.
Quick and routine screening for alcohol-related problems within a wide range of health and social service settings has, therefore, become an important focus, with NICE producing guidelines which recommends that alcohol screening be carried out as a matter of routine practice to improve early identification and management of risky drinking behaviour (NICE, 2010). This is supported by the Home Office (2012) who have developed and implemented a national alcohol strategy in response to the impact of alcohol which focuses on reducing Alcohol related harm, with the key consideration being that assessment is required to identify people with high risk alcohol related behaviours. The NHS England (2014) guidance further reiterates the importance of an evidence base for illness prevention in public health.
Alcohol screening tools are applied in healthcare settings to identify people who engage in the high-risk consumption of alcohol, and subsequently to inform interventions to reduce the risk of alcohol-related harm (WHO 2017). THE NHS, Next Steps on the NHS Five Year Forward View document, further expresses the importance of assessment and Trusts have been given financial incentives: The new national NHS Commissioning for Quality and Innovation (CQUINs), for providing screening, brief interventions and advice to people with high alcohol consumption.
There are many alcohol assessment tools that may be used within an acute setting such as A&E (Jones, 2010). The focus of alcohol assessment tools is within the A&E setting, the author has applied these to this paper within the SAU setting as this is a mirror environment, therefore the following alcohol assessment tools will be explored:
NICE guidelines (NICE 2010) suggest the use of the following validated alcohol screening tools: Alcohol Use Disorders Identification Test (AUDIT), the Fast Alcohol Screening (FAST) or the Paddington Alcohol Test (PAT). The Modified -Single Alcohol Screening Question (M-SASQ) and CAGE tool, which is an acronym from the four questions asked are both the M-SASQ and the CAGE tool are currently used in the Local Trust’s Accident and Emergency, therefore, the author will consider the above tools for use within the SAU surgical proforma with those recommended by NICE (2010).
The current alcohol assessment used in Accident and Emergency within the Acute Trust is the M-SASQ tool (Kaner et al 2013) (Appendix B) which was adapted from the Single Alcohol Screening Question (SASQ) tool developed by Williams and Vinson (2001). It asks a single question about how often a person consumes more than the guideline-recommended number of standard drinks on a single occasion, from ‘never’ to ‘daily or almost daily’ (Kaner et al 2009, Screening and Intervention Programme for Sensible Drinking (SIPS) (SIPS 2017a).
Research suggests the M-SASQ is highly sensitive and specific for detecting problematic alcohol consumption in A&E settings (SIPS 2017a). Jones (2010) systematic review suggests that this type of short, time-efficient screening tool may be the most appropriate for A&E settings (Jones 2010), which suggests that this may also be applied in acute surgical assessment unit. However, the M-SASQ screens only for people who engage in episodic (‘binge’) drinking, overlooking people who engage in high-risk consistent but lower-level alcohol use. The author suggests that this may not be appropriate and may be inadequate both in terms of identifying high risk drinkers and it has a closed question framework that does not facilitate an open conversation, the use of yes and no answer only end, what the patient might view as, a difficult conversation.
As health professionals we have a duty to ensure that we communicate openly and effectively (NMC 2015) using open ended questions can ensure that assumptions any biases are removed (Volk 1997). (Boyd 2008). There is much more emphasis on personal health responsibility (Department of Health 2013) and people with AUD may feel judged or held responsible as there is much cultural stigma attached to social health burden conditions (Weis et al 2006), therefore, in using this tool, patients may not be as comfortable mentioning risky behaviour.
The literature reports that the most sensitive of these tools, with a higher sensitivity event than the M-SASQ tool, is the Fast Alcohol Screening Test (FAST) (Appendix C) (Jones, 2010; SIPS, 2017b). The FAST tools first question is similar to M-SASQ, although where M-SASQ considers an answer to more than monthly to be positive and a referral to the alcohol liaison service is made, the FAST tool askes three further questions regarding frequency, ability to remember events and any concerns expressed from a health professional (SIPS 2017b, which have been adapted from AUDIT, a score of three is considered positive (SIPS 2017b) A study by Hodgson et al (2001) found that out that when compared with AUDIT, FAST detected 930 out of 1000 people with alcohol misuse that AUDIT had identified.
FAST was further researched by Hodgson et al (2002) which used a large study group of 666 people across two London accident and emergency departments, it found that FAST had a high sensitivity and specificity for detecting hazardous and non- hazardous patterns of drinking and validated its use in busy clinical settings. It is useful, in that the first question has a high filter value and can detect up to 70% of hazardous drinking.
Further recommended for use by NICE (2010) is the Paddington Alcohol Test (PAT) (Appendix D). This is a much shorter tool than the FAST tool, consisting of three focused questions (Public Health England, 2008). Research has demonstrated it to be acceptably sensitive and specificy for detecting problematic alcohol consumption in A&E settings (Jones, 2010). A key strength noted with PAT is that it is a targeted screening tool, applied only to people with certain presentations and only takes under a minute to complete, it is therefore seen as time and cost-effective (Jones, 2010). The PAT is used within many A&E departments and is listed as one of the tools recommended by NICE (2010). PAT guides the assessor to deliver brief intervention for people identified to be engaging in high-risk alcohol consumption (Public Health England, 2011), whilst desirable to guide assessors to deliver brief interventions, the purpose of implementing a universal alcohol assessment tool would be to assess all patients who are admitted so this may not be appropriate to the surgical assessment unit. The NICE individual behaviour-change guidance (2014) advocates that all contact may provide an opportunity for interventions that aim to improve behaviours that lead to ill health and further state that each intervention should be person centred. Patients who are not admitted for an alcohol related injury or disease may have an existing AUD (Ryder et al 2010) or require health promotion advice which the Department of Health (2014) states that health professionals should use all contact with patients as an opportunity to provide health promotion advice.
The CAGE tool (Appendix E) (Cook 2000) was developed because it was that AUDIT was too long to use in a clinical setting. Although effective in detecting harmful and dependent AUD (Edwards et al 1982), CAGE has 71 percent sensitivity and 90 percent specificity (Dhalla, and Kopec,2007). Despite this, it does not ask about levels of consumption, frequency or length of heavy of any alcohol intake that may identify hazardous drinkers (Nilsen & Cone 1994). Cherpital (1999) study supports this finding and further adds that CAGE fails to detect low but risky drinking levels.
A comparative study (Bradley et al1998) of CAGE with AUDIT found that CAGE did perform better at identifying patients with alcohol abuse or a dependence on alcohol but that AUDIT showed a slight benefit in that it identified hazardous drinking, which was attributed to the questions regarding frequency of heavy drinking. CAGE tool is frequently used in practice although it is a closed question framework has a similar draw back to that of the M-SAQ in that it only requires yes or no answers which do not lead to an open dialogue or further discussion. Closed questions to get specific information from patients may well bring a difficult conversation to an end (Boyd, 2008).
AUDIT (Appendix F) is a tool that is also recommended by NICE (2010), it was developed by the WHO (Saunders al 1993) and is seen as the GOLD standard in assessment, it is a 10-question screening tool designed to identify heavy drinkers, alcohol-related problems and symptoms of dependence over the past year. Saunders et al (1993) states that AUDIT has a 92 percent sensitivity and 94 percent specificity in detecting harmful and hazardous drinking. It is in the style of a structured interview and can be incorporated within history taking very easily and it has the advantage that when presented to patients in this format, very few patients find the questions offensive (Babor et al 2010). In practice, however, it has been found to be relatively long to administer and relatively complex when scoring and interpreting the results (Gual et al 2002) although, to put this in perspective in the authors experience, completion would take 4-5 minutes which is supported by Moyer (2013) who’s study states that completion should only take 3 -5 minutes.
The goal of alcohol screening and assessment is that it identifies and allows responses to high-risk alcohol-related behaviours before it results in injury and/or illness (Singh et al 2017). It also allows the opportunity to provide advice and allow patients to be aware of alcohol and associated consequences (Singh et al 2017). Evidence shows that intervention in an acute hospital has a positive impact, measured by a decrease in re-admissions and a decrease in alcohol consumption Dinh-Zarr et al 2009, Hughes et al.2013, McQueen et al 2009, Nilsen et al 2008, Patton et al, 2005, Wei et al 2015) and are cost effective (Barrett et al 2006, Burton et al (2016).
Working within the SAU, Nurse Practitioners are often the first person to assess patients on admission and the author feels that they are well placed in the assessment and subsequent management of patients who engage in high- risk alcohol-related behaviours (Rizer & Lusk, 2017). Currently if patients are assessed as having a AUD, they are referred to the Alcohol liaison nurse for advice, brief intervention, or referral. This is a service that has been highly successful, although the author has observed that current demand outweighs the services that can be provided. Only 58% of hospitals in the UK have access to an alcohol specialist support service and 25% of these are not available outside of office hours (Anderson et al 2013). Pollini et al (2006) suggest that motivation may be higher and advice may have more meaning during an acute illness It would suggest that screening and assessment is essential on admission when otherwise it may be a missed opportunity.
The author suggests that the alcohol assessment process can potentially be extended to include opportunistic advice to those who are lower risk. Rizer & Lusk (2017) agree that nurses have an important role in brief intervention for alcohol consumption (Rizer & Lusk, 2017). This is underpinned that Nurse Practitioners often have frequent contact with patients throughout their admission and may develop a more therapeutic relationship than those of their medical counterparts, furthermore, the delivery of brief intervention can be conceptualised as a natural, and sensible, extension of the assessment role. The aims of brief intervention and advice are to use the results of an alcohol consumption assessment to ensure, where appropriate, that patients are aware about the risks associated with their alcohol consumption, and motivate behavioural changes to reduce these risks (Singh et al 2017).
Vadlamudi et al. (2008: p. 290) argues that failure to use alcohol assessment results to identify those that may need referral for brief interventions or further counselling “raises serious ethical and quality-of-care concerns”. Additionally, the delivery of brief interventions is a key aspect the health promotion role, however, it must be noted that few studies consider nurse-led brief interventions specifically. Two systematic reviews were found which suggest nurse-led brief interventions for alcohol consumption are just as effective as those led by physicians (Joseph et al 2014, Platt et al 2016).
The introduction of changes in relation to alcohol screening and assessment in practice, may represent a variety of challenges both for leaders and for staff in acute hospital trust settings. The literature suggests that paucity of time and lack of an appropriate space to undertake alcohol screening are key barriers to effective alcohol screening in acute healthcare settings (Johnson et al., 2011). Nygaard and Aasland (2011) conceptualise this slightly differently, suggesting that there are often difficulties integrating new alcohol screening processes into well-established practice routines. These barriers may be exacerbated by the introduction of a longer screening process; they must be addressed at the organisational level – for example: by changing the duration, location and standard content of nurse consultations.
Time restraints are an important consideration when considering the challenge in the implementation of brief intervention by practitioners in practice (Berends & Roberts, 2012). The author argues that brief interventions typically involve a single session of 5 minutes’ and up to 15 minutes’ duration between a patient and a Nurse Practitioner, which may take place at any point in a patient’s presentation to a healthcare setting (Rizer & Lusk, 2017; Singh et al., 2017). Derges et al. (2017) consider time barriers more broadly, suggesting that a lack of support from a healthcare setting – including lack of provision of time (often due to work overload), but also lack of role clarity, education resources and referral options all prevent nurses implementing brief screening for patients engaging in high-risk alcohol consumption.
Skinner et al. (2009) suggests that creating and maintaining an enthusiastic attitude among nurses towards the delivery of brief interventions is unlikely if healthcare settings do not value and support such practices. This again reinforces the importance of effective leadership if changes to practices related to the assessment of alcohol consumption are to be effective. As noted earlier in this paper, one of the fundamental roles of a leader in a healthcare setting is to create a culture within that setting conducive to positive changes (The King’s Fund, 2015b). The literature suggests this can be achieved by, for example, promoting effective team-working, collaborative goal-setting and utilising participatory leadership practices (The King’s Fund, 2017).
Conclusion
This paper has presented a critical analysis of how alcohol screening and assessment on an acute surgical assessment unit in an acute hospital Trust may be improved. It has discussed several alcohol assessment tools available that may be implemented and used within the surgical admission proforma and to assist in the identifications of those that require health promotion advice, brief interventions and referral to the alcohol liaison service.
It is important that all patients have an alcohol assessment using an alcohol assessment tool to identify people who have an AUD, who engage in high risk consumption of alcohol, inform interventions and referrals to reduce the risk of alcohol-related harm and subsequently enable Nurse Practitioners to fulfil their health promotion role. Current screening processes in the acute hospital Trust where the author is employed as a nurse practitioner – involving single, open-ended question on a simple proforma tool – are inadequate.
A number of alternative tools for alcohol screening in SAU settings were considered. It is clear that using an alcohol screening tools is effective and evidence shows that it can increase the number of excessive alcohol users identified and when referred can encourage to be used to help people reduce their alcohol and is in keeping with the current government agenda to prevent and reduce alcohol harm.
The M-SASQ tool is currently used in the Local Acute Trust Accident and Emergency department, it is as a short and time-efficient tool, this is appropriate for A&E settings, and it is also highly sensitive / specificity for detecting problematic alcohol consumption (Jones, 2010; SIPS, 2017a). The author feels The AUDIT tool has shown to have a more open approach and a higher sensitivity and specificity for detecting a variety of AUDs, although this should still be used as a guide as critical thinking is essential in accessing the patient (Cottrell, 2011). This will be put forward for a trial period at local SAU where the author is based.
This paper also shown initial screening may be extended beyond the initial assessment for high-risk alcohol consumption to include health promotion advice and the delivery of brief intervention. The delivery of brief interventions is a natural extension of the Nurse Practitioner’s role in alcohol consumption assessment. Nurses are well-paced to deliver such intervention, and it is a key aspect of their health promotion role. Furthermore, to respond to the increasing complexities in the healthcare system, nurses are now expected to be able to perform advanced tasks such as the delivery of brief interventions (Rizer & Lusk, 2017). Having a multidisciplinary approach to screening and assessment that patients receive the best possible care (Owen et al 2017) and may alleviate some of the burden on the alcohol liaison services.
This paper demonstrates that there are multiple complex barriers associated with the nurse’s assessment, brief intervention and advice-giving role for people engaging in high-risk alcohol consumption. These issues highlight the importance of effective leadership in challenging, changing and enhancing service delivery which are key responsibilities of all nurses, and nurse leaders in particular. The ultimate aim of leadership is to ensure direction, commitment and to develop a culture within a healthcare setting necessary for the delivery of continually-improving, high-quality healthcare (The King’s Fund, 2015b). Throughout this paper, the author has reflected on strategies they can use in their own leadership practice to challenge, change and enhance service delivery in relation to the implementation of changes to alcohol consumption screening practices specifically, and other practice-related changes generally.
References
Anderson W, Sir Gilmore I, Bauld L, Bellis M, Brown KA, Drummond C, Gillan E, Hastings G, Hughes E, Irving C, Parsons H, Atwarg H, Langford A, Ludbrook A, Purves R, Stead M (2013) Health First: An evidence-based alcohol strategy for the UK. University of Stirling. Available at: https://www.stir.ac.uk/media/schools/management/documents/Alcoholstrategy-updated.pdf. Accessed on 23rd December 2017.
Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham, K, (2010) Alcohol: No Ordinary Commodity. Research and Public Policy 2nd Edition, Oxford University Press. Oxford.
Barrett, B. Byford S, Crawford MJ, Patton R, Drummond C, Henry JA, Touquet R. (2006) Cost-effectiveness of screening and referral to an alcohol health worker in alcohol misusing patients attending an accident and emergency department: A decision making approach. Drug and Alcohol Dependency. 81 (1): 47-54
Berends, L & Roberts, B (2012), Implementation effectiveness of an alcohol-screening and intervention project at two hospitals in regional Victoria, Australia. Contemporary Drug Problems. 39 (2) pp. 289-309.
Boden, JM., Fergusson DM, Horwood LJ ( 2013) Alcohol misuse and criminal offending: findings from a 30-year longitudinal study. Drug and Alcohol Dependence. 128 (1-2) pp. 30 – 36. DOI: 10.1016/j.drugalcdep.2012.07.014.
Boyd, MA (2008). Psychiatric Nursing: Contemporary Practice. Wolters Kluwer Health. London.
Bradley AK, Bush KR, McDonell MB, Malone T Fihn (1998) Screening for Problem Drinking Comparison of CAGE and AUDIT, Journal of General Internal Medicine. 13 (6) pp.379-389. doi:10.1046/j.1525-1497.1998.00118.x.
Burton R. Henn Cm Lavoie, O’Connor R, Perkins C, Sweeney K, Greaves F, Ferguson B, Beynon C, Belloni A, Musto V, Marsden J, Sheron N, Wolff A. (2016). The Public Health Burden of Alcohol and the Effectiveness and Cost-Effectiveness of Alcohol Control Policies: An Evidence Review. Public Health England. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/583047/alcohol_public_health_burden_evidence_review.pdf. Accessed on 3rd December 2017.
Cook, C.C.H., (2000) Prevention and treatment of Wernicke-Korsakoff syndrome. Alcohol & Alcoholism, 35 (Suppl. 1): pp. 19-20. doi: 10.1093/alcalc/35.Supplement_1.19
Cottrell, S (2011) Critical Thinking Skills. Developing Effective Analysis and Argument. 2nd Edition, Palgrave Macmillan. Basingstoke
Department of Health (2012) Long Term Conditions Compendium of Information Third Edition. Department of Health. London. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216528/dh_134486.pdf. Accessed on 3rd December 2017.
Derges, J, Kidger, J, Fox, F, Campbell, R, Kaner, E & Hickman, M (2017), Alcohol screening and brief interventions for adults and young people in community-based settings: A qualitative systematic literature review. BMC Public Health. 17 (1) (562). doi: 10.1186/s12889-017-4476-4.
Dhalla, S, Kopec, JA (2007) The CAGE questionnaire for alcohol misuse: a review of reliability and validity studies. Clinical and investigative medicine. 30 (1) pp. 33 – 41. Academic Search Complete.
Dinh-Zarr, TB, Goss, CW, Heitman, E, Roberts, IG & DiGuiseppi, C (2009), Interventions for preventing injuries in problem drinkers. Cochrane Database of Systematic Reviews. 3. doi: 10.1002/14651858.CD001857.pub.
Edwards G, Arif A, Hodgson R (1982) Nomenclature and classification of drug and alcohol related problems: a WHO Memorandum. World Health Organisation Bulletin. 59 (2) pp. 225–42. Pub Med.
Francis, R (2013), Report of the Mid-Staffordshire NHS Foundation Trust Public Inquiry, Available at: http://webarchive.nationalarchives.gov.uk/20150407084949/http://www.midstaffspublicinquiry.com/sites/default/files/report/Executive%20summary.pdf.
Accessed on 8th December 2017.
Frankel, A (2008) What leadership styles should senior nurses develop? Nursing Times. (104) 35. pp. 23-24.
Freedman, N. D. (2007) Alcohol and head and neck cancer risk in a prospective study. British journal of cancer. 96 (9) pp. 1469 – 1474. doi: 10.1038/sj.bjc.6603713.
Giltinane, CL (2013), Leadership styles and theories, Nursing Standard (27) 41. pp. 35-39.
Gual A, Segura L, Contel M, Heather N, Colom J (2002) Audit -3 and Audit -4: Effectiveness of Two Short Forms of the Alcohol Use Disorders Identification Test. Alcohol and Alcoholism. 37 (6) pp. 591 – 596. doi.org/10.1093/alcalc/37.6.591.
Harrington-Dobinson A, Blows W (2007) Substance misuse. Part 1: nurses’ guide to alcohol and promoting healthy lifestyle changes. British journal of nursing. 15 (22) pp.1217 – 1219. doi: 10.12968/bjon.2006.15.22.22558.
Hodson R, Alwyn T., John, B., Thom, B., Smith A. (2012) THE FAST ALCOHOL SCREENING TEST. Alcohol and alcoholism. 37 (1) pp. 61 – 66. doi:10.1093/alcalc/37.1.61
Hodgson, R. Alwyn, T. John, B., Thom, B. & Smith, A. (2001) The FAST Alcohol Screening test. Alcohol and Alcoholism, 37 (1) pp. 61 – 66.
Home Office (2012), The Government’s Alcohol Strategy. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/224075/alcohol-strategy.pdf. Accessed on 15th December 2017.
Hughes NR, Houghton N, Nadeem H, (2013) Salford alcohol assertive outreach team: a new model for reducing alcohol-related admissions. Frontline Gastroenterology 4:130–4. DOI: 10.1007/s11606-014-2968-9.
Johnson, M, Jackson, R, Guillaume, L, Meier, P & Goyder, E (2011), Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: A systematic review of qualitative evidence, Journal of Public Health, vol. 33, no. 3, pp. 412-421.
Jones, LA (2010), Systematic review of alcohol screening tools for use in the emergency department, Emergency Medicine Journal. Available at: http://emj.bmj.com/content/28/3/182.long. Accessed 8th December 2017.
Joseph, J, Basu, D, Dandapani, M & Krishnan, N (2014), Are nurse-conducted brief interventions (NCBIs) efficacious for hazardous or harmful alcohol use? A systematic review, International Nurse Review. 61 (2) pp. 203-210.
Kaner, E, Coulton, S, Gilvarry, E, Godfrey, C, Myls, J, Oyefeso, A, Perryman, K & Sepherd, J (2013), Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): Pragmatic cluster randomised controlled trial. British Medical Journal. (346) 8501.pp. 540 – 548. Doi:10.1093/alcalc/agu046.
Kaner, E, Martin, C, Paul, C, Simon, D, Paolo, D, Colin, G, Eilish, G, Godfrey, C, Heather, N, Mules, J, Newbury-Birch,D, Oyefeso, A, Parrott, S, Perryman, K, Phillips, T, Shenker, T & Shepherd, J (2009), Screening and brief interventions for hazardous and harmful alcohol use in primary care: A cluster randomised controlled trial protocol, BMC Public Health. 9 (1) pp. 287-299. doi:org/10.1186/1471-2458-9-287
Kelly, P (2010), Essentials of Nursing Leadership and Management (2nd Edition.), Delmar Cengage Learning. Clifton Park, New York.
Mandelberg, J.H., Kuhn, R.E., & Kohn, M.A. (2000). Epidemiologic analysis of an urban, public emergency department’s frequent users. Academic Emergency Medicine, 7, 637–646. doi:10.1111/j.1553-2712.2000.tb02037.x
Martineau F, Tyner E, Lorenc T, Petticrew M, Lock K. (2013) Population-level interventions to reduce alcohol-related harm: an overview of systematic reviews. Preventative Medicine. 57 (4) pp. 278 – 96.
McQueen, J, Howe, TE, Allan, L & Mains, D (2009), Brief interventions for heavy alcohol users admitted to general hospital wards. Cochrane Database of Systematic Reviews. 8. doi: 10.1002/14651858.CD005191.pub
Moyer V (2013) Screening and behavioural counselling interventions in primary care to reduce alcohol misuse: clinical summary of US Preventive Services Task Force recommendations. Annals of Internal Medicine. 159 (3) pp. 210-218.
National Institute of Health and Care Excellence (2010) Alcohol-use disorders: prevention Public health guideline [PH24] Available at: https://www.nice.org.uk/guidance/ph24/chapter/glossary#alcohol-related-harm Accessed on 13th December 2017
National Institute of Health and Care Excellence (2011) Alcohol-use disorders: diagnosis, assessment and management of harmful drinking and alcohol dependence guidance [CG115] Available at: https://www.nice.org.uk/guidance/cg115. Accessed 29th November 2017.
National Institute for Health and Care Excellence (NICE) (2014) Behaviour change: individual approaches [PH49] Available at: http://www.makingeverycontactcount.co.uk/media/1020/01_nice-behaviour-change-individual-approaches.pdf. Accessed on 15th December 2017.
National Institute for Health and Care Excellence (NICE) (2012), Patient Experience in Adult NHS Services: Improving he Experience of Care for People using Adult NHS Services. Available at: https://www.nice.org.uk/guidance/cg138. Accessed on 29th November 2017.
Nilsen P, Baird J, Mello MJ, Nirenberg T, Woolard, Bendtsen P, Longabaugh R (2008) A systematic review of emergency care brief alcohol interventions for injury patients. Journal Substance Abuse Treat. 35 (2) pp.184 – 201.
Nygaard P, Aasland G (2011) Barriers to Implementing Screening and Brief Interventions in General Practice: Findings from a Qualitative Study in Norway. Alcohol and alcoholism (Oxford) 46 (1) pp. 52 – 60. doi: 10.1093/alcalc/agq07.
Parkin, D.M. (2011) Cancers attributable to the consumption of alcohol in the UK in 2010. British Journal Cancer. 106(2) 14- 18. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3252062/ . Accessed on 2nd December 2017.
Public Health England (2014), Alcohol Treatment in England: 2013-14. Available from: http://www.nta.nhs.uk/uploads/adult-alcohol-statistics-2013-14-commentary.pdf. Accessed on 30 November 2017.
Public Health England (2008), Fast Alcohol Screening Test (FAST). Available at: https://www.alcohollearningcentre.org.uk/Topics/Latest/Fast-Alcohol-Screening-Test-FAST/. Accessed on 12th December 2017.
Public Health England (2011), Paddington Alcohol Test 2011. Available at: https://www.alcohollearningcentre.org.uk/_assets/PAT_2011_Paddington_Alcohol_Test.pdf. Accessed on 12th December 2017.
Rizer, CA & Lusk, DM (2017), Screening and initial management of alcohol misuse in primary care, Journal for Nurse Practitioners. 13, (10) pp. 660-666.
National Health Service (2014) THE FORWARD VIEW INTO ACTION: PLANNING FOR 2015/16. Public Health England. Available at: https://www.england.nhs.uk/wp-content/uploads/2014/12/forward-view-plning.pdf. Accessed on 2nd December 2017.
National Health Service Leadership Academy (2011), Clinical Leadership Competency Framework, NHS Leadership Academy, London. Available from: http://www.leadershipacademy.nhs.uk/wp-content/uploads/2012/11/NHSLeadership-Leadership-Framework-Clinical-Leadership-Competency-Framework-CLCF.pdf. Accessed on 21st December 2017.
National Health Service England (2016), Leading Change, Adding Value. Available from: https://www.england.nhs.uk/wp-content/uploads/2016/05/nursing-framework.pdf. Accessed 12st December 2017.
National Health Service (NHS) England (2017), Next Steps on the NHS Five Year Forward View. Available from: https://www.england.nhs.uk/wp-content/uploads/2017/03/NEXT-STEPS-ON-THE-NHS-FIVE-YEAR-FORWARD-VIEW.pdf. Accessed 8th December 2017.
Nursing and Midwifery Council (2015), The Code: Professional Standards of Practice and Behaviour for Nurses and Midwives. Nursing and Midwifery Council. Available at: https://www.nmc.org.uk/standards/code/. Accessed on 15th December 2017.
Office of National Statistics (2017) Overview of the UK population: July 2017
An overview of the UK population, how it’s changed, what has caused it to change and how it is projected to change in the future. The UK population is also compared with other European countries. Office of National Statistics. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/july2017. Accessed on 29th December 2017.
Owens L, Patterson K, King P Richardson A (2017) multidisciplinary team (MDT) approach to managing alcohol-dependent patients with comorbid depression in an acute hospital setting. European Psychiatry. 41, Supplement. pp.393.
Patton, R., Hilton, C., Crawford, M.J. & Touquet, R (2005) The Paddington Alcohol Screening Test: A short report. Alcohol and Alcoholism. 39 (3) 266–268. doi.org/10.1093/alcalc/agh049.
Platt L, Melendez-Torres GJ, O’Donnell A (2016) How effective are brief interventions in reducing alcohol consumption: do the setting, practitioner group and content matter? Findings from a systematic review and meta-regression analysis. Available from: http://bmjopen.bmj.com/content/6/8/e011473. Accessed on 5th December 2017.
Pollini, R.A. O’Toole TP, Ford D, Bigelow G. (2006) Does this patient really want treatment? Factors associated with baseline and evolving readiness for change among hospitalized substance using adults interested in treatment. Addictive Behaviours 31 pp. 1904-1918.
Royal College of Nursing (RCN) (2017), Leadership. Royal College of Nursing. Available at: https://www.rcn.org.uk/clinical-topics/clinical-governance/leadership. Accessed on 15th December 2017.
Ryder S D, Aithal GP, Holmes M, Burrows M, Wright N R. (2010) Effectiveness of a nurse-led alcohol liaison service in a secondary care medical unit. Clinical Medicine (10) pp. 435 – 4. doi: 10.7861.
Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addiction. 88 (6) pp.791 – 14. doi: 10.1111/j.1360-0443.1993.tb02093.x.
Screening and Intervention Programme for Sensible Drinking (SIPS) (2017b), Fast Alcohol Screening Test (FAST). Available at: https://www.sips.iop.kcl.ac.uk/fast.php. Accessed on 17th December 2017.
Screening and Intervention Programme for Sensible Drinking (SIPS) (2017a) M-SASQ, Available from: https://www.sips.iop.kcl.ac.uk/msasq.php. Accessed on 17th December 2017.
Singh M, Gmyrek A, Hernandez A, Damon D, Hayashi S (2017) Sustaining screening, brief intervention and referral to treatment (SBIRT) services in health-care settings. Addiction, 112 (Supplement). pp. 92-100. doi: 10.1111/add.13654.
Skinner, N, Roche, AM, Freeman, T & McKinnon, A (2009), Health professionals’ attitudes towards AOD-related work: Moving the traditional focus from education and training to organisational culture. Drug: education, prevention & policy. 16 (3) 232-249. doi: 10.1080/09687630902876338.
The King’s Fund (2015a), Better Value in the NHS: Report Summary, Kings Fund. Available at: https://www.kingsfund.org.uk/publications/better-value-nhs/summary?gclid=CO2cj-GFocgCFSeK2wodP9sEqw. Accessed on 18th December 2017.
The King’s Fund (2017), Improving NHS Culture. The Kings Fund. Available at: https://www.kingsfund.org.uk/projects/culture. Accessed 7th December 2017.
The King’s Fund (2016), Improving Quality in the English NHS: A Strategy for Action. The Kings Fund. Available from: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/Improving-quality-Kings-Fund-February-2016.pdf. Accessed 12st December 2017.
The King’s Fund (2015b), Leadership and Development in Health Care: The Evidence Base. Kings Fund. Available at: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/leadership-leadership-development-health-care-feb-2015.pdf. Accessed 15th December 2017.
Vadlamudi, RS, Adams, S, Hogan, B, Wu, T & Wahid, Z (2008), Nurses’ attitudes, beliefs and confidence levels regarding care for those who abuse alcohol: Impact of educational intervention, Nurse Education in Practice. 8. pp. 290-298.
Volk,J R(1997). Item Bias in the CAGE Screening Test for Alcohol Use Disorders. Journal of General International Medicine. 12 (12) pp.763–769. doi: 10.1046/j.1525-1497.1997.07162. x.
Warriner, S (2009) Midwifery and nursing leadership in the ever-changing NHS. British Journal of Midwifery. 17 (12) pp. 764-768. doi: 10.12968/bjom.2009.17.12.45544.
Wei J, Defries T, Lozada M, Young N, Huen W, Tulsky J (2015) An inpatient treatment and discharge planning protocol for alcohol dependence: efficacy in reducing 30-day readmissions and emergency department visits. Journal of general internal medicine 30 (3) pp. 365–70. doi:10.1007/s11606-014-2968-9.
Weis MG, Ramakrishna J, Somma D (2006) Health-related stigma: rethinking concepts and interventions. Psychology, Health & Medicine. 11 (3) pp. 277-87. doi: 10.1080/135485006005950.
West, M., Armit, K., Loewenthal, L., Eckert, R., West, T. and Lee, A. (2015) Leadership and Leadership v Development in Healthcare: The Evidence Base. London, Faculty of Medical Leadership and Management. Available at: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/leadership-leadership-development-health-care-feb-2015.pdf. Accessed on 25th November 2019.
Williams, R & Vinson, DC (2001), Validation of a single screening question for problem drinking, Journal of Family Practice. 50 (4) pp.307-312. Academic Search Elite.
World Health Organisation (2014a) Global status report on alcohol and health 2014. Geneva, Switzerland: World Health Organisation, pp.11-13. Available at: http://apps.who.int/iris/bitstream/10665/112736/1/9789240692763_eng.pdf?ua=1. Accessed 17th December. 2017
World Health Organisation, International Agency for Research on Cancer (2010). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. VOLUME 96 Alcohol Consumption and Ethyl Carbamate. World Health Organisation. LYON, FRANCE. pp.16 – 24. Available at: https://monographs.iarc.fr/ENG/Monographs/vol96/mono96.pdf. Accessed on 17th December. 2017.
World Health Organisation, International Agency for Research on Cancer (2014b) World Health Organisation. pp.77-80. Available at: http://file:///C:/Users/mail/Desktop/University%20Masters/Challenging%20and%20enhancing%20Health%20Care/Assignment/World%20Cancer%20Report.pdf. Accessed on 17th December 2017.
World Health Organisation (2007) World Health Organisation – International Classification of Diseases, chapter V, F00-F99, mental and behavioural disorders due to psycho active substance use. Available at; http://apps.who.int/classifications/apps/icd/icd10online/ Accessed 16th December 2017.
World Health Organisation (2017), Screening and Brief Intervention for Alcohol Problems in Primary Health Care. Available at: http://www.who.int/substance_abuse/activities/sbi/en/. Accessed 8th December 2017.
World Health Organisation (WHO) (1988). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Alcohol drinking. Lyon: International Agency for Research on Cancer. Available at: https://monographs.iarc.fr/ENG/Monographs/vol96/mono96.pdf. Accessed on 12th December 2017.
Appendices
Appendix A
Local Surgical Assessment Proforma
Appendix B
The M-SASQ (single alcohol screening question)
Based on Williams and Vinson (2001)
Is this incident related to alcohol Y/N?
If so, over the last year, how often have you had 6 or more alcoholic drinks on a single occasion:
Never / Monthly / Weekly / Daily?
If monthly or more offer referral to the alcohol liaison nurse
Appendix C
Fast Alcohol Assessment Tool
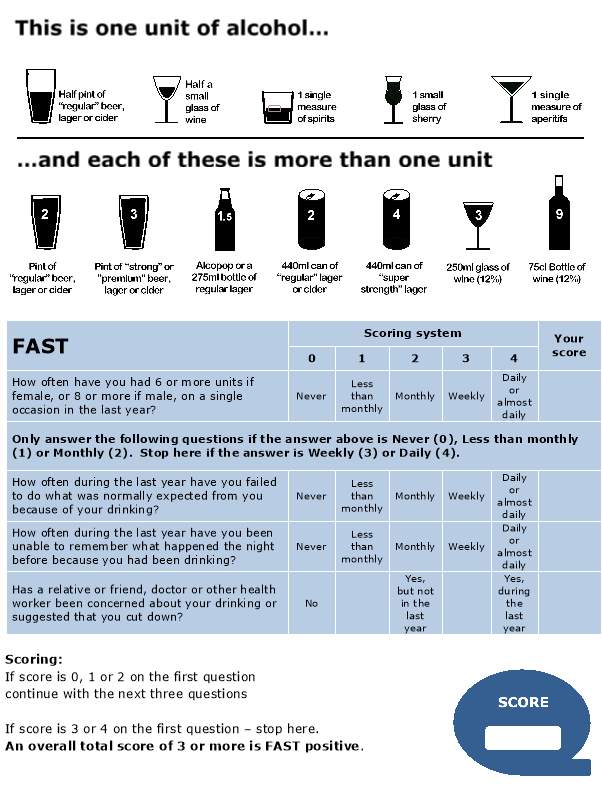
(SIPS 2017b)
Appendix E
The CAGE Questionnaire
CAGE is an acronym derived from four questions:
Have you ever felt you should cut down on your drinking?
Have people annoyed you by criticising your drinking?
Have you ever felt bad or guilty about your drinking?
Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (eye opener)?
The CAGE takes only a minute to complete and has been a widely used screening test in clinical practice, The items are easy to remember and can be administered orally by a practitioner.
Asking patient to restrict answers to last 6 months can give a clearer picture of current situation.
A positive reply to 2 or more questions warrants closer questioning of alcohol
(Cook 2000)
Appendix F
Alcohol Use Disorders Identification Test AUDIT
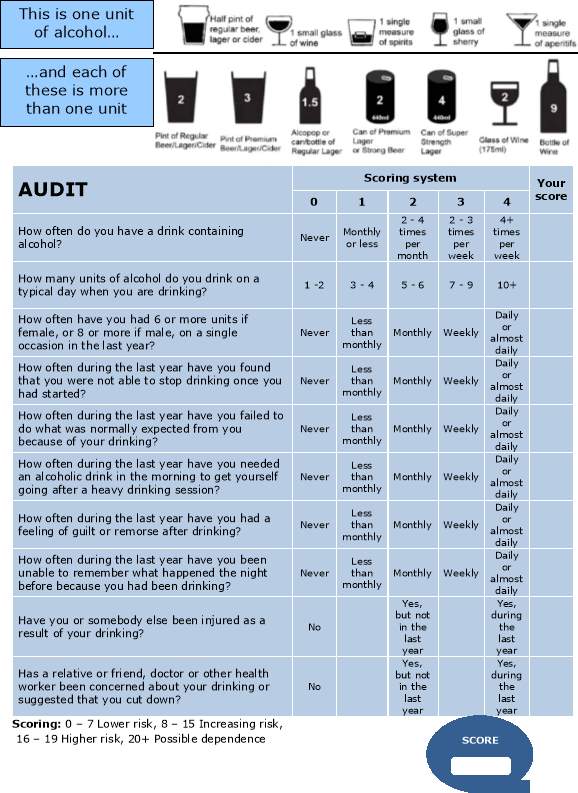
(Saunders et al 1993)
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Health and Social Care"
Health and Social Care is the term used to describe care given to vulnerable people and those with medical conditions or suffering from ill health. Health and Social Care can be provided within the community, hospitals, and other related settings such as health centres.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




