The Effects of Religiosity and Spirituality on Depressed Adults
Info: 9124 words (36 pages) Dissertation
Published: 28th Feb 2022
Tagged: PsychologyReligionMental Health
Abstract
Purpose/Objectives: The purpose of this paper is to determine the effects of religiosity and spirituality on depressed adults.
Background/Rationale: The number of people with depression continues to rise as mental health is gaining more awareness. According to World Health Organization (2017), there are more than 350 million people who currently suffer from depression. Treatment options are available but a holistic approach is what is needed.
Description of the Project/Innovation: The study of the literature will be conducted to determine the association of religiosity and spirituality with depression. In addition, using the Holistic Model of Nursing, the Psychiatric Mental Health Nurse Practitioner (PMHNP) will incorporate a religiosity and spirituality scale in an outpatient mental health setting. This scale will be implemented on current and new depressed adults, and the effectiveness will be measured at 3 months with a depression scale. The goal is for the client to have a reduction in depression symptomology or be symptom free.
Interpretation/Conclusion: The research suggests that assessing spirituality and encouraging spiritual discussion may improve depression. Based on this association, a religiosity and spirituality scale was developed, along with a plan to implement this intervention in the outpatient mental health clinic.
Implication: If this scale demonstrates success in reducing depressive symptomology, then it needs to be implemented within all other locations of the mental health clinic. Future research needs to be done to attest this intervention.
Background and Significance
Mental health disorders are on the rise and they are becoming a pressing issue. In the United States 1 in 5 adults experienced a mental disorder in 2015 (National Alliance on Mental Illness [NAMI], 2017). This number encompasses several disorders ranging from anxiety, schizophrenia, attention deficit hyperactivity disorder (ADHD) to mood disorders, but the one condition that has been gaining immense attention is depression. Depression is the number one cause of disability in adults with mental health illness (World Health Organization [WHO], 2017).
Currently, there are over 350 million people who suffer from depression worldwide (WHO, 2017). United States has more than 16 million adults who have had a depressive episode in 2015 (NAMI, 2017). While that number is only a fraction of the 350 million, it is however 6.7% of the United States population (WHO, 2017). This number is increasing because depression is gaining attention and awareness as it is seen more as a comorbid condition for both mental and physical conditions.
Depression affects one physically, emotionally, and socially. Weight changes, fatigue, insomnia, and concentration are some symptoms that make up the physical component of depression, whereas, depressed mood, irritability, anger, restlessness, loss of interest, and suicidal ideation make up the psychological component (American Psychiatric Association, 2013). This symptomatology leads to a socially withdrawn behavior. Out of these common symptoms, the one that raises red flags is the suicidal ideation. Suicidal ideation is common among depressed patients and it may lead to suicidal attempts and even completion of suicide. When the risk of suicide is 25 times greater in depressed patients than general population, and the lifetime risk of suicide among depressed patients being 15%, this warrants a great deal of urgency (American Association of Suicidology, 2014).
The current practice of treating depression entails the use of psychotherapy and psychopharmacology. Psychotherapy is the therapy provided by a licensed mental health professional which aims to resolve beliefs, thoughts, social skills, self-esteem and emotional issues (Sadock, Sadock, & Ruiz, 2015). This evidence-based approach is the first line of therapy for not just depression but any mental health illness. This therapy is provided in multiple mental health settings such as hospitals, clinics, school, and even home.
The second line of therapy is psychopharmacology. The psychopharmacology approach includes the use of psychotropic medications or medications that are prescribed to treat mental health disorders. They are mainly prescribed by primary care physicians, psychiatrists, nurse practitioners, and physician assistants once a thorough assessment of the patient is performed. These medications act on the brain to affect the mind, emotions, and behavior. According to recent poll, approximately 1 in 5 American adults take 1 psychiatric medication (Medscape, 2011). With advances in the pharmacology field, safer medications are being made with less severe side effect profile. This gives patients alternatives on what they are taking and what effects to expect in their treatment plan.
Although there have been advances in treating depressed patients with medications and evidenced based psychotherapies, there is work to be done. Stressful life style, negative cognition style, and lack of social support lead to patients relapsing (Burcusa & Iacono, 2007). For some, medications and therapy is only effective for a short time, while for others, they just have not found this treatment plan of medications and therapy to be effective. This leads to significant impairment of their work, social life, overall functioning, and in severe cases even death (Burcusa & Iacono, 2007). Hence, Patten (2013) recommends a strategy that focuses long-term treatment to reduce recurrence, and ultimately, burden of depression.
One key component has been missing in the treatment plan for the depressed patients. Since depression does not have one single cause, it needs to be addressed with a holistic approach. This approach includes a thorough assessment of religiosity and spirituality. Religiosity and spirituality have been neglected in mental health due to the predominance of the medical model. However, the WHO defines health as a combination of mental, physical, and social well-being (D’Souza & George, 2006). For patients who have been struggling to cope with their mental conditions, religiosity and spirituality has served a greater purpose in their lives (Patten, 2013). There has been trending research on the importance of incorporating spirituality and religiosity in treatment plan for superior outcome (Peslow et al., 2014).
The central aim for this paper is to explore research on religiosity and spirituality and how it impacts depressed patients in the adult population. The other objective will be to propose a spiritual assessment for this population which can be utilized by various mental health settings. After seeing multiple depressed adults in an outpatient setting, the proposed spiritual assessment will focus primarily on outpatient behavioral health clinic such as Pacific Clinics. Here the client can call in, make an appointment, see their provider, and receive treatment immediately. Pacific Clinic sees clients from all walks of life and their goal is to make them functional. The team comprises of psychiatrists, Psychiatric Mental Health Nurse Practitioner (PMHNP), therapists, case managers, nurses, and directors.
I believe that spirituality has a direct link to positive psychological attitude. Spurr & Walker (2013) stated that “spirituality as a dimension of wellness, an awareness of a being or force that transcends and gives a deep sense of wholeness or connectedness to the universe, and a positive sense of meaning and purpose in life” (p. 223). As a staunch devotee of God, I understand the importance of having religiosity and spirituality in one’s life. Therefore my goal as a PMHNP is to analyze the evidence surrounding use of religion and spirituality and incorporate an evidence-based spiritual aspect of healing along with psychotherapy and psychopharmacology to improve the patients’ health outcome. This will lead to the compassionate quality care that patients deserve and decrease in rates of depression.
Literature Review
Methods
The objective of this review of the literature was to examine if religiosity and spirituality had an impact on adults with depression. The literature review was conducted using three electronic databases Cumulative Index to Nursing and Allied Health Literature (CINAHL), PubMed, and Medline. Within these databases, keywords depression AND religion AND spirituality AND treatment OR intervention OR therapy were searched. The search was limited to English-language, adults, published from 2006-2016 that emphasized the effects of religiosity and spirituality on depressed adults. A total of 53 articles were initially found but the number reduced to 47 once the duplicates were removed. The abstracts from the 47 articles were reviewed. Thirty-two articles were eliminated upon further review as they did not meet the inclusion criteria. The exclusion criteria were: age below 18 years, any foreign language articles, and any articles that were not relevant to the research topic (e.g. cancer, HIV). Fifteen full-text articles remained. Data was analyzed from the 15 articles and pertinent findings were summarized and included in the results section. The results included associations found between religion and spirituality with depressed adults.
Analysis of the Literature Review
Effects of religiosity and spirituality on depression
The key concept that was reviewed in all of the studies was the effect of religiosity and spirituality on depression. The term religiosity encompassed religious behaviors whereas spirituality discussed spiritual well-being. To determine the role of religiosity and spirituality, various activities and mechanisms were discussed. These included religious activities, praying, reading, and daily spiritual experiences. Thirteen out of fifteen studies revealed that the greater the religiosity and spirituality, the lower depressive symptomology (Caplan et al., 2011; Galek & Porter, 2010; Greeson et al., 2015; Hsu, 2014; Keating, 2013; Koenig, Pearce, Nelson, & Erkanli, 2016; Krumrei, Pirutinsky, & Rosmarin, 2013; Murphy & Fitchett, 2009; Peselow, Pi, Lopez, Besada, & Ishak, 2014; Phillips, Paukert, Stanley, & Kunik, 2009; Schettino et al., 2011; Stanley et al., 2011; Wittink, Joo, Lewis, & Barg, 2009). The studies suggested that the subjects were using these religious techniques on daily basis and it helped them gain strength, improve problem solving styles, and increase their faith which helped them cope with adversities.
Positive religiosity and spirituality led to forgiveness, hopefulness, purposefulness, and a deeper inner peace (Greeson et al., 2015; Krumrei et al., 2013; Murphy & Fitchett, 2009; Phillips et al., 2009; Roh, Lee, Lee, & Martin, 2014). Baetz & Bowen (2011) suggested that religiosity and spirituality improve depressive thoughts and in turn decreased suicidal ideations. On the other hand, negative religiosity and spirituality led to increase in depressive symptoms, and poorer health outcomes (Keating, 2013; Krumrei et al., 2013; Murphy & Fitchett, 2009; Peselow et al., 2014; Phillips et al., 2009; Stanley et al., 2011). There was a greater decrease in mental well-being, life satisfaction and coping. Severe negative religiosity and spirituality can even increase suicidal ideation (Baetz & Bowen, 2011).
Rating scales for depression
Within the literature review, a number of rating scales were used to identify the outcomes of incorporating interventions on depression. A common form of reporting that was observed in all of the reviews was self-reporting surveys. These included face to face semi-structure interviews, phone interviews, and internet surveys. The findings for the surveys were strictly subjective and the various types of surveys ranged from Causal Belief Scale, Beck’s Inventory Scale, Religious Well-being Scale, Montgomery Asberg Depression Rating Scale, Hamilton Rating Scale, and Dysfunctional Attitude Scale (Sadock, Sadock, & Ruiz, 2015). Even though diverse rating scales were applied in different research settings, all aimed to identify the outcome of incorporating religiosity and spirituality with their standard treatment plan for depressed individuals. Interestingly, the research did not suggest that any particular scale worked better than the other.
Depression among believers and non-believers in God
There was a common trend noted amongst eight of the fifteen studies when it came to believing in God (Baetz & Bowen, 2011; Caplan et al., 2011; Keating, 2013; Koenig et al., 2016; Krumrei et al., 2013; Murphy & Fitchett, 2009; Peselow et al., 2014; Schettino et al., 2011). These authors noted in their studies that those who believed in God had better outcomes for depression than the non-believers. The severity of depressive symptoms decreased along with the overall outcome. As Peslow et al. (2014) records, hopelessness, dysfunctional attitudes, and depression were less at baseline and improved at a faster rate for the believers than those who did not believe in God. Trust and mistrust in God, abandonment, anger, questioning and resentment towards God were shared topics in four (Baetz & Bowen, 2011; Keating, 2013; Krumrei et al., 2013; Schettino et al., 2011) of the eight studies that discussed belief in God. In these studies, it was noted that those who did not believe in God had a poorer prognosis for depression at baseline and a slower reduction of symptoms of depression at the end of the study compared to the believers. However, Caplan et al., (2011), Koenig et al., (2016), Murphy & Fitchett (2009) suggested that there was no difference in prognosis at baseline. The subjects who had faith in God had a quicker reduction of symptoms and a greater improvement in depression.
Social support and depression
Hsu (2014), Keating (2013), Koenig et al., (2016), Murphy & Fitchett (2009), Roh et al., (2014), and Schettino et al., (2011) suggest that along with religiosity, spirituality, and coping mechanisms, social support was given great importance. Support from family, friends, workmates, and religious groups led to a decrease in depressive symptomology. Furthermore if support groups were combined with daily spiritual experiences and increased religiosity and spirituality, then the combined effect yielded most favorable results and a substantial improvement in depression (Hsu, 2014; Keating, 2013; Murphy & Fitchett, 2009; Roh et al., 2014).
Conclusion
Although it is not mandated to explore religious and spiritual background in depressed patients, the above evidence suggests that it is an important part of holistic care. What we know is that religiosity and spirituality plays a significant role in mental health especially depression. It is used as a tool to cope and heal. Aten & Leach (2013) note, upon utilization of religiosity and spirituality, a stronger therapeutic bond between the patient and the clinician is created. The research reviewed here also suggests that a believer in God who is religious and spiritual may have an edge in the healing process compared to the nonbelievers.
What we do not know is that why religiosity and spirituality are not being used. Is it the “fear of imposing personal values, bias or negative attitudes toward religion, viewing spirituality as outside of scope of practice, or lack of training?” (Aten & Leach, 2013, p. 17). These are just some of the documented reasons for opposition but are there more.
What we need to know is how to bridge this gap and find a way to incorporate the evidence surrounding religiosity and spirituality into practice. According to the above literature, it is clear that religiosity and spirituality have a significant effect on depression and suicide. With more than 16 million adults suffering from a specific form of depression, it is critical that this intervention needs to be promoted. As the review of the literature results suggests, a combined effort of incorporating religiosity and spirituality, paired with individualized treatment plan, coping techniques, and support systems should lead to positive outcomes amongst depressed adults (Hsu, 2014; Keating, 2013; Koenig et al., 2016; Murphy & Fitchett, 2009).
Related Issue
Financial Implications and the Reimbursement for Time
According to the Centers for Medicare and Medicaid Services (CMS, 2015), the reimbursement rates for psychotherapy session have been on a decline. In 2001, the medicare reimbursement rate for a 45-minute psychotherapy session was $102, whereas today, it is just $84.74 (CMS, 2015). That is more than 30 percent reduction. It is for this particular reason that psychiatrists or nurse practitioners are now resorting to prescribing psychotropic medications rather than providing evidence-based psychotherapy. Although Kartsson (2011) suggests that psychotropic medications are not as equally effective as psychotherapy at improving depression (Kartsson, 2011), it is however a quicker fix.
Office visit time is conserved by asking direct questions that focus on the improvement or the side effects of the prescribed medications rather than exploring the biopsychosocial stressors. This can have a pronounced effect on the outcome of the depressed client as the combination of psychotropic medications with psychotherapy yields the best result (Sadock, Sadock, & Ruiz, 2015). If only one treatment option is provided then the practitioner is only focusing on making the client functional and not properly managing all aspects of clients’ care. This slows down the recovery process for the family member as well as the community. If the client is not recovered, then they cannot be happy, fulfilled, useful, and an asset to the family and the community. Hence, we can assume that money and time may be the reasons why religiosity and spirituality is not assessed in an outpatient mental health setting; even though it may produce positive outcomes.
Religiosity and Spirituality Assessments
To positively influence depressed individuals, the religiosity and spirituality assessments conducted throughout the above research suggest the utilization of few particular assessment scales. These scales include Religious Involvement Inventory (RII), Functional Assessment of Chronic Illness Therapy- Spiritual Well-Being (FACIT-Sp-12), and the Spirituality Index of Well-being. The RII discusses the impact of believing in God, while FACIT-Sp 12 focuses on measuring faith, meaning and peace. The Spirituality Index of Well-being measures how one views their spiritual quality of life. Daaleman & Frey (2004) have suggested these scales to be valid and reliable tools to be used in practice. This is supported by the studies of Hsu (2014), Keating (2013), Koenig et al., (2016), Murphy & Fitchett (2009), Roh et al., (2014), and Schettino et al., (2011).
Conflicting Religious and Spiritual Views
As proposed by the above evidence, religious and spiritual beliefs are associated with wellbeing and mental health. Koenig (2004) suggests that religious beliefs and practices are linked with multiple positive outcomes. These include a decrease in suicide rates, substance abuse, depression, and anxiety. In addition, these religious beliefs also instill hope, optimism, stability, marital satisfaction, purpose and meaning in life, and a faster recovery process.
Since the benefits are great, it is also important to essentially incorporate this into practice. There is a push to include religiosity and spirituality into psychiatric care; however threats to the therapeutic boundaries make it controversial (Poole & Higgo, 2010).
To assess religiosity and spirituality with someone, one does not have to be religious or spiritual. They need to be able to respect the person and the person’s beliefs seated across from them. The problem arises when the religious and spiritual views of the practitioner become conflicting with their clients (Poole & Higgo, 2010). In this instance, the overall care is compromised.
Koenig (2004) suggested reasons why practitioners do not address spiritual issues. The reasons compromised of the uncertainty of time and energy needed to address spiritual issues. The practitioners felt that there was not enough time to discuss these matters. In addition, the practitioners did not want to create an environment where they felt they were overstepping boundaries. A therapeutic rapport has been established and they did not want to create an uncomfortable atmosphere (Koenig, 2004). Not addressing the spiritual issues can impact treatment outcome and more importantly, it is unethical. Moreover, the therapeutic alliance between the practitioner and the client is not solidified.
Humanistic Nursing Theory, Depression, and Religiosity and Spirituality
One of the most widely used nursing models is Zderad and Paterson’s humanistic nursing model. It is based on two ideas of existentialism and phenomenology. Oxford University Press (2014) defined existentialism as “the existence of the individual person as free and responsible agent determining their own development through act of the will” (“Existentialism,” n.d., para. 1), while phenomenology is defined as “an approach that concentrates on the study of consciousness and the object of direct experiences” (“Phenomenology,” n.d., para. 1). Through these two ideas, the most important concept of this model is revealed which is the nurse-patient relationship.
In this nurse-patient relationship, both individuals affect the outcome of the interventions. It is not just the medical interventions that affect the healing process, but it is also the relationship itself. The goal of the nurse should be to respect, value, and understand the patient. If these aspects are taken into consideration, then the patient is viewed as a whole (Patterson & Zderad, 1988). This element of viewing client as a whole can be incorporated into an outpatient behavioral health setting where depressed adults need more help than their psychotherapy and psychotropic medications. A holistic approach is needed which focuses on not just the mind and the body, but also the soul. A religious and spiritual assessment needs to be integrated into outpatient mental health setting where it will not only improve quality outcomes in depressed adults, but it will bring forth a faster improvement (Caplan et al., 2011; Koenig et al., 2016; Murphy & Fitchett, 2009).
Bringing religiosity and spirituality in this particular setting could possibly trigger a chain of events that may be beneficial to all of the mental health disorders. This religious and spiritual assessment will help build a therapeutic relationship between the practitioner and the patient, and it will aid in decreasing depressive symptomology. In order for this to occur, the four metaparadigms of Paterson’s and Zderad’s humanistic nursing theory needs to be met. The four metaparadigms are person, health, environment, and nursing (Paterson & Zderad, 1988).
Person in the humanistic theory refers to viewing person as a whole with special life experiences. Here, the life experiences of the patient are more important and a thorough assessment of social, spiritual, emotional and educational is essential. Within the second metaparadigm, health is viewed as more than just an illness (Paterson & Zderad, 1988). It is seen as being fulfilled and as a resource for maximizing ones potential. Thirdly, the environment is where the interaction occurs. It is the place and time where comfort is built and situations are understood. Lastly, the nursing in the humanistic theory refers to “a purposeful call and response in which the nurse responds to the call by caring for the person who has health-related unmet needs” (p. 53). As mentioned above, care is based on person-focused and it entails professionalism, expertise, holism, and life experiences from both the nurse as well as the patient. This is where the genuine presence of the nurse leads to improvement in wellbeing.
The humanistic model of nursing aligns with the proposed idea of incorporating a religiosity and spirituality assessment in outpatient mental health clinic for depressed adults. This intervention will follow the same four metaparadigms. The person metaparadigm will include a thorough investigation of client’s vast experiences, creativity, awareness, and the ability to be responsible. The health paradigm will include assessment of depression, spirituality, religiosity and social support. Environment will be the practitioner’s office where the visit will take place and it will depend on the availability of the practitioner. Lastly nursing will include the interaction, openness, education, presence, and support from the practitioner. This intervention is based on the humanistic model of nursing. The aim of this intervention is to improve outcomes for the depressed adults. This is supported by Glanz & Bishop (2010) work that demonstrates that interventions based on theories are more effective than interventions without theories. Moreover, research by Castro, Freitag, & Teixeira (2011), Pereira & Carvalho (2012), and Wu & Volker (2012), suggest that incorporating humanistic theory already leads to benefits on the burn unit, obstetric unit, and palliative care.
Advanced Practice Nurse Role
As mentioned above, there are more than sixteen million depressed adults in the United States. This is a distressing situation calling for alternative solutions apart from psychotherapy and psychopharmacology. To improve the identified health issue, a link is needed that can translate evidence into practice. This link is the PMHNP.
PMHNP’s are advanced practice nurses (APN) who have completed graduate-level education from accredited schools (Rounds, Zych, & Mallary, 2013). The APN program prepares students to see patients across the health wellness-illness continuum. PMHNPs are specifically trained to work with the mental health population (Rounds, Zych, & Mallary, 2013). In addition, PMHNP’s role is to lead collaborative inter-professional care teams in their work setting and bring forth innovative nursing practices that focus on individualized care. This client-centered care includes being able to see the person as a whole and to promote health education which the client can use away from the clinical setting.
PMHNP’s have additional preparation and skills to use the scientific process and national Nursing Standards of Care (Bryant-Lukosius et al., 2004; Mariano, 2016). The Nursing Standards of Care include assessing and making a diagnosis, proposing an evidence-based intervention, implementing that intervention, and evaluating the effectiveness of that particular intervention. While nursing remains the foundation, it is the privilege of diagnosing disorders, proposing interventions, and prescribing medications that sets apart APN from nurses.
The formulation of the Religiosity and Spirituality Assessment
Upon gathering the three religious and spiritual instruments that were linked to depression, the PMHNP will assimilate these assessments and formulate a 10-question religious and spirituality scale (Appendix A). This will be a specialized collection of evidence-based questions that are aimed at inquiring about a person’s religion and spiritual characteristics and preferences (Daaleman & Frey, 2004). Administration and discussion of these questions has been linked to decrease in the depression symptomology (Caplan et al., 2011; Galek & Porter, 2010; Greeson et al., 2015; Hsu, 2014; Keating, 2013; Koenig et al., 2016; Krumrei et al., 2013; Murphy & Fitchett, 2009; Peselow et al., 2014). Additionally, the evidence surrounding the scale is also associated with increased speed of symptom reduction and stronger therapeutic alliance between the prescriber and the client (Koenig et al., 2016). From business point of view, this scale also serves its purpose. If the clients become stable sooner, then they will be seen less often. This ultimately may lead to more availability of prescribers for newer clients. Since this scale serves multiple purposes, it is appropriate to propose it as an intervention to decrease depression in the mental health setting.
Proposed Intervention
Since the role of PMHNP is to integrate evidence-based practice in their work setting, a thorough researched intervention is developed and integrated into practice at Pacific Clinics in Monrovia. Pacific Clinics in Monrovia will be the starting point, and if successful, the goal is to incorporate this scale in all 90 Pacific Clinics locations. Humanistic Model of Nursing Theory will be used to formulate this intervention and it is important to consider the four domains of this theory: person, health, environment, and nursing (Paterson & Zderad, 1988).
Person
Since the focus of the Humanistic Nursing Theory revolves around the person, in this particular situation, the focus will revolve around the religiosity and spirituality assessment scale. The PMHNP’s goal is to bring forth a 10-question religiosity and spirituality scale that is an amalgamation of RII, FACIT-Sp 12 and the Spirituality Index of Well-being scales (Daaleman & Frey, 2004). While each of these scales has been proven to create positive effects for people, it is presumed that an accumulation of these scales will yield similar results. The content in this 10-question assessment scale is supported by multiple researches in mental health (Caplan et al., 2011; Galek & Porter, 2010; Greeson et al., 2015; Hsu, 2014; Keating, 2013; Koenig et al., 2016; Krumrei et al., 2013; Murphy & Fitchett, 2009; Peselow et al., 2014).
This 10-question scale includes an assessment of several spiritual themes. The themes include faith, blessings, peace, God, problems, priorities, strength, satisfaction, illness, and openness. Each question discussion a particular theme. The first question discusses the importance of faith in one’s life. The second question inquired about gratification of one’s blessings. Third discussed feelings of inner peace, while fourth focused on being one with God. Fifth and sixth question examines the role faith has played throughout life and inquires about the places where one finds courage to deal with problems. Seventh question discusses the comfort associated with religion and spirituality, while question eight discusses life’s satisfaction. The last two questions discuss the insight into illness and the willingness to discuss religious and spiritual matters (See Appendix A for more information on the scale).
Even though this scale remains the focal point of the intervention, it is also important to consider an additional scale that helps measure the effectiveness of the religiosity and spirituality scale. This additional scale is the Patient Health Questionnaire (PHQ-9). The PHQ-9 is specifically designed to assess depression. The criteria for Major Depressive Disorder require the presence of 5 or more of the following symptoms to be present for the 2 week period. The symptoms include depressed mood, sleep problem, lack of interest, hopelessness, decreased energy, decreased concentration, loss or increase in appetite, psychomotor agitation or retardation, and suicidal ideations (DSM-5, 2013). Accordingly, PHQ-9 is an investigation of these symptomology.
Health
According to Paterson & Zderad (1988), health is more than just illness. It is for this reason, the PMHNP is bringing forth a holistic approach to mental health, more specifically, in depressed adults. Through the discussion of this religiosity and spirituality assessment scale, the goal is to reduce depressive symptomology in the adult population. The effectiveness of the religiosity and spirituality scale will be measured by the changes in the PHQ-9 scores and the clients overall satisfaction. Furthermore, the plan is to maximize potential for each individual and help nurture their emotional and mental health (Paterson & Zderad, 1988). If this religiosity and spirituality assessment scale is successful, it can help patients grow in a hale and hearty way. It will bring out the clients creativeness to cope with all life situations and not just depression. The focus ultimately lies in restoring, sustaining, and promoting health (Paterson & Zderad, 1988), which is the important objective of this scale.
Environment
According to Paterson & Zderad (1988), environment is the place where the intervention takes place. For this particular scenario, it would be the Pacific Clinics Behavioral Healthcare Services in Monrovia, California. More specifically, it will be the psychiatrist or the PMHNP’s office. In order to get this scale in place, the first step requires the PMHNP to set up a meeting with the prescribers, therapists, case managers, informational technologist, and the director himself. The prescribers are the psychiatrists and the PMHNPs. In order for any intervention to pass and be effective in this clinical setting, the program directors approval is necessary (A. Sanchez, personal communication, March 3, 2017). PMHNP needs to educate the interdisciplinary team on the overwhelming statistics of depression and the importance of including religiosity and spirituality in depression management. Even though the team might see depressed individuals daily, statistics speaks volumes.
The current treatment plan for depression at Pacific Clinics needs to be addressed. This plan consists of limited psychotherapy by the therapists and an overreliance on medication services provided by the prescribers. For the depressed individuals, insurance reimbursement determines the number of therapy sessions. The medication management visits are based on the availability of the prescribers. This is not an ideal situation for the patients as they are left with limited options and limited coping mechanisms in their everyday lives.
This gives the PMHNP the opportunity to present the 10-question religiosity and spirituality assessment scale, which is a feasible solution that is reasonable, sustainable, and financially accommodating. This intervention is evidence based, requires less than 10 minutes to administer, and is cost effective. The goal of this intervention serves the core values of Pacific Clinics, which are to make the client as first priority, and to have the client reach their highest level of functioning (“Pacific clinics,” 2017). In addition, it also respects cultural differences which eliminate any biased beliefs.
To roll out this scale effectively, interdisciplinary collaboration is mandatory. Everyone in the meeting plays a key role in enhancement of the client’s wellbeing and therefore they need to be aware of the new intervention and their role within it. During this meeting, the PMHNP will present the data, the evidence, and the positive outcome that has been associated with the evidence based scale (Hsu, 2014; Keating, 2013; Murphy & Fitchett, 2009; Roh et al., 2014). The PMHNP will then verbalize the expected roles of each team member.
The prescriber’s role would be introduced as crucial as they will be the one executing the scale. Based on their clinical judgment and the PHQ-9 scores, the prescriber will appropriately diagnose the client as depressed and then carry out the religiosity and spirituality assessment scale for the next three months. This time frame allows for maximized results from a collaborative effort of the scale, therapy, and the medications. According to the Humanistic Model, there will be a stronger alliance between the prescriber and the client, and expectantly, a discussion of religiosity and spirituality should lead to an improvement in client’s depression. As D’Souza & George (2006) state, “Our calling as physicians and clinicians is to cure sometimes, relieve often, and comfort always” (p. 411). When the prescriber respects and addresses the core that gives clients hope and meaning in life, the treatment is considered holistic (D’Souza & George, 2006).
The role of the informational technologist would be to insert the scale into the electronic medical record system. The scale should appear as a drop down menu after the selection of appropriate depressive symptomology by the prescribers. The therapists will be asked to follow up with the client regularly regarding their progress in spirituality. The case managers will be responsible for finding any resources which may be beneficial to the client. This will make it easier for the client to find support outside of the clinic.
Lastly, The PMHNP will then verbalize the religiosity and spirituality assessment scale and its criteria. This scale is to be performed on clients aged 18 and above who are currently depressed and meet the criteria for major depressive disorder. Since every prescriber has a unique style of assessing clients, it is crucial that they follow the scale as indicated. This is a multi-evidence based scale and each question is supported by research, and therefore the scale must be applied thoroughly.
Any questions or concerns about the intervention and the individual role will be thoroughly discussed and cleared up in this meeting. In order for this intervention to be successful, it is important for everyone to be working together. Personal spiritual views cannot be conflicting with the client’s spiritual views. The imposing of a particular belief is not ethical. One must not initiate a prayer without having a background on the client’s beliefs, religion, and spirituality. The goal is to make the client fully functional through a holistic collaborative approach. Once the director and the team approve and understand their role, the intervention can be carried out immediately.
Nursing
The last domain in the Humanistic theory is nursing. Here is where the nurse cares for the client whose needs are not met (Paterson & Zderad, 1988). The essential feature of the religiosity and spirituality scale is that it strives to meet all the needs of the client. There is a gap in mental health and it is trying to fill that void. By utilizing all the current research on religiosity and spirituality and the impact it has on depression, the PMHNP can bring forth change that is in forefront of peoples mind (Hsu, 2014; Keating, 2013; Murphy & Fitchett, 2009; Roh et al., 2014). The medications and the therapy are crucial for depressed adults, but religiosity and spirituality is equally as important (Koenig, 2013).
Through this intervention, the PMHNP is able to carry out their role within the standards of practice. By executing this designed plan, they are able to successfully implement and evaluate this intervention at an advanced practice level. While they are translating the evidence into practice, they are teaching and promoting health. In addition, they are able to build and lead collaborative inter-professional care teams to improve client outcomes.
Conclusion
Depression in adults is a prevalent issue across United States. It not only affects one’s ability to think and feel, but it also affects their appetite, sleep, relationships, and even work (Sadock, Sadock, & Ruiz, 2015). In order for one to be diagnosed as depressed, there needs to be significant distress or impairment in functioning. This must last for 2 weeks with at least five or more of the following symptoms: depressed mood, sleep problems, lack of interest, hopelessness, decreased energy, decreased concentration, loss or increase in appetite, psychomotor agitation or retardation, and suicidal ideations (DSM-5, 2013). While the standard of treatment for depression includes therapy and medications, sometimes it is not enough. The high relapse rate, along with slower response to treatment, and the increased probability of suicide rate justifies a need for an increase in treatment options.
In addition to the current treatment practice, augmenting an evidence-based religiosity and spirituality scale has the potential to help decrease the depression symptomology as evidence suggested in the literature review. This review of the literature explored the effects of religiosity and spirituality on depressed individuals. The evidence in the review of the literature suggested that lower depressive symptomology was associated with greater religiosity and spirituality. The evidence also indicated that a depressed adult with a strong spiritual background will have a rapid improvement in their health outcome compared to someone who is not spiritual. Mutually, all articles including Peslow et al. (2014) suggest that assessing spirituality and encouraging spiritual discussion may improve depression.
By reviewing these findings, implementing a plan, and evaluating the outcome, the PMHNP has fulfilled their role and followed their standard of practice. Remarkably, the second objective of this paper was to propose a spiritual assessment which can be utilized in a mental health setting to improve depressive outcomes. After taking into account the daily spiritual experiences, Religious Involvement Inventory, FACIT-Sp 12 and the Spirituality Index of Well-being, this intervention was innovatively created. This 10-question religiosity and spirituality scale incorporates key themes and discussion points which has the potential to send positivity in the clients lives. It gives client’s reason to introspect and it avenues to support system. Through spirituality, the healthcare team can emphasize hope, insight, beliefs, and a sense of purpose (Peslow et al., 2014).
Future research recommendations consist of evaluating the usefulness of this particular intervention at Pacific Clinics. The overall effectiveness would be measured by collecting the PHQ-9 forms and gathering a report from the prescribers as well as the clients. If there was a remarkable difference in the depressive symptoms within these clients, then it is recommended that this intervention be applied into all 90 Pacific Clinic locations.
There could be potential barriers nonetheless that may hinder this intervention from reaching its full effectiveness. Future research should also focus on discovering these barriers which may include but not limited to lack of time, conflicting spiritual views, difficulty adapting, enthusiastic spirit, crisis situation, and an atheist mindset. While these factors could emerge from the client’s side, it may very well be visible in the prescriber. In addition, the healthcare team’s involvement must also be assessed. Each team member was given a particular task and if they abide by their responsibilities, then the client would have received the compassionate quality care which they deserve.
Future research may also focus on the relationship between the client and the prescriber. There has to be some change that was observed once this intervention was administered. The change may have strengthened the prescriber-client bond or it may have done the opposite. It is imperative for future research to avoid limitations of previous research and move forward with careful evaluation (James & Wells, 2003). Hitherto, religion and spirituality is ignored in the clinical realm, it may be time to incorporate this in the clinical ground.
References
American Association of Suicidology. (2014). Depression and suicide risk factsheet. Retrieved March 24, 2017, from https://www.suicidology.org/portals/14/docs/resources/factsheets/2011/depressionsuicide2014.pdf
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association.
Ana Kelve de Castro, D., Lorita Marlena Freitag, P., & Maria Grasiela Teixeira, B. (2011). Application of humanistic theory concepts at a burn unit. Revista Da Rede De Enfermagem Do Nordeste, Vol 10, Iss 2 (2011), (2)
Aten, J. D., & Leach, M. M. (2009). Spirituality and the therapeutic process: A comprehensive resource from intake to termination. Washington, DC: American Psychological Association.
Baetz, M., & Bowen, R. (2011). Suicidal ideation, affective lability, and religion in depressed adults. Mental Health, Religion & Culture, 14(7), 633-641. doi:10.1080/13674676.2010.504202
Bryant-Lukosius, D., DiCenso, A., Browne, G., & Pinelli, J. (2004). Advanced practice nursing roles: development, implementation and evaluation. Journal Of Advanced Nursing, 48(5), 519-529. doi:j.1365-2648.2004.03235.x10.1111/j.1365-2648.2004.03234.x
Burcusa, S. L., & Iacono, W. G. (2007). Risk for Recurrence in Depression. Clin Psychol Rev. 2007 December ; 27(8), 959–985.
Caplan, S., Paris, M., Whittemore, R., Desai, M., Dixon, J., Alvidrez, J., . . . Scahill, L. (2011). Correlates of religious, supernatural and psychosocial causal beliefs about depression among Latino immigrants in primary care. Mental Health, Religion & Culture, 14(6), 589-611. doi:10.1080/13674676.2010.497810
Centers for Medicare and Medicaid Services. (2015). Physician fee schedule. Retrieved March, 24, 2017, from https://www.cms.gov/medicare/medicare-fee-for-service-payment/physicianfeesched/
Daaleman, T. P., & Frey, B. B. (2004). The Spirituality Index of Well-Being: a new instrument for health-related quality-of-life research. Annals Of Family Medicine, 2(5), 499-503.
D’Souza, R., George, K. (2006). Spirituality, religion and psychiatry: its application to clinical practice. Australasian Psychiatry, 14(4), 408-412.
Existentialism. (n.d.). In Oxford’s online dictionary. Retrieved March 24, 2017 from https://en.oxforddictionaries.com/definition/existentialism
Galek, K., & Porter, M. (2010). A brief review of religious beliefs in research on mental health and ETAS theory. Journal of Health Care Chaplaincy, 16(1/2), 58-64. doi:10.1080/08854720903489246
Glanz, K., & Bishop, D. (2010). The role of behavioral science theory in development and implementation of public health interventions. Annual Review Of Public Health, 313, 99-418. doi:10.1146/annurev.publhealth.012809.103604
Greeson, J. M., Smoski, M. J., Suarez, E. C., Brantley, J. G., Ekblad, A. G., Lynch, T. R., & Wolever, R. Q. (2015). Decreased symptoms of depression after mindfulness-based stress reduction: potential moderating effects of religiosity, spirituality, trait mindfulness, sex, and age. Journal Of Alternative And Complementary Medicine (New York, N.Y.), 21(3), 166-174. doi:10.1089/acm.2014.0285
Haugan, G. (2015). The FACIT-Sp spiritual well-being scale: an investigation of the dimensionality, reliability and construct validity in a cognitively intact nursing home population. Scandinavian Journal Of Caring Sciences, 29(1), 152-164. doi:10.1111/scs.12123
Hsu, H.-C. (2014). Effects of Religiousness on Depressive Symptoms Among Elderly Persons in Taiwan. Clinical Gerontologist, 37(5), 446-457. doi:10.1080/07317115.2014.937549
Isolda Pereira da, S., & Ana Fátima Carvalho, F. (2012). Concepts of humanistic theory in obstetric care. Revista Da Rede De Enfermagem Do Nordeste, Vol 8, Iss 1 (2012), (1)
James, A., & Wells, A. (2003). Religion and mental health: towards a cognitive-behavioral framework. British Journal Of Health Psychology, 8(3), 359-376. doi:10.1348/135910703322370905
Kartsson, H. (2011). How Psychotherapy Changes the Brain: Understanding the Mechanisms. Psychiatric Times, 28(8), 21-23.
Koenig, H. G. (2004). Religion, spirituality, and medicine: research findings and implications for clinical practice. Southern Medical Journal. 97(12),1194-200.
Keating, D. M. (2013). Spirituality and support: a descriptive analysis of online social support for depression. Journal Of Religion And Health, 52(3), 1014-1028. doi:10.1007/s10943-012-9577-x
Koenig, H., Pearce, M., Nelson, B., & Erkanli, A. (2016). Effects on Daily Spiritual Experiences of Religious Versus Conventional Cognitive Behavioral Therapy for Depression. Journal of Religion & Health, 55(5), 1763-1777. doi:10.1007/s10943-016-0270-3
Kroenke, K., Spitzer, R. L., Williams, J. W., Ashrafioun, L., Bonar, E., & Conner, K. R. (2016). Patient Health Questionnaire–9. Journal Of American College Health, 64(3), 257-261.
Krumrei, E., Pirutinsky, S., & Rosmarin, D. (2013). Jewish Spirituality, Depression, and Health: an Empirical Test of a Conceptual Framework. International Journal of Behavioral Medicine, 20(3), 327-336. doi:10.1007/s12529-012-9248-z
Mariano, C. (2016). NURSING EMERGING. ANA Nursing: Scope and Standards of Practice, (2015) 3rd Edition. Beginnings (American Holistic Nurses’ Association), 36(2), 5.
Medscape. (2011). America’s Use of Psychotropic Medications on the Rise. Retrieved March 24, 2017, from http://www.medscape.com/viewarticle/753789
Munoz, A. R., Salsman, J. M., Stein, K. D., & Cella, D. (2015). Reference values of the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being: a report from the American Cancer Society’s studies of cancer survivors. Cancer (0008543X), 121(11), 1838-1844. doi:10.1002/cncr.29286
Murphy, P. E., & Fitchett, G. (2009). Belief in a concerned god predicts response to treatment for adults with clinical depression. Journal Of Clinical Psychology, 65(9), 1000-1008. doi:10.1002/jclp.20598
National Alliance on Mental Illness. (n.d.). Mental health by the numbers factsheet. Retrieved March 24, 2017, from http://www.nami.org/Learn-More/Mental-Health-By-the-Numbers
Pacific Clinics. (n.d.). About us. Retrieved March 24, 2017 from http://www.pacificclinics.org/about_us
Paterson, J., Zderad, L. (1988). Humanistic Nursing.
Patten, S. (2013). Recurrence risk in major depression. Depression & Anxiety (1091-4269), 30(1), 1-4. doi:10.1002/da.22030
Peselow, E., Pi, S., Lopez, E., Besada, A., & Ishak, W. W. (2014). The Impact of Spirituality Before and After Treatment of Major Depressive Disorder. Innovations in Clinical Neuroscience, 11(3/4), 17-23.
Phenomenology. (n.d.). In Oxford’s online dictionary. Retrieved March 24, 2017 from https://en.oxforddictionaries.com/definition/existentialism
Phillips, L. L., Paukert, A. L., Stanley, M. A., & Kunik, M. E. (2009). Incorporating religion and spirituality to improve care for anxiety and depression in older adults. Geriatrics, 64(8), 15-18.
Poole, R., & Higgo, R. (2011). Spirituality and the threat to therapeutic boundaries in psychiatric practice. Mental Health, Religion & Culture, 14(1), 19-29. doi:10.1080/13674671003746845
Roh, S., Lee, Y.-S., Lee, J. H., & Martin, J. I. (2014). Typology of religiosity/spirituality in relation to perceived health, depression, and life satisfaction among older Korean immigrants. Aging & Mental Health, 18(4), 444-453. doi:10.1080/13607863.2013.848837
Rounds, L. R., Zych, J. J., & Mallary, L. L. (2013). The consensus model for regulation of APRNs: Implications for nurse practitioners. Journal Of The American Association Of Nurse Practitioners, 25(4), 180-185. doi:10.1111/j.1745-7599.2012.00812.x
Sadock, B. J., Sadock, V. A., & Ruiz, P. (2015). Kaplan & Sadock’s synopsis of psychiatry: Behavioral sciences/clinical psychiatry (Eleventh edition.). Philadelphia: Wolters Kluwer.
Schettino, J. R., Olmos, N. T., Myers, H. F., Joseph, N. T., Poland, R. E., & Lesser, I. M. (2011). Religiosity and treatment response to antidepressant medication: a prospective multi-site clinical trial. Mental Health, Religion & Culture, 14(8), 805-818. doi:10.1080/13674676.2010.527931
Spurr, S., Berry, L., & Walker, K. (2013). The meanings older adolescents attach to spirituality. Journal For Specialists In Pediatric Nursing, 18(3), 221-232. doi:10.1111/jspn.12028
Stanley, M. A., Bush, A. L., Camp, M. E., Jameson, J. P., Phillips, L. L., Barber, C. R., . . . Cully, J. A. (2011). Older adults’ preferences for religion/spirituality in treatment for anxiety and depression. Aging & Mental Health, 15(3), 334-343. doi:10.1080/13607863.2010.519326
Swenson, D. (2006). Advanced registered nurse practitioners: standards of care and the law. Journal Of Legal Nurse Consulting, 17(4), 3-6.
Wittink, M. N., Joo, J. H., Lewis, L. M., & Barg, F. K. (2009). Losing faith and using faith: older African Americans discuss spirituality, religious activities, and depression. Journal Of General Internal Medicine, 24(3), 402-407. doi:10.1007/s11606-008-0897-1
World Health Organization. (n.d.). Depression factsheet. Retrieved March 24, 2017, from http://www.who.int/mediacentre/factsheets/fs369/en/
Wu, H., & Volker, D. L. (2012). Humanistic Nursing Theory: Application to hospice and palliative care. Journal Of Advanced Nursing, 68(2), 471-479. doi:10.1111/j.1365-2648.2011.05770.x
Appendices
Appendix A
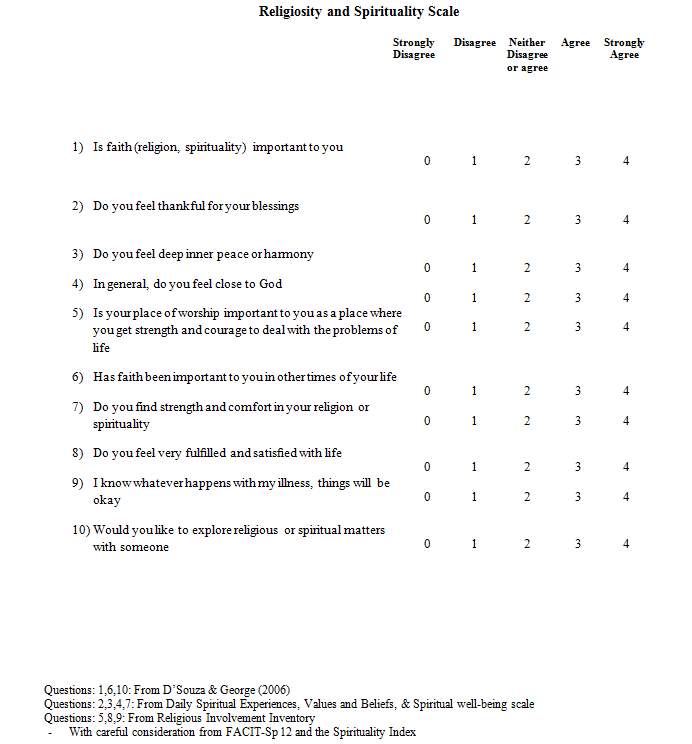
(D’Souza & George, 2006; Haugan, 2015)
Appendix B
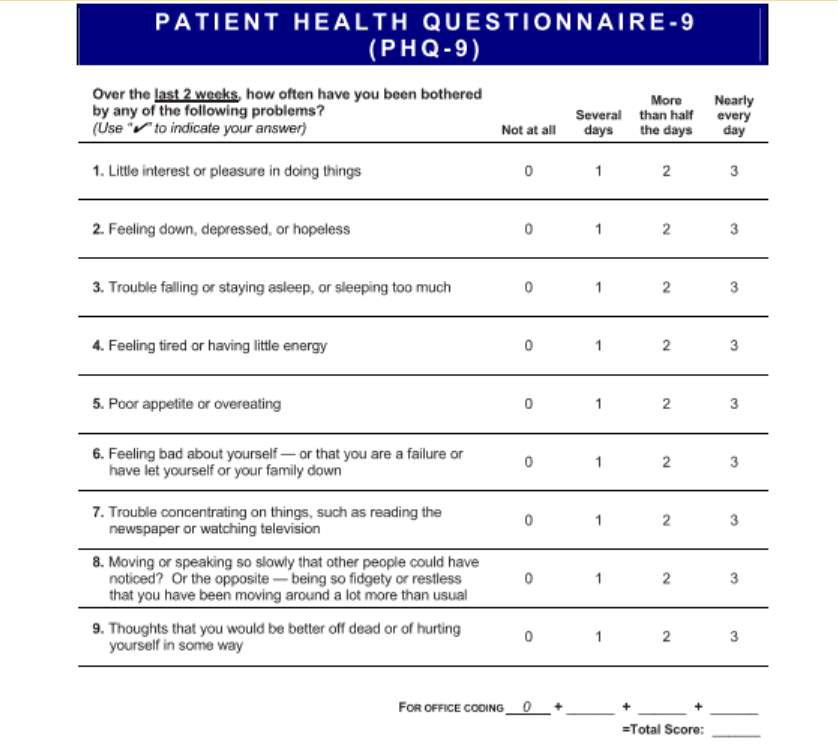
(Kroenke et al., 2016)
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Mental Health"
Mental Health relates to the emotional and psychological state that an individual is in. Mental Health can have a positive or negative impact on our behaviour, decision-making, and actions, as well as our general health and well-being.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




