Caring and Professional Practice in Mental Health Nursing
Info: 7626 words (31 pages) Dissertation
Published: 9th Dec 2019
Tagged: NursingMental Health
Contents
Appendix 2…………………………………………….21
Case Study
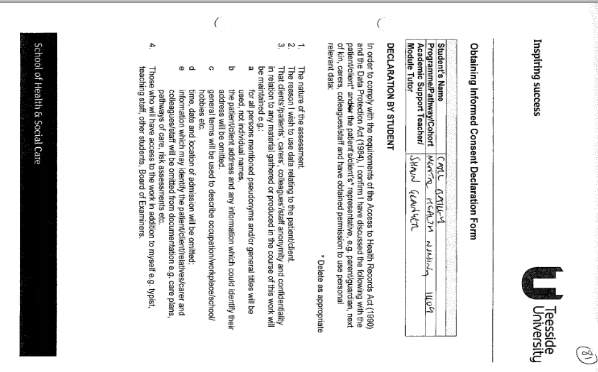
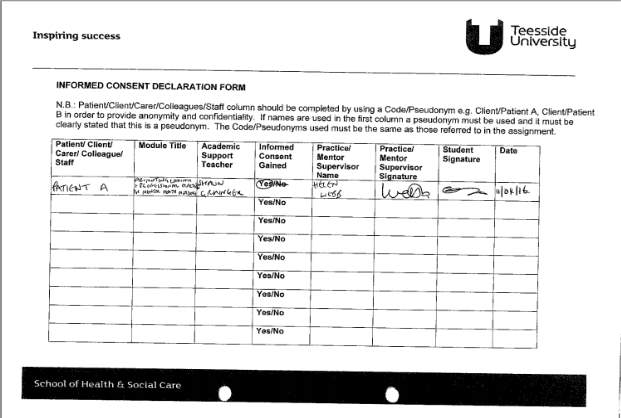
The purpose of this case study is to explore the delivery of care to a patient who was part of the student nurse’s journey throughout placement. The patient was of interest to the student due to being admitted as they begin their time on the ward and having an illness of specific interest. Due to this assignment requiring an in depth discussion of the patient’s background, history and current care, it is required by the School of Health and Social Care and Nursing Midwifery Council (NMC, 2015) to have gained consent from the patient. Although the patient was deemed as competent to give consent it was considered good practice to also include their main carer in the decision following a conversation with the patient. To ensure this was completed in accordance with guidelines the nature of the assignment was explained to the patient and the carer and they were also made aware that confidentiality would be maintained, in agreement with the NMC Code (NMC, 2015); for the patient and all those involved in their care. Confidentiality will be ensured throughout the assignment by referring to the patient as the pseudonym ‘Patient A’ and generalised terms being used to prevent identification. The only information that will be disclosed is the gender of the patient which is female, this is due to symptoms that are only present in females when suffering from the illness discussed. The gaining of consent and explanation that the patient was not under any obligations to agree with reassurance their care would not be effected was witnessed by a qualified nurse and signed for in place of the patient (Appendix 1).
Patient A was initially admitted to a general hospital following a significant reduction in weight over a short period of time. The reduction in weight had meant that Patient A was now at risk of causing herself serious physical harm. Patient A was admitted to an intensive care ward due to the significant physical risk of her low weight. Whilst Patient A was in the general hospital a referral was made to the CAMHS inpatient service, where the student was currently on placement, to be assessed for an eating disorder. During the assessment process Patient A was assessed for Anorexia Nervosa (AN), which is classed as a serious mental health condition in which the person attempts to keep their body weight as low as possible through means of restricting diet, excessive exercising and vomiting (NHS, 2016a). Patient A’s symptoms were measured against the criteria for diagnosing AN highlighted by the ICD-10 (World Health Organisation, 1992). It was here that Patient A was deemed to be at only 64% of her recommended body weight for age and height, this placed her in the red zone of the Junior MARSIPAN Guidelines (Ayton et al., 2015). She had an abnormal ECG with a long QT interval, had bradycardia with a heart rate of 38 beats per minute when resting, her body temperature was 33.5°C on admission to general hospital. Patient A had lost 20KG in the previous 8 weeks, she was also suffering from amenorrhea and had not had a period for a prolonged period of time. Patient A expressed a fear of putting weight on and had a self-belief that she was overweight, despite her current presentation. Patient A had been taking part in compensatory behaviours to manage her weight and aiming for further weight reduction by restricting her diet and excessively exercising. It was from this assessment and the meeting of the criteria highlighted by the ICD-10 that Patient A was diagnosed with AN and would benefit from a hospital admission. The decision was made whilst taking the National Institute for Health and Care Excellence (NICE) guidelines (2004a) into consideration, which state that treatment for those suffering with AN should remain on an outpatient basis. However, it was due to the immediate significant risk (NICE, 2004a) Patient A was posing to her physical health that admission was deemed necessary, once she had physically recovered enough to be admitted to a Mental Health Hospital.
When the decision to admit Patient A to hospital was relayed back to her she stated that she did not need treatment as she felt as though she was not ill; and for this reason would not be willing to go into hospital as an informal patient. Due to the need for Patient A to receive treatment, in accordance to NICE guidelines (2004a), the decision was made to detain her on a Section 2 of the Mental Health Act (Department of Health ,DoH 1983). This meant Patient A would be admitted into hospital for a period of assessment and treatment for up to 28 days; following this period Patient A would be reassessed and either discharged, remain as an informal patient or detained on a Section 3 (DoH, 1983). Following the period it was decided to detain Patient A on a Section 3 due to the need for further treatment and taking into account the lack of insight Patient A had into her illness.
The Nursing Process is a scientific method, consisting of six steps; assessment, diagnosis, outcome identification, planning, implementation and evaluation (Kneisl et al., 2004). It is seen as a problem solving method and is universally seen as the most appropriate method to follow when caring for a patient due to it encompassing all necessary components (Kneisl et al., 2004; Fortinash & Wooret, 2004). The dynamic nature of the model enables the nurse to focus on what is important at the time and offers a flexible approach (Fortinash & Worret, 2004). This is significantly important when caring for those with mental health issues (Ward, 2011; Cleary et al., 2012) due to the complexity and unpredictability of the illnesses that are being treated.
The assessment phase of the nursing process is often referred to as the most critical (Fortinash & Worret, 2004), it is here that the nurse must effectively use their interpersonal skills and utilise as many different forms of collecting information available to them as possible. This will help in making the correct clinical judgements and ensure the appropriate interventions are put in place (Kneisl et al., 2004). The importance of employing a holistic assessment is addressed throughout the healthcare setting (The Sainsbury Centre for Mental Health, 2001; DoH, 2002; Disability Rights Commission, 2006; Brimblecombe, 2007) whilst also being recognised as a way to develop the therapeutic relationship (Shatell et al., 2007). To guarantee a holistic assessment is undertaken the nurse should consider the biopsychosocial model; which focuses on the three domains that can effect a person. The importance of considering this model is recognised through evidence showing that anorexia is more than often a result of the three domains impacting on one another (McCabe et al., 2006; Connan et al., 2003); therefore, by disregarding one this would potentially have a negative impact on recovery. Furthermore, Holt and Convey (2012) provide evidence to support the need for the biopsychosocial model to be paramount in assessment and planning; whilst considering a person-centred approach and individualised care to promote the best chance for health promotion.
Prior to admission to hospital Patient A had already undergone assessments which had resulted in her diagnosis of AN. However, upon admission to the inpatient setting Patient A was assessed using various different methods to ensure a holistic approach was adopted and both subjective and objective data was obtained (Kneisl et al., 2004). This is to help formulate an idea of how best to work with Patient A to aid her recovery. Initial assessment was conducted through discussion with Patient A and her carer; this has been highlighted as one of the most vital forms of collecting information (Fortinash & Worret, 2004). This allowed Patient A to offer her own interpretation of what she believed was happening through discussing her mental, social and physical state which then offered the nurse the opportunity to assess her insight in each aspect and also determine where the issues were more prevalent. Through identifying the biopsychosocial needs then assessment is undertaken in accordance with NICE guidelines (2004a). The nurse should also use their observation skills in this situation to notice any problems that the patient might be unwilling to talk about. It could be through an inability to maintain concentration or eye contact, if the patient was restless, having closed body language or other unusual habits that the nurse could begin to assume further issues. In Patient A’s case it was observed that self-harm marks were present accompanied by teary eyes thus resulting in the assumption of low mood being present.
Patient A underwent numerous physical examinations which consisted of an electrocardiography (ECG) and other physical observations. This was to determine how the AN had affected her hearts functioning. This was vital due to the complications the illness can cause for the heart which can result in mortality (Papadopoulos et al., 2009; Grover et al., 2012; Yahalom et al., 2013). The ECG offered an opportunity to determine if there was an irregular heartbeat which fortunately there was not. However, it was discovered that Patient A was bradycardic and was showing signs of hypotension which suggested that her AN had begun to cause cardiac related problems (NHS, 2016b). Taking NICE recommendations (2004a) into consideration blood tests were also carried out with the results showing no current abnormalities meaning no immediate action was required. However, if abnormal readings in levels of potassium, glucose or bicarbonate were present the necessary action would need to be taken.
As part of the assessment process it was also required that Patient A was to complete the EDI-3 (Garner, 2004). This a 91-item questionnaire which is designed to assess the symptoms and psychological features of an eating disorder. The EDI-3 has received support from research (Clausen et al., 2010) showing it to be a valid tool to measure the presence of an eating disorder. However, with it being a self-report measured style of assessment this means it is open to possible manipulation (Fan et al., 2006; van de Mortel, 2008) and the findings should be acted upon with caution. The findings from Patient A’s completed EDI-3 did show that she was high scoring in; a drive for thinness, perfectionism, interoceptive awareness, asceticism and social insecurity; all of which show signs that an eating disorder is present.
Patient A’s assessment also included the use of a formulation meeting which utilised Weerasekara’s (1995) 5P’s model. Formulation is recognised as a means of ensuring a thorough assessment is accomplished (Dallos & Johnstone, 2014). Also, when completed with the client, whilst actively listening to their wants and needs, it can help foster a therapeutic relationship (Robinson, 2009). Through this it was possible to highlight Patient A’s current problem and discover how the predisposing, precipitating and perpetuating were contributing to the progression of the illness and through exploration of Patient A’s protective factors it was possible to begin to look into how these could be utilised in working towards recovery.
The nursing diagnosis will look at issues that have been highlighted in the assessment. The immediate risk that was identified was Patient A’s weight loss as a result of diet restriction, poor self-image and excessive exercising with secondary issues being low mood and self-harm. It is through the thoughtfulness given to these that the next step of the nursing process is outcome identification. It is this step that the nurse should work with the client to identify specific goals with measurable indicators (Fortinash & Worret, 2004); with the aim of improving their health status (Kneisl et al., 2004). The consideration of risk that could derive from a client reaching outcome goals that are not desired (e.g. an anorexic gaining weight could cause low mood) should also be focused on in this step (Fortinash & Worret, 2003). This is the point at which the nurse will have to utilise their risk management skills.
Due to Patient A going through a period of starvation it was important that the nurse identified goals in regards to weight gain so that they did not cause further complications (NICE, 2006). The aim of this would be to prevent refeeding syndrome from occurring which can be fatal (Crook et al., 2001; Mehanna et al., 2008; Webb et al., 2011). Further outcomes for Patient A would be to reduce her exercise, to help improve her self-image, to normalise food and to aim to towards the reintroduction of her period; which was the point agreed where Patient A would be able to maintain her weight. The nurse also identified Patient A’s low mood and self-harm as areas that required improvement so outcome indicators were identified in the reduction of self-harming behaviours and working towards mood improvement. However, the nurse must consider how AN and low mood are often linked and can foster each other’s development (Sassaroli et al., 2008; Blinder et al., 2006). For this reason when planning the care of the patient thought must be given to how best to treat both effectively so one does not negatively affect the other. It was also deemed important here to consider risk in relation to weight loss (NICE, 2004a) and the self-harm (NICE, 2004b). Patient A was offered education into her self-harming behaviours and offered different methods to cope with her stressors, she was also encouraged to be open about her self-harm so that staff can help her in the treatment and maintain her safety.
The next stage would be to plan the care for the patient (Kneisl et al., 2004). This should focus on the outcomes that have been identified during assessment and that plans should look to treat the patient in a safe, effective and timely manner (Fortinash & Worret, 2004). When care planning is conducted correctly it can be fundamental in the development of a therapeutic relationship (Shatell et al., 2007). Care plans should be developed with the client’s wants and needs being paramount in the process (NICE, 2011). Thus, adhering to the DoH’s (2010) strive to implement ‘no decision about me, without me’ into all patient’s care. Consequently, evidence supports this approach (Gould, 2012; Hiskey, 2012; Barry & Edgman-Levitan, 2012) through suggesting the inclusion of clients and carers in care planning can improve adherence, promote a positive outcome and increase patient satisfaction.
Care plans offer individualised care (NICE, 2016) and are the means of planning, implementing and evaluating care. It is vital that when developing these that the decisions made are evidence based so that the best care available is being delivered (Gordon & Watts, 2011; Melnyk & Fineout-Overholt, 2008). Care pathways can offer an excellent point of reference when seeking evidence due to them being developed through thorough utilisation of evidence based practice (Cavlan et al., 2011; Courtney & McCutcheon, 2009). The care plans were formulated with Patient A to focus on the restoration of weight, this was done by taking the recommendations from NICE (2004a) at aiming for an increase of 0.5-1kg each week. In order to promote this Patient A was given the opportunity to discuss with the dietician the plans that will be put in place to achieve this by looking to increasing her calorie intake by 3500-7000 calories per week (NICE, 2004a). Weight gain would be monitored each week at a weekly weighing. This would be taken as a dry weight upon rising and would be observed by a member of staff to reduce the risk of Patient A falsifying her weight (Royal College of Psychiatrics (RCP), 2014; Jaffa et al., 2011). As recommended by NICE (2004a) a chart which plotted Patient A’s weight change in relation to body growth was kept as a point of reference to determine actual body weight against recommended body weight so improvement or decline could be measured.
Patient A’s physical observations was monitored initially four times per day and recorded on an Early Warning Score Chart (NICE, 2004a). This was due to Patient A’s low blood pressure and heart rate upon admission. However, after a period of admission and due to an increase in both this was reduced to once daily at request of Patient A and discussion in the multidisciplinary team (MDT), who should be consulted when making decisions on patient’s care (DoH, 1983). Patient A was also prescribed thiamine and multivitamins in accordance with NICE guidelines (2004a) and supporting evidence from the RCP (2004). Patient A also underwent blood testing on a daily basis upon admission whilst checking for refeeding syndrome (NICE, 2006; Mehanna et al., 2008). Once Patient A was no longer at risk of refeeding syndrome it was agreed to reduce blood monitoring to once weekly. This was not only used to monitor Patient A’s physical health but as a way of determining if Patient A had been participating in any compensatory behaviours (NICE, 2004a); such as water loading, excessively exercising and instigating vomiting. If this was the case then Patient A would be challenged in regards to these behaviours. It could be at this point that the nurse could utilise the blood results as evidence alongside the section 3 to implement care plans, which had Patient A’s best interests in thought (DoH, 1983; NICE, 2004a). It was decided on numerous occasions that Patient A’s care plans would be altered to introduce a locked bedroom and bathroom aspect to reduce the risk of vomiting.
The treatment of Patient A’s AN was not only focused around the physical aspect of her illness but also through the use of psychological therapies and education. NICE (2004a) recommend that at least one psychological intervention should be implemented. The decision was made to offer Patient A cognitive behavioural therapy (CBT) which has been recognised as an effective intervention in the treatment of AN (NICE, 2004a; Fairburn, 2005; Watson & Bulik, 2013); with studies providing evidence for positive outcomes for the majority of clients who agree to undergo the treatment (Ball & Mitchell, 2004; Carter et al., 2009). However, it must be considered that the effectiveness of CBT is heavily reliant on the patient’s motivation to change (NHS, 2014; RCP, 2013) which could be problematic when caring for those in the early stages of AN who lack insight into their illness. Due to Patient A also suffering from low-mood the need was highlighted to improve this, especially as Patient A was currently using self-harm as a coping strategy. An immediate method to alleviate her mood would be through the use of an antidepressant medication. However, due to Patient A’s low weight it would not be recommended to start on an antidepressant as they can often cause nausea, a loss of appetite and weight loss (NHS, 2015) as well as evidence showing that they can have a negative impact on bone density in AN patients (Misra et al., 2010; Vestergaard et al., 2008). Research has also shown that the use of antidepressants when caring for those who are severely underweight is often ineffective in aiding recovery (Ferguson et al., 1999; Holtkamp et al., 2005). Contrariwise, evidence has supported the use of Olanzapine in the treatment of AN (Dunican & Del Dotto, 2007); however, due to Patient A being under the age of 18 this would only be prescribed if there was deemed to be no other alternative (NHS, 2016). For this reason the decision was made not to prescribe Patient A an antidepressant but instead utilise the transferrable skills attained in the CBT (NHS, 2014), which is recognised as being as effective as medication in the treatment of depression (RCP, 2013; NHS, 2014) and the improvement of mood.
AN is recognised as an illness that heavily effects the carers involved (NICE, 2004a; RCP, 2004) and it is vital the nurse is able to recognise the importance of the carer in the recovery process (Royal College of General Practitioners (RCGP), 2013). Yet, controversially it is often that the carers’ needs are neglected throughout the journey of the patient (Graap et al., 2008; RCP, 2004); which can result in a poorer deliverance of care (RCGP, 2013). Furthermore, evidence shows that when carers needs are addressed the recovery process can be aided and stressors reduced (Raenker, et al., 2013; RCGP, 2013). NICE (2004a) recommend the use of family therapies in the treatment of AN; which is supported by Watson and Bulik (2013) who completed a review of randomised controlled trials to distinguish that in most cases family based interventions were effective in the treatment of AN and other eating disorders. It has been reported that it can be as effective as CBT in the treatment of AN (Ball & Mitchell, 2004) and is deemed as being salient in the treatment of younger patients due to them often being more reliant on their carer (RCP, 2004).
When involving the main carer of Patient A in her treatment it was important to first of all to ensure it was appropriate to do so (NICE, 2004a). It was through the assessment period that it is was evident that Patient A was heavily reliant on her carer for support and it was obvious that their life had been taking over by the illness. This provided a strong rationale to introduce family therapy along with other methods of care delivery; which were specifically tailored to Patient A and her carer, therefore, providing a better chance of promoting a positive outcome (Ewing et al., 2015). Patient A’s carer was invited to attend meal support groups, which has been highlighted as one of the cornerstones of the treatment of eating disorders (DeSantis, 2002; Noorduin & Vandereycken 2003; Couturier & Mahmood, 2009). Patient A’s care also involved the inclusion of the outreach team to educate how AN might manifest in certain situations and the best ways to challenge the illness at these times. It was also evident the Patient A’s carer would benefit from extra support in regards to living with a loved one who suffers from an eating disorder; so they were invited to attend a carer support group. Carer support groups are deemed as an effective method in which to educate the care giver and give carers an opportunity to share the stories and coping strategies (RCP, 2004; NICE, 2004a; Whitney et al., 2005); Treasure et al. (2005) also reported feedback from carers who identified it is very important in coping with the difficult times and a necessity in the recovery process.
By adopting a The Care Programme Approach (CPA) (DoH, 2008) into the delivery of care this ensures that a holistic approach is adopted and that the patient can be as involved in the care as their illness allows them. Whilst care is continually evaluated in weekly MDT meetings the CPA allows for care to be discussed in further detail; with inclusion of a wider team and carers. In Patient A’s case a CPA meeting was organised every six weeks, it was here that her progress would be discussed; taking into account the biopsychosocial approach. Plans could then be made with all of the MDT, carers and Patient A present; thus, the care that was to be delivered would be agreed on whilst taking into account the wants and needs of all involved. With evidence providing backing that this vital in promoting a therapeutic relationship (Barry & Edgman-Levitan, 2012; Gould, 2012). It also important when implementing the CPA that an effective MDT is in place and recommended more so in eating disorders due to the complexity of the illness (Rome et al., 2003; Kaplan, 2002); in Patient A’s cases this included a vast amount of professionals from different fields which ensured all of her biopsychosocial needs were considered.
The development of a therapeutic relationship is unique in the outcome of a patient’s care (Hiskey, 2012) and if the bond is positive the outcome will be likewise. The importance of being aware of that what works for one person might not work for another should always be considered (Dziopa & Ahern, 2009); and that assuming this could potentially hinder the development. Whilst it is important to consider how holistic care, having an effective MDT and patient involvement can help develop the therapeutic relationship (Barry & Edgaman, 2012; Gould, 2012; Shatell et al., 2007); the nurse should also be aware of their own impact on the development of a therapeutic relationship. The building of trust should be the cornerstone to this (Bloomfield & Pegram, 2015; Shatell et al., 2007) this can be established through staff interactions, offering empathetic care and being honest (Carter, 2009; Dziopa & Ahern, 2009); which will result in the nurse being able to fulfil their role as an advocate for the patient in their time of need (NMC, 2015). The nurse must be self-aware throughout interactions and utilise their therapeutic skills; such as mirroring, paraphrasing and summarising the conversation (Stickley & Freshwater, 2006), to help make the patient feel relaxed and valued. The building of the therapeutic relationship with Patient A started on her admission to the ward when she was assigned a key nurse and co-worker; time would be set aside for Patient A to meet up and discuss her issues and plan care to help her recovery. Patient A would also be given chance to reflect on this time and the honesty that was encouraged would continue to build the relationship.
At the time of this case study Patient A still remains an inpatient but there has been considerable improvement recognised. Patient A has managed to put weight on and is now currently in the green zone of the MARSIPAN Guidelines (Ayton et al., 2015). There has also been a reduction in Patient A’s self-harming behaviours. It is still apparent that Patient A’s recovery is in the early stages and that work is still ongoing in regards to ensure improvements continue. However, it is evident from the discussion that Patient A is receiving the most appropriate care and evaluation is constantly ongoing to ensure this remains the case.
References
Ayton, A. et al. (2015). Summary of Junior MARSIPAN: Management of Really Sick Patients under 18 with Anorexia Nervosa. The Royal College of Psychiatrists.
Ball, J. & Mitchell, P. (2004). A randomized controlled study of cognitive behavior therapy and behavioral family therapy for anorexia nervosa patients. Eating Disorders.12, 303-314.
Barry, M. & Edgman-Levitan, S. (2012). Shared Decision Making – The Pinnacle of Patient-Centred Care. The New England Journal of Medicine. 366(9), 780-781.
Blinder, B. et al. (2006). Psychiatric Comorbidities of Female Inpatients With Eating Disorders. Psychosomatic Medicine. 68, 1-9.
Bloomfield, J and Pegram, A. (2015). Care, compassion and communication. Nursing Standard. 29 (25), 45-50.
Brimblecombe, N., Tingle, A., Tunmore, R. & Murrells. (2007). Implementing holistic practices in mental health nursing: A national consultation. International Journal of Nursing Studies. 44, 339-348.
Carter, J. et al. (2009). Maintenance Treatment for Anorexia Nervosa: A Comparison of Cognitive Behavior Therapy and Treatment as Usual. International Journal of Eating Disorders. 42, 202-207.
Cavlan, O. et al. (2011). Using care pathways to improve health systems. Health International. 11, 6-17.
Cleary, M., Hunt, G., Horsfall, J. & Deacon, M. (2012). Nurse-Patient Interaction in Acute Adult Inpatient Mental Health Units: a Review and Synthesis of Qualitative Studies. Issues in Mental Health Nursing. 33, 66-79.
Connan et al. (2003). A neurodevelopmental model for anorexia nervosa. Physiology & Behevior. 79, 13-24.
Courtney, M. & McCutcheon, H. (2010). Using Evidence to Guide Nursing Practice. 2nd ed. Elsevier, Australia.
Couturier, J. & Mahmood, A. (2009). Meal Support Thereapy Reduces the Use of Nasogastric Feeding for Adolescents Hopitalized with Anorexia Nervosa. Eating Disorders. 17, 327-332.
Crook, M., Hally, V. & Panteli, J. (2001). The Importance of the Refeeding Syndrome. Nutrition. 17(8), 632-637.
Dallos, R. & Johnstone, L. (2014). Formulation in Psychology and Psychotherapy: Making sense of people’s problems. 2nd Ed. Routledge, London.
Department of Health. (1983). Mental Health Act 1983. Available from: www.legislation.gov.uk/ukpga/1983/20/contents (Accessed 23rd May 2018).
Department of Health. (2002). The Single Assessment Process. The Stationery Office, London.
Department of Health. (2008). Refocusing the Care Programme Approach: Policy and Positive Practice Guidance. Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_083649.pdf (Accessed 30th May 2018).
Department of Health. (2010). Equity and excellence: Liberating the NHS. Available from: www.gov.uk/government/publications/liberating-the-nhs-white-paper (Accessed 25th May 2018).
DeSantis, A. (2002). Therapeutic mealtime support: A treatment strategy for disordered eating. Pulse. 21(4), 4-5.
Disability Rights Commission. (2006). Equal Treatment: Closing the Gap: A Formal Investigation into the Physical Health Inequalities Experienced by People with Learning Disabilities and/Or Mental Health Problems. DRC, London.
Dunican, K. & Del Dotto, D. (2007). The Role of Olanzapine in the Treatment of Anorexia Nervosa. The Annals of Pharmacotherapy. 41, 111-115.
Dziopa, F. & Ahern, K. (2009). Three Different Ways Mental Health Nurses Develop Quality Therapeutic Relationships. Issues in Mental Health Nursing. 30, 14-22.
Ewing, G., Austin, L., Diffin, J. & Grande, G. (2015). Developing a person-centred approach to carer assessment and support. British Journal of Community Nursing. 20(12), 580-584.
Fairburn, C. (2005). Evidence-Based Treatment of Anorexia Nervosa. International Journal of Eating Disorders. 37, 26-30.
Fan, X. et al. (2006). An Exploratory Study about Inaccuracy and Invalidity in Adolescent Self-Report Surveys. Field Methods. 18(3), 223-244.
Ferguson, C. et al. (1999). Are Serotonin Selective Reuptake Inhibitors Effective in Underweight Anorexia Nervosa. International Journal of Eating Disorders. 25(1), 11-17.
Fortinash, K. & Worret, P. (2003). Psychiatric nursing care plans. 4th Ed. Mosby, St. Louis.
Fortinash, K. & Worret, P. (2004). Psychiatric Mental Health Nursing. 3rd Ed. Mosby, St. Louis.
Garner, D. (2004). Eating Disorder Inventory-3. Professional Manual. Psychological Assessment Resources, Florida.
Gordon, W. & Watts, C. (2011). Applying skills and knowledge: Principle of Nursing Practice F. Nursing Standard. 25(33), 35-37.
Gould, D. (2012). Service users’ experiences of recovery under the 2008 Care Programme Approach. London: Mental Health Foundation.
Graap et al. (2008). The Needs of Carers of Patients with Anorexia and Bulimia Nervosa. European Eating Disorders Review. 16, 21-29.
Grover, C., Robin, J. & Gharahbaghian, L. (2012). Anorexia Nervosa: A Case Report of a Teenager Presenting with Bradycardia, General Fatigue, and Weakness. Pediatric Emergency Care. 28(2), 174-177.
Hiskey, S. (2012). Time to re-evaluate the therapeutic relationship. Mental Health Practice. 15(5), 34-35.
Holt, J. & Convey, H. (2012). Ethical practice in nursing care. Nursing Standard. 27(13), 51-56.
Holtkamp, K. et al. (2005). A retrospective study of SSRI treatment in adolescent anorexia nervosa: insufficient evidence for efficacy. Journal of Psychiatric Research. 39(3), 303-310.
Jaffa, T., Davies, S. & Sardesai, A. (2011). What Patients with Anorexia NervosaShould Wear When They Are Being Weighed: Report of Two Pilot Surveys. European Eating Disorders Review Journal. 19, 368-370.
Kaplan, A. (2002). Psychological Treatments for Anorexia Nervosa: A Review of Published Studies and Promising New Directions. Canadian Journal of Psychiatry. 47, 235-242.
Kneisl, C., Wilson, H. & Trigoboff, E. (2004). Contemporary Psychiatric-Mental Health Nursing. Pearson Education, New Jersey.
McCabe, M. et al. (2006). Accuracy of body size estimation: Role of biopsychosocial variables. Body Image. 3, 163-171.
Mehannha, H., Moledina, J. & Travis, J. (2008). Refeeding syndrome: what it is, and how to prevent and treat it. British Medical Journal. 336, 1495-1498.
Melnyk, B. & Fineout-Overholt, E. (2008). The evidence-based practice beliefs and implementation scales: psychometric properties of two new instruments. Worldviews on Evidence-Based Nursing. 5(4), 208–216.
Misra, M. et al. (2010). Use of SSRIs may Impact Bone Density in Adolescent and Young Women with Anorexia Nervosa. CNS Spectrums. 15(9), 579-586.
National Institute for Health and Care Excellence. (2017). Eating disorders: recognition and treatment Available from: https://www.nice.org.uk/guidance/ng69. (Accessed 25th May 2018).
National Institute for Health and Care Excellence. (2004). Self-harm in over 8s: short-term management and prevention of recurrence. Available from: http://www.nice.org.uk/guidance/cg16/chapter/1-Guidance#issues-for-all-services-and-healthcare-professionals. (Accessed 29th May 2018).
National Institute for Health and Clinical Excellence. (2006). Nutrition support in adults: oral nutrition support, enteral tube feeding and parenteral nutrition. Available from: www.nice.org.uk/page.aspx?o=cg032. (Accessed 28th May. 2018).
National Institute for Health and Clinical Excellence. (2011). Service user experience in adult mental health services. Available from: https://www.nice.org.uk/guidance/qs14/chapter/quality-statement-8-care-planning. (Accessed 28th May 2018).
National Institute for Health and Clinical Excellence. (2016). Care Pathways. Available from: https://www.nice.org.uk/About/What-we-do/Our-Programmes/About-NICE-Pathways. (Accessed 28th May 2018).
NHS. (2014). Cognitive behavioural therapy (CBT) – Considerations. Available from: http://www.nhs.uk/Conditions/Cognitive-behavioural-therapy/Pages/Advantages.aspx. (Accessed 28th May 2018).
NHS. (2015). Selective serotonin reuptake inhibitors (SSRIs) – Side effects. Available from: http://www.nhs.uk/Conditions/SSRIs-(selective-serotonin-reuptake-inhibitors)/Pages/Side-effects.aspx. (Accessed 30th May 2018).
NHS. (2016). Anorexia Nervosa. Available from: http://www.nhs.uk/Conditions/Anorexia-nervosa/Pages/Introduction.aspx. (Accessed 29th May 2018).
NHS. (2016). Anorexia Nervosa – Complications. Available from: http://www.nhs.uk/Conditions/Anorexia-nervosa/Pages/Complications.aspx. (Accessed 26th May 2018).
NHS. (2016). Anorexia Nervosa – Treatment. Available from: http://www.nhs.uk/Conditions/Anorexia-nervosa/Pages/Treatment.aspx. (Accessed 30th May 2018).
Noorduin, C. & Vandereycken, W. (2003). Coping with stressful family meals. Patients, parents and therapist around the table. Eating Disorders Review. 14(6), 1-3.
Nursing and Midwifery Council. (2015). The Code – Standards of Conduct, Performance and Ethics for Nurses and Midwives. London: NMC.
Papadopoulos, F., Ekbom, A., Brandt, L. & Ekselius, L. (2009). Excess mortality, causes of death and prognostic factors in anorexia nervosa. The British Journal of Psychiatry. 194, 10-17.
Raenker et al. (2013). Caregiving and Coping in Carers of People with Anorexia Nervosa admitted for Intensive Hospital Care. International Journal of Eating Disorders. 46, 346-354.
Robinson, B. (2009). When therapists variables and the client’s theory of change meet. Psychotherapy in Australia. 15(4), 60-65.
Rome et al. (2003). Children and Adolescents With Eating Disorders: The State of the Art. Pediatrics. 111(1), 98-108.
Royal College of General Practitioners. (2013). RCGP Supporting Carers in General Practice: Summary Report on GP practice journeys towards improved carer identification support. Available from: http://www.rcgp.org.uk/~/media/EFE191B727514B66909FEED20FF23E1F.ashx. (Accessed 30th May 2018).
Royal College of Psychiatrics. (2004). Eating Disorders: Core interventions in the treatment and management of anorexia nervosa, bulimia nervosa, and related eating disorders. Available from: http://www.ncbi.nlm.nih.gov/books/NBK49304/pdf/Bookshelf_NBK49304.pdf. (Accessed 30th May 2018).
Royal College of Psychiatrics. (2013). Cognitive Behavioural Therapy. Available from: http://www.rcpsych.ac.uk/mentalhealthinformation/therapies/cognitivebehaviouraltherapy.aspx. (Accessed 29th May 2018).
Royal College of Psychiatrics. (2014). MARSIPAN: Management of Really Sick Patients with Anorexia Nervosa. 2nd Ed. Royal College of Psychiatrics.
Sassaroli, S. et al. (2008). Perfectionism in depression, obsessive-compulsive disorder and eating disorders. Behaviour Research and Therapy. 46, 757-765.
Shatell, M., Starr, S. & Thomas, S. (2007). ‘Take my hand, help me out’: Mental health service recipients’ experience of the therapeutic relationship. International Journal of Mental Health Nursing. 16, 274-284.
Stickley, T. & Freshwater, D. (2006). The art of listening in the therapeutic relationship. Mental Health Practice. 9(5), 12-18.
The Sainsbury Centre for Mental Health. (2001). The Capable Practitioner. SCMH, London.
Treasure et al. (2005). Working with families of adults with anorexia nervosa. Journal of Family Therapy. 27, 158-170.
van de Mortel, T. (2008). Faking it: social desirability response bias in self-report research. Australian Journal of Advanced Nursing. 25(4), 40-48.
Vestergaard, P., Rejnmark, L. & Mosekilde, L. (2008). Selective Serotonin Reuptake Inhibitors and Other Antidepressants and Risk of Fracture. Calcified Tissue International. 82, 92-101.
Ward, L. (2011). Mental health nursing and stress: Maintaining balance. International Journal of Mental Health Nursing. 20, 77-85.
Watson, H. & Bulik, C. (2013). Update on the treatment of anorexia nervosa: review of clinical trials, practice guidelines and emerging interventions. Psychological Medicine. 43, 2477-2500.
Webb, G. et al. (2011). Complications of Emergency Refeeding in Anorexia Nervosa: Case series and review. Acute Medicine. 10(2), 69-76.
Weerasekara, P. (1995). Multiperspective Case Formulation. Krieger, Florida.
Whitney, J. et al. (2005). Experience of caring for someone with anorexia nervosa: qualitative study. British Journal of Psychiatry. 187, 44-449.
World Health Organization. (1992). The ICD-10 Classification of Mental and Behavioural Disorders. Diagnostic criteria for Research. Geneva.
Yahalom, M. et al. (2013). The Significance of Bradycardia in Anorexia Nervosa. The International Journal of Angiology. 22, 83-94.
 Appendices
Appendices
 Appendix 1
Appendix 1
Appendix 2
| # | Query | Limiters/Expanders | Last Run Via | Results |
| S18 | S14 AND S15 | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
1,229 |
| S17 | S13 AND S15 | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
2,040 |
| S16 | S13 AND S14 | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
398 |
| S15 | S8 OR S9 OR S10 | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
106,149 |
| S14 | S4 OR S6 | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
7,897 |
| S13 | S1 OR S2 OR S7 | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
29,409 |
| S12 | formulation | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
9,499 |
| S11 | nursing process | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
6,898 |
| S10 | sad | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
1,503 |
| S9 | depression | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
104,844 |
| S8 | low mood | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
339 |
| S7 | low weight | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
15,594 |
| S6 | family therapy | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
5,374 |
| S5 | refeeding syndrome | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
241 |
| S4 | cbt | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
2,599 |
| S3 | self-harm | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
1,934 |
| S2 | eating disorders | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
9,833 |
| S1 | anorexia | Search modes – Boolean/Phrase | Interface – EBSCOhost Research Databases Search Screen – Advanced Search Database – CINAHL Complete |
6,254 |
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Mental Health"
Mental Health relates to the emotional and psychological state that an individual is in. Mental Health can have a positive or negative impact on our behaviour, decision-making, and actions, as well as our general health and well-being.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




