The Stigma Behind BME Groups And Mental Health
Info: 22927 words (92 pages) Dissertation
Published: 13th Oct 2021
Tagged: Mental Health
Abstract
Statistics have shown that mental health stigma is rife within the Black and minority ethnic (BME) population. Due to limited research in this area, the aims of the study were to gain a deeper understanding from the BME perspective regarding the perceived stigma towards mental health, barriers to accessing mental health services and finding effective solutions in reducing mental health stigma as well as increasing access to mental health services. Through purposive sampling, participants comprised of three males and three females; three of afro-Caribbean descent and three from Asian and Arabic origin, all between the ages of twenty-one and twenty-six. Thematic analysis was conducted to identify key themes tailored to the research aims. The analysis identified five broad themes: lack of education in mental health, shaming and discrimination from social circles, poor support from family and friends, barriers to seeking help and improving BME access to mental health services. Results found was similar to previous studies; strengthening stigma literature. Although, sample consisted of university educated students. Overall, to reduce misconceptions about mental illness and prevent racial and in group discrimination, community awareness campaigns; increasing therapists from BME backgrounds and developing culturally adapted interventions would be beneficial.
CONTENTS
Abstract………………………………………………………….
Introduction………………………………………………………
Mental Health Stigma
Repercussions For Those Stigmatised With Mental Illness
The Lack Of Literature on Stigma and BME Communities
The Impact Of Stigma On BME Groups Receiving Treatment
Collectivist Culture v Individualistic Society
Barriers To Access To Mental Health Services And Treatments
But Why Are BME’s With Mental Health Issues Over-represented In The Criminal Justice System?
BME community Is Equally An Expert In Mental Health
The Present Study
Aims Of The Study
Methodology………………………………………………………
Design…………………………………………………….
Participants…………………………………………………
Materials…………………………………………………..
Pilot Study………………………………………………….
Procedure………………………………………………….
Ethical Considerations…………………………………………..
Data Analysis………………………………………………..
Reflexivity………………………………………………….
Results Analysis
Theme 1: No Such Thing As Mental Health In The BME Culture
Theme 2: In-Group Discrimination And Cultural Naivety
Theme 3: Lack Of Support From Family And Friends
Theme 4: Barriers To Seeking Help
Theme 5: Increasing BME Access To Mental Health Services
Discussion
Strengths…………………………………………………..
Limitations…………………………………………………
Unique Contribution……………………………………………
Practical Implications…………………………………………..
Conclusion
References………………………………………………………..
Appendices……………………………………………………….
Introduction
Mental health is a growing crisis in contemporary society; the rising number of children facing mental health problems has led to mounting pressure on acute services (Berry, 2017). Substance abuse addictions have had negative implications on public health, education and the penal system (Lynch, Nicholson, Dance, Morgan & Foley, 2010). Statistics conducted in England by NatCen show a 24% rise from 2007 to 2014 in adults aged 16-74 with conditions such as anxiety and depression accessing mental health services; people that were Caucasian, female or in mid-life (age 35-54) were more likely to receive treatment whereas Black and minority ethnicities (BME) had significant low treatment rates (“Adult Psychiatric Morbidity Survey”, 2017). Rehman and Owen (2013) led a survey on 740 ethnic minorities with mental health issues. Results showed that BME’s with mental illness had to deal with both racial and social discrimination; 73% of participants reported discrimination, where 49% were alarmingly directed from mental health staff. The survey also found BME individuals with mental illness experienced moderate to severe discrimination from their own community. This places importance in understanding why BME groups do not access mental health services; this study will thus explore mental health stigma as a significant factor for the BME population not accessing services.
Mental Health Stigma
The concept mental health has been a convoluted area of research. For Jorm (2000), mental health refers to the understanding of psychological disorders that can be aided by recognition, prevention and management. In need of revision, mental health has experienced a shift away from diseases and a focus towards positive psychological health; the World Health Organisation (WHO) defines mental health as a state of well-being in which every person understands their potential and is able to cope or adapt with stresses of everyday life whilst making a positive contribution to their community (Manderscheid, Ryff, Freeman, McKnight-Eily, Dhingra & Strine, 2010; “WHO | Mental health: a state of well-being”, 2017). Public and self-stigma has had a destructive impact on people struggling with mental health; patients are denied access to jobs, housing and health care, which are barriers to their respective recoveries (Corrigan, Thompson, Lambert, Sangster, Noel, & Campbell, 2003; Whitley, 2016). This is demonstrated in the work undertaken by Thornicroft (2007), which features many excerpts from people with mental illness showing how this has affected their home, personal, social and working life, for example Maria (pp. 125–6):
“I have never committed a crime, never hurt a fly
All at once, I am no longer welcome in my home.
Just because I have a mental health problem
I am now shunned.
My life made even more difficult to live”
(Thornicroft, 2007). Studies have shown social support from families, friends and education has had positive effects on reducing stigma for adults and adolescents with mental health (Corrigan et al, 2005; Corrigan, Morris, Michaels, Rafacz, & Rüsch, 2012).
However, family members frequently experience stigma as a result of their association with the individuals struggling with mental health; this is referred to as courtesy stigma where children, parents, siblings and spouses are commonly stigmatised (Goffman, 1963; Kjellin & Östman, 2005). Family stigma consists of public perceptions and often attributes poor parenting as the cause of a mental illness. In turn, family members feel shame for being solely blamed for the cause of the mental illness; this shame leads on to avoiding social contact and hiding issues in secrecy within family as well. As a result, the family reinforces mental health stigma as they avoid communication regarding the family member with the mental disorder and thus, the individual struggling suffers alone in silence (Larson & Corrigan, 2008).
Repercussions For Those Stigmatised With Mental Illness
People with mental health are simultaneously challenged with dealing with the symptoms from their disorders and the stigma attached to their mental illness (Corrigan & Watson, 2002). The term stigma is defined as a held perception of people involving three negative attributes. The first being poor attitudes that influence prejudice and later seclude groups. The second is behavioural actions like distancing yourself from people with mental illness. The final attribute is discriminative remarks where a lack of knowledge about people with mental illness leads onto ignorant statements (Corrigan & Watson, 2002; Thornicroft, Rose, Kassam & Sartorius, 2007). Mental health stigma is rather a complex phenomenon that can be divided into two categories: public (external) and self-stigma (internal) (Corrigan, Scmidt, Bink, Nieweglowski & Al-Khouja, 2016; Gray, 2002). Literature has characterised public stigma as comprising of negative reactions and unfair treatment of the general public towards the individual with a mental illness, which leads onto isolation and restriction to social support. Whereas self-stigma focuses on the person having negative beliefs of themselves, primarily focusing on the shame and embarrassment; which in turn prevents individuals with a mental illness from speaking about their issues and seeking help (Corrigan, Lurie, Goldman, Slopen, Medasani & Phelan, 2005; Dinos, 2004; Drapalski, Lucksted, Perrin, Aakre & DeForge, 2013; Gray, 2002; Rusch, Angermeyer & Corrigan, 2005; Rüsch, Corrigan, Todd, & Bodenhausen, 2010).
The Lack Of Literature on Stigma and BME Communities
Despite extensive research on mental illness and possible interventions to address stigma, previous literature on mental illness within Black and Minority Ethnic (BME) groups have been neglected due to poor empirical support and a lack of scientific research evidence (Alvidrez, Snowden & Kaiser, 2008; Knifton, 2012; Knifton, Grvais, Newbigging, Mizra & Quinn, 2009; Memon, Taylor, Mohebati, Sundin & Cooper, 2016). For instance Crisp, Gelder, Rix, Meltzer & Rowlands (2000) study focused on the opinions of the British public regarding mental illness; results showed respondents commonly perceived individuals with alcoholism, schizophrenia and drug addiction as dangerous and unpredictable. However, 26% of the BME groups contacted refused to be interviewed and 95% of the sample used was white, therefore, the sample contained insufficient numbers from BME people to represent their views. Crisp et al (2000) proposed that the BME individuals who refused were possibly influenced by personal sensitivities to self-revelation; this is reflected in their attitudes to people with mental illnesses. Although, within the last decade or so, there has been an attempt to rectify this; evidence from middle and low-income countries are virtually absent compared to high economically developed countries such as the UK, where stigma is stronger in BME communities due to complex and cultural factors (Hanely & Brown, 2013; Knifton, 2012). Statistics also show that there is an overrepresentation of BME people admitted to mental health inpatient units (Denzel, van Esch, Harte, & Scherder, 2016). Upon until recently, there has been extensive research focusing on the stigma attached to mental health and finding adequate solutions to counter this issue (Corrigan, Bink, Schmidt, Jones, & Rüsch, 2015; de Freitas, 2013; Thornicroft, 2007; Thornicroft, Mehta, Clement, Evans-Lacko, Doherty, 2015).
The Impact Of Stigma On BME Groups Receiving Treatment
Within the last decade, a few researchers to varying success have attempted to produce literature and sufficient evidence, which highlight the effects of stigma on BME communities (Knifton, 2012; Kinfton et al., 2009; Memon et al., 2016). Questionnaires measuring 257 BME individual’s attitudes, behavioural intent and knowledge about mental health from Knifton et al., (2009) study suggested that stigma within BME groups are shaped by experiences of racism and migration. On one hand, Asian families feared mental health issues would compromise their inability to fulfil everyday family obligations like household chores or holding a job; this was deemed embarrassing and unacceptable as this impacts their family reputation (Karim, Saeed, Rana, Mubbashar, & Jenkins, 2004). On the other hand, Chinese participants hid mental health problems and avoided treatments due to the fear and belief of their family being exposed can lead to disgrace inhibiting them tackling their mental health issues (Li, Lee, Chieu, & Kleinman, 2005).
Shefer, Rose, Nellums, Thornicoft & Henderson (2013) found that the BME groups emphasised stigma and a lack of knowledge in mental health as significantly apparent in their community; their native countries are traditionally religious where there is a focus on rituals and removing evil spirits out of the person whom may potentially be struggling with a mental issue. Qualitative studies conducted in recent years emphasise these perceptions where conceptualisation of mental health stigma derive from evil spirits and witchcraft; thematic analysis used in such studies highlighted community stigma and negative labels towards the mentally ill are brought on by ones sinful life and as a result suffer from mental health issues (Islam & Campbell, 2012; Thomas, Tol, Vallipuram, Sivayokan & Jordans, 2016). For example, Hanely & Brown (2013) discovered in Arabic cultures that Jinn are evil spirits that cause physical and emotional distress at times of vulnerability such as postnatal illness; jinn-possession is a result of an individual making morally wrong or sinful choices. Contrastingly, thematic analysis found there was no connection found between supernatural causes such as jinn, Satan and mental illness in Islam & Campbell’s (2013) study; instead the Qur’an mentions madness (spiritual insanity) sustained from sin. This suggests that more research is needed in the future to have further understanding with the impact of jinn-possession on mental illnesses.
Additionally, Memon et al., (2016) found BME groups were unable to recognise symptoms of mental illnesses and possible diagnosis of a mental health disorder, which causes social isolation from both family and friends and standing in the community. Furthermore, people from BME backgrounds felt the financial costs of possible therapeutic interventions were too expensive since majority of BME individuals were from poor socio-economic backgrounds (Dardas & Simmons, 2015; “National Institute for Mental Health in England”, 2003). This suggests that concerns regarding stigma prompted BME individuals to either avoid or delay treatment for mental health issues (Alvidrez, Snowden & Kaiser, 2008). It should be noted that Memon et al. (2016) study primarily contained university-educated participants that may not represent all BME people. However, this study’s method of focus groups involved people from diverse BME backgrounds making the research generalizable for the BME society overall.
Collectivist Culture v Individualistic Society
Another significant aspect of mental health stigma is cultural differences. Papadopoulos, Foster & Caldwell (2012) study proposed that people from ‘collectivist’ cultures such as; Greek, Greek Cypriot and Chinese were more likely to hold stigmatising attitudes towards mental illness compared to Caucasian people who are traditionally from ‘individualistic’ cultures like the USA and UK (Markus & Kitayama, 1998). Using snowball sampling and a quantitative questionnaire survey of 305 individuals from four UK based cultural groups. Results revealed that the more stigmatizing a culture’s mental illness attitudes are, the more likely collectivism effectively explains these attitudes. One major setback of this study is it fails to add people from BME backgrounds such as Africans and Latin Americans that are predominantly from collectivist cultures. The ‘individualism-collectivism’ was best explained by Markus & Kitayama, (1998) who argued that individualistic cultures are more likely to embrace diversity and uniqueness as a result of seeking personal goals whereas in collectivist cultures there is a desire for in-group goals; once an individual strays from this norm, they are highly visible within the community and existing connections are lost. Previous literature indicates that as a consequence, family members within BME communities will attempt to hide relatives with a mental illness and in turn prevents them accessing necessary mental health services; this is where more apparent stronger negative attitudes and lack of knowledge derive from (Galletly & Burton, 2011; Papadopoulos, Tsai, Alsbiei, O’Brien, & Schwab, 2002; Pettigrew & Tropp, 2006).
Barriers To Access To Mental Health Services And Treatments
Conclusive evidence has proved ethnic minorities generally experience greater psychological distress and receive poorer quality care (Alegría, Mulvaney-Day, Torres, Polo, & Cao, 2007; Gone & Trimble, 2012; Harris, Edlund, & Larson, 2005; Snowden & Yamada, 2005). For example, white Americans are particularly liable to receiving good mental health care compared to Black and Latino Americans (Cook, McGuire, & Miranda, 2007; Cook, McGuire, Lock & Zaslavsky, 2010). Duffin (2008) showed that mistrust among mental health services and BME is partly associated with BME’s believing they are more likely to be sanctioned than Caucasian people. It was also claimed that BME people often have no access to talking therapies or counselling. This is supported by Henderson, Williams, Gabbidon, Farrelly & Schauman, 2014; Memon et al., 2016; Schwartz & Blankenship, 2014; Sue, Capodilupo, Torino, Bucceri & Holder, (2007) who stressed that there is language and communication barriers where there is a lack of fluent English from the patient; this makes BME individuals feel that they have to be submissive to an experienced doctor who may be perceived as more superior to them. This is unfamiliar to BME’s and may explain why they struggle and show hesitant behaviour. Subsequently, doctors are incapable of listening to their needs, as BME groups are reluctant to engage with mental health services on behalf of family and friends due to this barrier. As a result, mental health issues are a matter for the family and privacy is favoured instead of seeking clinical help because of prevalent discrimination felt by BME groups (Carpenter-Song, Chu, Drake Ritsema & Smith, 2010; Burgess, Ding, Hargreaves, Van Ryn, & Phelan, 2008; Sue et al., 2007).
But Why Are BME’s With Mental Health Issues Over-represented In The Criminal Justice System?
As mentioned earlier, the overrepresentation of BME people in the mental health system is of significant importance to the understanding of mental health stigma within the BME community (Bhui, Aslam, Palinski, McCabe & Johnson, 2015; Hatch, Gazard, Williams, Frissa & Goodwin, 2016; Raleigh, Irons, Hawe, Scobie, & Cook, 2007; Saltus, Ba, Msc, Jarvis, & Duval, 2013). The 2005 Healthcare Commission census of mental health patients in England and Wales, found around 9% of inpatients were black, despite the fact that black people comprise just 2.2% of the population according to government figures (Home Commission, 2005; “The criminal justice system,” 2007). The 2006 census also revealed admission rates for black people into mental health care were three times higher on average than other groups (Office for National Statistics, 2003; “The criminal justice system,” 2007). Scientific evidence show BME patients are more likely to experience compulsory admission to in-patient care services via criminal justice system whether it be through the courts, prison or home office and involve police force and brutality (Bhui, Stansfeld, Hull, Priebe, & Mole, 2003; Vinkers, de Vries, van Baars, & Mulder, 2009; de Wit, Tuinebreijer, van Brussel, & Selten, 2010). There is also evidence for higher prevalence rates of psychotic disorders in BME groups in contrast to non-BME groups; they experience difficulties getting into adequate treatment and as a result there is an overrepresentation of BME detainees with psychotic disorders within mental health services due to many BME’s accessing primary mental health care facilities (Denzel, van Esch, Harte & Scherder, 2016).
BME community Is Equally An Expert In Mental Health
There is substantial evidence that propose user involvement rather than merely being beneficiaries in the delivery and treatment of mental health services as the key to successful engagement of therapeutic interventions (Bee, Brooks, Faser & Lovell, 2015; Peck, Gulliver, & Towell, 2002). Henderson, Flood, Leese, Thornicroft & Sutherby, (2004) study showed a joint crisis intervention plan formulated by patient and health professionals resulted in reduced rates of enforced admission of individuals with severe mental illness, increased user esteem and the ability to empower people struggling with mental health to regain greater control over their recovery and care. With the BME population participating in the planning and provision of care, there is a higher likelihood of reduced compulsory admission with severe mental illness and thus less days spent in inpatient care (Crawford, 2002; Henderson et al., 2004; Simpson & House, 2003; Thornicroft & Tansella, 2005). Patient involvement in personal care planning (PPI) has seen promising results and is an effective help for patients. However there is room for improvement in research for its effectiveness for specific patient groups such as BME (Coulter, Entwistle, Eccles, Ryan & Shepperd, 2015; Ennis & Wykes, 2013; Hibbard & Greene, 2013).
The Present Study
Overall, literature has focused on stigma and mental health but not substantially from BME perspectives. As discussed above, ethnic minorities are underrepresented in prior research and the effects of stigma in these communities have been severely neglected (Crisp et al., 2000; Saltus, et al, 2013). BME individuals with mental illness feel local primary care systems in place are not pluralistic and fair. This creates a barrier for ethnic minorities accessing mental health support programmes, as they are unable to receive the necessary treatment required (Donner, Mutter & Scior, 2010; Kovandžić, Chew-Graham, Reeve, Edwards & Peters, 2011; Pole, Gone, & Kulkarni, 2008).
BME groups prefer therapeutic interventions that have been culturally adapted where mental health professionals are from ethnic minorities. Due to the culturally adapted interventions only being something that has happened recently therefore there is not enough research evidence to empirically support it’s effectiveness (Bhui et al, 2015; Cardemil, Nelson & Keefe, 2015; Dardas & Simmons, 2015; Sue, Zane, Nagayama Hall, & Berger, 2009). They also favour an anti-stigma intervention that engages the whole community and aims to educate people in regards to mental health (Shefer et al., 2013; Memon et al., 2016; Knifton, 2012; Knifton et al., 2009). In addition to this, Islam, Rabiee & Singh (2015) found that for many BME groups, they prefer seeking help from a faith/ spiritual leader before taking medical advice and intervention suggesting that religious leaders incorporated into intervention plans will be useful for the BME community and accelerate access to treatments.
Studies such as Shefer et al., (2012) and Memon et al., (2016) suggest prompting and guiding can not work as effectively due to the difficulty of people becoming influenced by others opinions; hence, it is appropriate to use directive semi structured interviews as stigma is very personal. This is essential in understanding BME group’s views on why they feel stigma is attached to mental health. This present study can inform other researchers in stigma literature about BME people and the issues they face so suitable and effective treatments could be implemented for this community.
Aims Of The Study
The aims of this study are to find out:
- BME group’s experiences and perception regarding stigma attached to mental health,
- Explanations for why the BME community are not accessing primary and secondary mental health services,
- And what the BME community think are effective solutions to increasing access to mental health services.
Methodology
Design
The study was qualitative using semi-structured interviews; centred on an interview guide (Appendix A), it was developed to encourage participants to speak openly and honestly (Nielson, 2007). A qualitative framework such as this was the most appropriate method as previous works on this topic were mostly quantitative and descriptive due to a lack of research from BME communities; hence the nature of the study required an in-depth design. In need for more depth and detailed data from people’s personal accounts; the researcher can then ask for more clarification and elaboration (DiCicco-Bloom and Crabtree, 2006; Cridland, Jones, Magee, & Caputi, 2013).
One key characteristic that led the researcher to choose a qualitative framework was that the researcher comes across as directive; as a result they are able to direct the participant and the flow of the conversation (Rubin & Rubin, 2012). Additionally, the researcher can ask for more clarification, elaboration and unintended questions (Shinebourne & Smith, 2009). Smith (2014) proposes that a qualitative study encourages dialogue regarding participants perspectives and their socio-cultural context as well as having an impact and importance on a particular group. For instance providing positive social change for BME individuals with mental illness.
On one hand, the interviewer had to have double attention where they formulated questions based on the spontaneous nature of answers deriving from the interview whilst bearing in mind their structured questions must be answered (Wengraf, 2011). On the other hand, with the permissions of the interviewees, the interviews were audio recorded so transcribed data were accurate. However, the transcription process was time consuming (Byrman 2001). Furthermore, conclusions from qualitative interviews are not generalizable in the way quantitative results are to the population (Edwards & Holland, 2013); this highlights some drawbacks of using qualitative research such as semi-structured interviews.
Participants
Through social media and word of mouth, purposive sampling was used to recruit six participants. The inclusion criteria comprised of three males and three females; three of afro-Caribbean descent and three from Asian and Arabic origin, all between the ages of twenty-one and twenty-six. Purposive sampling ensured the competence of the interview was based on reliability and reflexivity (Alvesson & Skoldberg, 2009; Tongco, 2007). Significance was placed on interviewing ethnic minorities; in turn, this enabled the researcher in gathering a holistic rich analysis and detailed account of extracts from the semi-structured interviews (Ritchie 2014). Pseudonyms were used to ensure confidentiality and anonymity (Burns and Grove, 2005; Polit and Beck 2006).
Materials
An interview guide was developed based on previous research in order to guide the interviewer (Memon et al., 2016; Shefer et al., 2013). Six main themes were constructed where the interview guide consisted of broad questions intending to generate flexible discussions on the attitudes and perceptions of mental health (DiCicco-Bloom, 2009).
These themes were: social problems (“Have you ever been bullied or know someone who has been bullied?”), academic issues (“Throughout your education life, have you struggled to deal with exam and assignment deadlines? In what way?“), financial difficulties (“Do you feel you get a lack of support from well-being services at work?”), religious influence (“What are some of the beliefs your religion speaks about in regards to mental and emotional issues someone faces?”), culture impact (“Do you feel your parents and country of origin’s culture has influenced you?”)and mental health stigma (“Do you feel people do not care what BME people say in regards to their emotions?“). In its respective order, directed questions were constructed to elicit specific responses and a deeper understanding of BME group’s feelings to mental health; it was ensured to ease the participants gradually into the main topic of discussion so rapport could be built between researcher and participant (Braun & Clarke, 2006).
Pilot Study
Two pilot interviews were conducted to test the interview guide and revise as necessary (Pietkiewicz & Smith, 2014). There was an icebreaker for the first few questions to obtain the most reliable and desired results from the respondent; probes were also used to prompt answers and allow the conversation to run naturally (DiccBloom & Crabtree, 2006; Cresswell, 2008). Results suggested there were weaknesses such as long-winded and ambiguous questions in the interview guide. Most importantly, new research questions were added, as data the interviewer wanted to find out was not being spoken of. As a result, unrelated questions were removed and other questions were amended to encourage descriptive responses.
Procedure
The six participants were collected via social media (Whatsapp) once the ethics application was approved from the Division of Psychology committee in Birmingham City University (BCU). One week prior to the interview, participants were emailed a kindly reminder of the interview date, time and location as well as how the day’s event will be carried out and if they still would like to participate. This was repeated the day before the interview. Approximately 30-45 minutes was the estimated duration of the interviews. Interviewees were verbally reiterated their rights to leave at any time and were not obliged to continue conversations that were delicate and sensitive to them; a consent form (Appendix B) was then signed.
For each participant, a booked room, time and date was organized at BCU to commence accordingly. As a result, the researcher was able to ensure the participant was kept safe and confortable; this enhanced the level of data gained (Watson, 2011). Every interviewee was initially given an information sheet (Appendix C) explaining the goals of the study and rationale behind their participation; opportunities to ask any questions or display any misunderstandings were given. After all questions were answered consent forms were signed where interviewees agreed to be audio recorded with a Dictaphone during a semi-structured interview. After the interview, a debrief (Appendix D) was given.
Ethical Considerations
Before data collection, the research received official approval from the Division of Psychology committee at BCU (Appendix E) to ensure protection for both participant and researcher. For the BPS code of conduct to be adhered to and prevent any violation of confidentiality, participant’s rights were verbally reiterated: if emotionally affected, a break or end to the interview was allowed. Any identifying information that arose such as names were changed to pseudonyms or omitted from transcriptions.No physical risk occurred, as interviews took place in quiet and private room within the university; they were protected from any hindrance and distractions. After the interview, participants were signposted to well-being services this information was offered in case any possible emotional affects that may have occurred from topics raised during interview guide. Individuals were signposted to relevant well-being services as part of the debrief, and also emailed to each participant.
Data Analysis
The interviews (Appendix F) were fully transcribed and analysed based on Braun & Clarke (2006) 6-stage model of thematic analysis due to its flexibility and accessible nature. A verbatim transcription approach was adapted from Tilley & Powick (2002) in order to transcribe the interview data. This was the most effective methodical approach when extracting data from interviews, so the interviewer was able to record examined themes found from the data in a ‘bottom-up’ way (Galvin, Suomimen, Morgan, O’Connel & Smith, 2015; Guest, 2011). Braun & Clarke (2006) thematic analysis involves the process of coding in six phases to construct significant patterns. Firstly, the researcher transcribed their data collection and fully immersed into the data using verbatim by reading the transcripts a dozen times. The next stage involved taking notes of items of potential interests and familiarising themselves with possible themes. The researcher then generated initial codes and collated them from entire data set into common themes. After this, the author then reviewed the themes and developed a thematic map; this is where the provisional themes, subthemes and relationships were found (Table 1.0). Finally, the data found were divided into themes based on quoted transcripts; relevant materials were extracted from the data by hand producing more accurate analysis (Chappell, 2006).
Reflexivity
The researcher was regularly in a process of reflexivity; deliberately thinking of causes, beliefs and assumptions found within the data. In turn, the researcher was honest as possible with their rationale behind their findings and personal thoughts (D’Cruz, Gillingham, & Melendez, 2007; Ibrahim & Edgley, 2015). As a result, adopting reflexivity in this qualitative study helped the researcher in their understanding of the expectations regarding the phenomena being studied (Shaw, 2010). The researcher kept field notes during the interview about the interactions with the interviewee that guided the interview and listened to the recordings and familiarised themself with the transcripts assisted in applying interpersonal reflexivity (researcher-participant interactions that in turn involve conversation between interviewer and interviewee) (Walsh, 2003).
Results Analysis
As mentioned above, Braun & Clarke (2006) 6-stage model of Thematic Analysis was the chosen method of data analysis. The researcher’s task was to identify a sufficient number of themes from six transcripts that reflected literature on mental health stigma within the BME community. In order to be familiarised with the in-depth data (transcribed interviews), the researcher fully immersed themself into the data via repetitively reading the transcripts. Where any thoughts and patterns kept occurring and catching the researchers attention, codes were generated throughout which would eventually lead to finalised themes. The coding’s were constructed as a result of what the researcher felt as relevant and significant to the topic of BME’s views on mental health stigma. Coding each line enabled the researcher to examine every detail instead of looking at the data holistically. This was conducted in an iterative manner whereby as new themes emerged, the transcripts were re-examined via generating a thematic map and table. Consequentially, finalised themes will be defined in detail below where supporting and refuting statements (excerpts) will be put together.
In table 1.0 below, the first theme aims to outline some of the reasons behind the BME’s lack of understanding and knowledge about mental health issues. The second theme discusses the discrimination targeted at BME people with mental illness from their own community. The third theme seeks to understand why BME do not communicate about mental health issues within the family. The fourth and final themes aim to find out what’s preventing BME accessing mental health services and what ways to increase access within the BME community. Instead of being presented distinctly, the views and perceptions of six BME individuals were collated and presented under each theme in the following sections:
Table 1.0: Breakdown of Themes and Sub-themes
| Themes | Sub-themes |
|
|
|
|
|
|
|
|
|
|
|
|
Theme 1: No Such Thing As Mental Health In The BME Culture
This theme seeks to identify how the BME community perceive mental health and illness through religion and cultural beliefs. According to findings, there is a lack of thorough awareness about mental health within the BME community. Rather, some participants cited supernatural and religious causes behind mental illness; the fear of being mentally ill due to witchcraft and being possessed is what drives stigmatising attitudes towards each other. This results in BME’s humiliating individuals who are mentally ill:
OP: “… I think in my religion well its frowned upon. Its almost like you’re an outcast, a witch or you got this spiritual something going on… its almost like if you’re mentally ill we wanna cast the demons out.”
The excerpt above demonstrates how someone struggling with mental health issues is looked at within some Christian denominations. This insinuates that something is wrong with the individual since they are not considered to be of a normal healthy state of mind (Thomas et al., 2016).
This is a complete contrast to biomedical scientists, psychiatrists and psychologists that understand mental health issues as abnormalities within the brain or long-term negative emotional issues:
SC: “…maybe what the scientific world would see as probably a seizure or something like that but for us who believe in evil spirits we might think that its an evil spirit whose kind of possessing the person”
The excerpt above highlights the significance religious practicing BME groups place on mental illness. Regardless of health expertise and sound evidence, BME individuals would support the claim that evil and supernatural possessions are what have caused a person to behave abnormally (Islam, Rabiee & Singh, 2015).
Through analysing the data, it has been observed that BME groups are uneducated when it comes to symptoms and diagnosis of mental illnesses (Memon et al., 2016). A lack of knowledge and understanding was perceived to be major factor in misconceptions made about mental health within BME communities:
PS: “… they are not… really educated in terms of what schizophrenia might be what parkinsons might be what dementia is… they don’t wanna be shamed or frowned upon you know…if they are diagnosed as mentally ill it might go around in the family, they maybe be segregated they maybe treated different…”
The extract above shows stigmatising views are a result of the BME’s way of thinking and upbringing; this then leads on to conflict within the family and breaks down established bonds because of the habitual denouncement of mental illness (Corrigan & Larsson, 2008).
A domino effect is thus created where people from BME backgrounds neglect conversations about mental health; mental illness is non existent within their culture and therefore there is no comprehension that people can face mental health issues:
MB: “… there’s this idea that black people have to look strong you have to look ermm like you can handle things so if we are struggling we don’t talk about it that’s the problem we don’t talk about whats going on and theres a culture in the black community not to talk about difficult times we just wanna look strong…”
This suggests that when BME individuals have a mental breakdown, they deal with issues on their own and place their problems behind the impression of being strong. This is because of their lack of awareness regarding support for mental health problems they face. BME individuals learn to accept problems as they are; in effect this makes them resilient when facing issues.
This is emphasised in the data as BME people who immigrate to the UK predominantly come from low economically developed countries (LEDC) and experience different childhoods; people from these backgrounds tend to form coping mechanisms as a result of hardships:
OP: “…they’re just diagnosing people so frequently be it mentally ill like someone might just be doing some sort of behaviour and you guys come and diagnose them as mentally ill so to my mum it was completely absurd…”
The excerpt above suggests BME people do not experience education or health promotion regarding mental health in their native countries as frequently as people from the UK. As a result, they are more hesitant to wanting to be well informed about mental illness and thus form ignorant statements. Ultimately, mental health is seen as an unacceptable topic of discussion (Memon et al., 2016).
Theme 2: In-Group Discrimination And Cultural Naivety
After examining the data, it was found that mental illness is seen so negatively in the BME community that it leads to shaming and isolation within social circles. There are perceived views within BME groups about not speaking about mental illness, however when an individual struggling does speak out:
OP: “… they will make you feel very uncomfortable, very very uncomfortable. They do not accept mental illness, they, its not something common out there especially in my community… Hundred percent. They would always look at them a certain way…”
The excerpt above suggests that BME’s attitude towards mental illness is a result of fear of losing the respect of others and standing within the community (Karim et al., 2004). Consequently, judgmental and ill-advised statements about someone struggling with mental health are created:
KB “… its like your mad you’re probably someone whose to them you’ve probably taken drugs you’ve probably you know had a history of crack to be jumping like that and having these hallucinations you’re either just a big sinner or this is Gods way of punishing you…”
Judgmental perceptions such as above are a common theme within BME communities; religious condemnations are believed to be a result of individual’s previous actions (Shefer et al., 2013).
Therefore stigma attributed to mental health is seen as a person’s own downfall and poor decision-making:
AM: “… there is a lack of understanding of mental illness in my community and things like schizophrenia are often looked at as if the person is crazy or possessed or much like the way some people believe in witchcraft…”
This suggests that there is a correlation in BME mental health sufferers between being perceived as mad, punished by God and possessed by a supernatural power.
Critical of mental illness, disapproving BME groups then lead onto separating themselves from mental health sufferers:
PS: “… if someone from our native country was to be suffering from a certain illness or mental health problem, they’d be kinda alienated and sectioned off…”
The extract above suggests that avoidant behvaiour is used within the community as a response of the public stigma attributed towards mental health sufferers and the social repercussions affecting the individual and family (Thornicroft, Rose, Kassam & Sartorius, 2007).
Theme 3: Lack Of Support From Family And Friends
From analysing the transcripts, a contributing factor to the deterioration of mental illness within BME individuals is the lack of support from families and friends within the BME population. The inability to speak to someone close to home and who knows you well is a warning that there are inadequate levels in the early onset diagnosis of mental disorders:
MB: “With family its all about communication no one talks, no one talks about difficult times its like talking about finding things hard is so alien in the black community…”
The excerpt above emphasises how difficult it is for BME individuals struggling with mental illness to talk about their problems; BME’s are therefore less willing to speak out due to judgements of both the family and BME community (Kjellin & Östman, 2005).
This is reinforced by cultural beliefs developed within BME groups where family members condescendingly play down mental health problems, especially if they are young:
KB: “… The words stress in a young person doesn’t come into her head she doesn’t understand she just literally like giggled and looked at me as if as I’m ridiculous its like stressed how are you stressed you’re young what do you even mean about stressed…”
The abstract above suggests that stigmatising responses by family members can have a demoralising affect on mental health sufferers; in turn BME individuals are likely to hide their problems away in order to not be ridiculed by their family (Drapalski et al., 2013).
However, the data found refuting claims within this theme; people from an Arabic background would show a level of sympathy towards someone suffering from mental illness:
AM: “… I think normally what they’d tend to do would be they feel sorry for the person… and obviously pray for them… and spiritual healing…”
This excerpt suggests that despite a lack of understanding of mental illness, religious BME individuals would consider the feelings and emotional pain a mental health sufferer is going through and show compassion through spiritual prayers.
Interestingly, this was found again within the analysed transcripts; BME Christians always felt compelled to help an individual from their community who is suffering from emotional distress:
OP: “… if someone is going through something mentally they are so ready to be like whats going on, whats happening inside of you. We want to make sure that spiritually, physically or mentally you are okay.”
The two refuting extracts above indicate that religious practicing BME groups aim to provide support to people with mental illness. This implies that some BME individuals take mental illness serious within their families and try to mitigate the severe effects.
Theme 4: Barriers To Seeking Help
A significant part of the data comprised of the negative experiences of BME individuals within health services and difficulties that prevent them from accessing necessary treatments. Participants cited institutional racism as one major factor:
AM: “… I don’t believe BME people are given the same kind of pedestal as (.) white people…its just I’ve noticed a lot more judgment and criticism of black people when committing crimes especially with mentally ill black people…”
The excerpt above suggests that BME people are not receptive to what health professionals say or even attempt to seek advice due to the level of racism attributed towards them by the police force; this deters individuals, as there is a perceived belief that they are liable to being mistreated in mental health services (Duffin 2008).
Other participants also pointed out that there is mistrust between themselves and service clinicians and as a result this could delay BME people seeking help:
OP: “…the therapists, the psychologists we cant trust them because like if we cant trust police people who are out there to help us and keep us safe, we wont trust somebody who they feel they just gonna diagnose us…”
The above extracts demonstrate that the BME population feel unsafe with health professionals; they have not received an adequate level of treatment or clinician support from civil servants such as general practitioners and police officers. As a response, they avoid contact and deal with possible mental health issues alone and within the family (Knifton et al., 2009).
The level of oppression and racism towards the BME is seen as a generational problem; it is ingrained in the children of BME adults to not seek help from services because of this:
SC: “… I think this stems from historical times where minorities have been oppressed… there’s still definitely racism still exists…”
KB: “…. I feel like if we do especially if we mention the word race we’re being told we’re throwing the race card. I don’t feel like people are taking that much into consideration because they don’t understand us. Health professionals too don’t understand us and our race…”
The two excerpts atop indicate that health clinicians are incompetent at the level of service given to BME individuals; due to a lack of understanding of BME’s culture and the recurrence to neglect the oppression of BME groups still face. This eventually results in mental health sufferers not getting any support (Islam, Raibee & Singh, 2015).
The data also found that Language and costly interventions were a deterrent for BME people accessing mental health institutions:
AM: “… it’s the language barrier where it comes down to…”
MB: “… I understand the implications of that as its very expensive and time consuming….”
All in all, BME individuals may be put off accessing treatments as a result of a lack of fluent English and economic difficulties (Dardas & Simmons, 2015). This then leaves BME mental health sufferer’s conditions to worsen due to the added pressures of dealing with in-group discrimination.
Theme 5: Increasing BME Access To Mental Health Services
From the data, there was a common consensus that there needs to be raised awareness and education in mental health and illness due to BME’s lack of knowledge of mental disorders:
SC: “… early education will be really important, maybe the government could do something to create more awareness about all the mental health issues…”
OP: “… there needs to be awareness of mental illness, campaigns ermm broadcasts. It needs to be put out there that mental illness is not just someone going crazy…”
The excerpts above suggests that nationally, attempts and considerable effort needs to be made by governments and public health institutions; this way the BME population are fully aware of the symptoms mental health conditions bring and how to respond to certain triggers (Memon et al., 2016; Knifton, 2012).
This was echoed by other participants where they felt mental health education is rather limited and ineffective within the BME community. One way to rectify this through targeting BME audiences via the media:
PS: “… TV channels that we have, maybe there could be some advertising on there or something, they can have a guess speaker, that works alongside the NHS and mental health, ermm to give out advice in terms of how these people could reach out to accessing these mental health services…”
The above extract indicates that a lot of the perceived stigmas attributed to mental health strugglers stems from negative experiences in healthcare; essentially, if BME’s are unwilling to seek help, information from professionals can be provided without having to fear of being discriminated (Hnederson et al., 2014). In turn, BME groups are being taught about the mechanisms behind mental illness and consequences if neglected and untreated.
In contrast, other participants mentioned that there should be wider community based interventions where there are support groups catered specifically for the BME community; this way, people will not feel deterred in seeking help from health experts regardless of race and ethnicity:
MB: “There should be more positive black groups I think, I think there are a lot of black groups that are about I dunno self acceptance and black empowerment and I don’t think that does any good and I think it reinforces our pain and reinforces our history …”
This strengthens the claim that mental health stigma is sometimes rooted in the history of oppression in BME groups. In order to combat this, installing community support groups that encourage helping one another regardless of ethnicity and limiting the stance of BME’s against Caucasian people will help improve access to mental health services (Bhui et al, 2015; Rehman & Owen, 2013).
After examining the data, it was discovered again that community based groups where the BME work in tangent together is an efficacious way in improving access to mental health services:
AM: “… there should be kind of a leader within the Arabic community and the same for black communities Asian communities who kinda takes the overall responsibility of (.) creating community centres…. These users can interact with their own people and that way it can be flagged up as well if people are brought together you cans tart to see the cracks in their personal lives…”
This extract above indicates that BME individuals are able to recognise mental health symptoms much more rapidly within a BME led community support group system; this could result in higher rates of admission in primary mental health services and a reduction in BME individuals with mental illness being sectioned or admitted to mental hospitals due severe psychosis issues.
Similarly, it was found that BME people that have been through stigmatisation but also effective treatments could help encourage BME communities to access mental health services:
KB: “… so I think we need role models. Black or whatever ethnic minority role models that have suffered who have recovered or who can share their experiences one to one…”
OP: “… so having people like us, look like us, talk like us, have the same experiences like us come out and speak about how services have helped them and improved their health”
These excerpts merely highlight that BME groups are much more susceptible to accessing services by listening to someone who has successfully recovered from a mental illness as they can relate and understand their cultural background.
According to findings, due to variations in cultural backgrounds, BME individuals perceived majority of treatments as tailored to Caucasian people:
SC: “… a lot of it is adapted to the western world so maybe the interventions need to be culturally adapted and the person who is giving this intervention should also be trained on how they should approach the minorities…”
The quote above suggests that BME’s view clinicians as culturally incompetent; this may delay treatment to BME mental health sufferers, as health specialists are not trained on how to be culturally sensitive to BME individuals.
Equally, the data found therapy based interventions lead by BME individuals as the most effective treatment:
PS: “… because that way they can build rapport easier, there would be no biasedness ermmm the person will feel more carmer…”
Findings from previous themes suggest that BME’s are hesitant in accessing and speaking about mental health issues; the extract above suggests that this can be eradicated if therapists are from the same ethnic groups as BME groups (Sue et al., 2009).
Additional to cultural adapted interventions, it was found that integrating spiritual and religious needs to devout BME mental heath sufferers was fundamental in forming effective treatments:
AM: “… religion is a big part for a lot of these BME cultures, theres Christianity, Hinduism, Islam so incorporating faith in the therapies is quite essential…”
The above extract implies that clinicians have a lack of knowledge and understanding regarding BME individuals spiritual needs and as a result, therapies and drug therapy used with BME clients need to be religious sensitive and ensure that their faiths are not compromised (Islam, Raibee & Singh, 2015).
Discussion
The results found are consistent with previous qualitative research that focused on mental health stigma, within the BME population; this was expected as a proportional amount of the interview guide was based on previous literature from Memon et al., 2016; Shefer et al., (2013). The first research aim was to identify BME group’s experiences and perception regarding stigma attached to mental health. Findings from this study indicated that BME’s expressed a high level of negative and ignorant attitudes towards people with mental illness due to three main factors: supernatural or religious beliefs, poor education in mental health, and social discrimination. Likewise, this was found in previous studies, where lack of knowledge of mental illness, the incapability of recognising symptoms of psychological disorders, and social shaming leads to mental health stigma (Islam & Campbell, 2015; Knifton, 2012; Memon et al., 2016; Shefer et al., 2013). The second research aim was also met where BME individuals mentioned the family being fearful of public stigma, prejudicial profiling from health clinicians, and mistrust of doctors for not accessing mental health services enough (Halbert, Armstrong, Gandy & Shaker, 2006; Kovandžić, et al.,, 2011; Pole, Gone, & Kulkarni, 2008). Although, one of the participants argued that views of BME groups against white people should be combated (Adegbembo, Tomar & Logan, 2006); this may reduce the perceived view that all clinicians are or have always prejudiced them. Finally, the last aim sought effective solutions to improving access to mental health services; community based anti-stigma interventions, therapies that comprised of BME clinicians and integrating religious and cultural beliefs in interventions were proposed by the participants (Islam, Raibee & Singh, 2015; Knifton, 2012; Sue et al., 2009).
In summary, the analysis found, reinforce that BME’s have limited awareness in the symptoms and treatments of mental illnesses. Subsequently, ethnic minorities predominantly use religious and cultural beliefs to demonstrate the severity of mental illness. The resulting effect leaves BME people who suffer from mental illness also having to deal with discriminative attitudes and behaviours from their own community. Due to such derogative behaviours, families and friends feel inclined to reinforce these beliefs, so they do not receive negative treatment from their social circles and lose the respect of others within the BME community. This merely suppresses the emotions and feelings of BME mental health sufferers; they cannot speak up about their issues to their families out of fear of social repercussions left on themselves and close ones. As a result, a false impersonation of being strong and being able to handle their issues is developed. However, it was discovered that religious practicing BME’s often show characteristics of compassion and concern for people with mental illness. This implies that there are religious and cultural differences in the way BME’s in the community approach mental health issues.
In addition to this, ethnic minority groups cited receiving poor experiences from professionals in public services contributing to high levels of mistrust. The mistrust from health professionals suggested there was a lack of effective therapeutic relationships due to the unwillingness of clinicians in understanding BME cultures and tailoring treatments towards them. In order to encourage more BME individuals to access mental health services, it was proposed that there should be implemented community based campaigns and interventions to help generate awareness and understanding of the causes and possible treatments for mental health problems. Culturally adapted interventions where clinicians are also from BME cultures and incorporating religious leaders to help meet devout BME’s spiritual and faith needs were also encouraged. Recent literature has cited this as more effective as increased user esteem and greater trust would be put in therapeutic interventions and clinicians (Crawford, 2002; Henderson et al., 2004).
Strengths
The participants comprised of two Christians, two Muslims, one Sikh and an atheist; in contrast to previous studies, this research puts significance on religious practicing people within the BME population. Despite differences in religious backgrounds, throughout most themes, there was constant similarities in the experiences and perceived views of mental health, especially within shaming BME’s with mental illness and losing standing in the community. On one hand, Christian, Muslim, and Sikh BME groups were more likely to show sympathy and concern with someone from the BME struggling with mental illness. On the other hand, they would cite supernatural and religious causes as the root of mental illness and thus shame the individual that is in need of help. This indicates that the less knowledge religious BME individuals know of mental health disorders, the more stigmatising and less empathetic they are to mental health sufferers. In addition, using semi-structured interviews enabled the interviewer to obtain as much information from deep-rooted personal accounts whilst easing the interviewee into discussion; mental health is a sensitive topic, especially for BME individuals so developing rapport was essential in gaining subjective views (Brewerton & Millward, 2001).
Limitations
The validity and reliability of this study may be seen as compromised due to some methodological limitations. First of all, the researcher attended the same university of some of the participants whereby four out of six were from the same degree. Consequently, numerous issues could of arisen; participant’s level of awareness regarding mental health could be much greater than people who do not study psychology and some participants may have taken a cautious approach when responding to questions due to conflict of interest and fear of sharing intimate details. As a result of possibilities of mutual friendship and bias, responses to questions may have been compromised to tailor results for the interviewer. Therefore, a comprehensive understanding of BME group’s perception and the stigma of mental health may not have been acquired due to researcher bias.
As mentioned above, the study comprised of university-educated participants; studies have found academically competent students to be advanced in their knowledge of mental illness compared to the BME population that are generally in manual labour jobs and in less contact with mental illness (Scottham, Sellers & Nguyen, 2008). Additionally, the study was situated in Birmingham; how BME’s perceive and react to mental illness varies when compared to different regions of the UK (Knifton et al., 2009). This study was also limited by the absence of middle and elderly aged BME groups; the age range of participants was from 18-26. Hence, it is difficult to generalise findings when the sample size consisted of these six participants to represent BME’s within Birmingham and the country as a whole. Future research should include participants on a larger scale deriving from around the country by using a longitudinal mixed design study (qualitative and quantitative between five to ten years). This will increase methodological pluralism, resulting in superior research and supported by enriched data (Edwards & Holland, 2013; Johnson & Onwugegbuzie, 2013).
Unique Contribution
There has been a considerable rise in media and political attention regarding mental health stigma in the last five years; BME groups is one of the demographics that have benefitted from this level of scrutiny. Hence, this study provides a fresh and unique look at the association between mental health stigma and increasing levels of severe mental illness. Through public discussion and debates, researchers have placed importance in understating the negative effects mental health has on society in general. As a result, future research should firstly aim to investigate new age movements and religions that can also contribute to the negative or positive perceptions of mental illness. Secondly, upcoming research in mental health stigma should be looked at in collectivist cultures and countries where stigma tends to be strong; it is not a coincidence that research and empirical evidence from these locations are lacking due to poor understanding of other cultures.
Practical Implications
Overall, the findings from this study suggest that a positive contribution can be made on a political level as well as to the NHS. The government can implement effective campaigns that are aimed at the BME community so they can be encouraged to have conversations and discussions about mental health; this may help reduce stigma and discrimination against BME’s with mental illness. Rehman and Owen, (2013) survey suggested that higher awareness and advertisements gives the very few open BME individuals with mental illness the opportunity to not feel neglected. In terms of the NHS, nurses and clinicians will be enabled to show more understanding and compassion towards BME mental health sufferers due to increased competency in cultural and religious beliefs; it is hoped that high levels in the diagnosis of mental disorders, especially severe psychosis would be reduced because of raised awareness in both clinicians and BME population, ending discrimination.
Conclusion
This study set out to understand BME’s experiences in mental health, and how developed stigma contributes to a large number of the BME population with mental illness not accessing mental health services. In turn, leaving BME mental health sufferers not receiving necessary treatment. Findings from this study identified that misconceptions in mental illness derived from a lack of education in cultures where religious or supernatural factors were seen as the root causes. The research has also shown that losing standing within community due to mental illness results in less support from friends and family; the shaming and discrimination thus deters BME individuals from seeking help.
Additionally, a lack of BME representatives in health services and experiences of institutional racism has created a barrier for BME’s in seeking help. In order to rectify this, forming community based awareness campaigns; increasing clinicians from BME backgrounds and developing culturally adapted interventions would be beneficial according to the participants. Notwithstanding the relatively limited sample and problems associated with the demographics, the study can notify other researchers investigating stigma, especially within minority groups about the issues they have to contend with so appropriate and effectual treatments can be implemented. Overall, the current findings enhance our understanding of mental health stigma within BME communities and add on to the increasing literature on stigma.
References
Adegbembo, A., Tomar, S., & Logan, H. (2006). Perception of racism explains the difference between Blacks’ and Whites’ level of healthcare trust. Ethnicity & Disease, 16(4), 792-8.
Adult Psychiatric Morbidity Survey. (2017). NATCEN Social Research. Retrieved 1 May 2017, from http://natcen.ac.uk/our-research/research/adult-psychiatric-morbidity-survey/?gclid=CPLcpsfLztMCFRAz0wodAjMG3Q
Alegría, M., Mulvaney-Day, N., Torres, M., Polo, A., Cao, Z., & Canino, G. (2007). Prevalence of Psychiatric Disorders Across Latino Subgroups in the United States. American Journal Of Public Health, 97(1), 68-75. http://dx.doi.org/10.2105/ajph.2006.087205
Alverson, H., Smith, B., Ritsema, M., Drake, R., Chu, E., & Carpenter-Song, E. (2010). Ethno-Cultural variations in the experience and meaning of mental illness and treatment: Implications for access and utilization. Transcultural Psychiatry, 47(2), 224-251. http://dx.doi.org/10.1177/1363461510368906
Bécares, L., Nazroo, J., & Wallace, S. (2016). Cumulative effect of racial discrimination on the mental health of ethnic minorities in the United Kingdom. American Journal Of Public Health, 106(7), 1294-1300. http://dx.doi.org/10.2105/ajph.2016.303121
Bee, P., Brooks, H., Fraser, C., & Lovell, K. (2015). Professional perspectives on service user and carer involvement in mental health care planning: A qualitative study. International Journal Of Nursing Studies, 52(12), 1834-1845. http://dx.doi.org/10.1016/j.ijnurstu.2015.07.008
Berger, L., Nagayama Hall, G., Zane, N., & Sue, S. (2009). The case for cultural competency in psychotherapeutic interventions. Annual Review Of Psychology, 60(1), 525-548. http://dx.doi.org/10.1146/annurev.psych.60.110707.163651
Bhui, K., Aslam, R., Palinski, A., McCabe, R., Johnson, M., & Weich, S. et al. (2015). Interventions to improve therapeutic communications between Black and minority ethnic patients and professionals in psychiatric services: systematic review. The British Journal Of Psychiatry, 207(2), 95-103. http://dx.doi.org/10.1192/bjp.bp.114.158899
BHUI, K., STANSFELD, S., HULL, S., PRIEBE, S., MOLE, F., & FEDER, G. (2003). Ethnic variations in pathways to and use of specialist mental health services in the UK: Systematic review. The British Journal Of Psychiatry, 182(2), 105-116. http://dx.doi.org/10.1192/bjp.182.2.105
Blankenship, D., & Schwartz, R. (2014). Racial disparities in psychotic disorder diagnosis: A review of empirical literature. World Journal Of Psychiatry, 4(4), 133. http://dx.doi.org/10.5498/wjp.v4.i4.133
Bodenhausen, G., Todd, A., Corrigan, P., & Rüsch, N. (2010). PW01-209 – implicit self-stigma in people with mental illness. European Psychiatry, 25, 1637. http://dx.doi.org/10.1016/s0924-9338(10)71616-3
Boyd, J., DeForge, B., Brown, C., Aakre, J., Perrin, P., Lucksted, A., & Drapalski, A. (2013). A model of internalized stigma and its effects on people with mental illness. Psychiatric Services, 64(3), 264-269. http://dx.doi.org/10.1176/appi.ps.001322012
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research In Psychology, 3(2), 77-101. http://dx.doi.org/10.1191/1478088706qp063oa
Brown, A., & Hanely, J. (2013). Cultural variations in interpretation of Postnatal illness: Jinn possession amongst Muslim communities. Community Mental Health Journal, 50(3), 348-353. http://dx.doi.org/10.1007/s10597-013-9640-4
Burns, N., & Grove, S. Study guide for the Practice of nursing research (1st ed.).
Burton, C., & Galletly, C. (2011). Improving medical student attitudes towards people with schizophrenia. Australian & New Zealand Journal Of Psychiatry, 45(6), 473-476. http://dx.doi.org/10.3109/00048674.2011.541419
Caldwell, K., Foster, J., & Papadopoulos, C. (2012). ‘Individualism-Collectivism’ as an explanatory device for mental illness stigma. Community Mental Health Journal, 49(3), 270-280. http://dx.doi.org/10.1007/s10597-012-9534-x
Campbell, J., Noel, J., Sangster, Y., Lambert, D., Thompson, V., & Corrigan, P. (2003). Perceptions of discrimination among persons with serious mental illness. Psychiatric Services, 54(8), 1105-1110. http://dx.doi.org/10.1176/appi.ps.54.8.1105
Campbell, R., & Islam, F. (2012). “Satan has afflicted me!” Jinn-Possession and mental illness in the Qur’an. Journal Of Religion And Health, 53(1), 229-243. http://dx.doi.org/10.1007/s10943-012-9626-5
Canino, G., Cao, Z., Polo, A., Torres, M., Mulvaney-Day, N., & Alegría, M. (2007). Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal Of Public Health, 97(1), 68-75. http://dx.doi.org/10.2105/ajph.2006.087205
Caputi, P., Magee, C., Jones, S., & Cridland, E. (2013). Family-focused autism spectrum disorder research: A review of the utility of family systems approaches. Autism, 18(3), 213-222. http://dx.doi.org/10.1177/1362361312472261
Cardemil, E., Nelson, T., & Keefe, K. (2015). Racial and ethnic disparities in depression treatment. Current Opinion In Psychology, 4, 37-42. http://dx.doi.org/10.1016/j.copsyc.2015.01.021
Carpenter-Song, E., Chu, E., Drake, R., Ritsema, M., Smith, B., & Alverson, H. (2010). Ethno-Cultural Variations in the Experience and Meaning of Mental Illness and Treatment: Implications for Access and Utilization. Transcultural Psychiatry, 47(2), 224-251. http://dx.doi.org/10.1177/1363461510368906
Clarke, V., & Braun, V. (2006). Using thematic analysis in psychology. Qualitative Research In Psychology, 3(2), 77-101. http://dx.doi.org/10.1191/1478088706qp063oa
Clement, S., Bhugra, D., Thornicroft, G., Hatch, S., Schauman, O., & Farrelly, S. et al. (2014). Mistrust of mental health services: Ethnicity, hospital admission and unfair treatment. Epidemiology And Psychiatric Sciences, 24(03), 258-265. http://dx.doi.org/10.1017/s2045796014000158
Cook, B., McGuire, T., & Miranda, J. (2007). Measuring Trends in Mental Health Care Disparities, 2000–2004. Psychiatric Services, 58(12), 1533-1540. http://dx.doi.org/10.1176/ps.2007.58.12.1533
Corrigan, P., & Larson, J. (2008). The stigma of families with mental illness. Academic Psychiatry, 32(2), 87-91. http://dx.doi.org/10.1176/appi.ap.32.2.87
Corrigan, P., & Watson, A. (2002). Understanding the impact of stigma on people with mental illness. World Psychiatry, 1(1), 16-20.
Corrigan, P., Angermeyer, M., & Rüsch, N. (2005). Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry, 20(8), 529-539. http://dx.doi.org/10.1016/j.eurpsy.2005.04.004
Corrigan, P., Lurie, B., Goldman, H., Slopen, N., Medasani, K., & Phelan, S. (2005). How Adolescents Perceive the Stigma of Mental Illness and Alcohol Abuse. Psychiatric Services, 56(5), 544-550. http://dx.doi.org/10.1176/appi.ps.56.5.544
Corrigan, P., Morris, S., Michaels, P., Rafacz, J., & Rüsch, N. (2012). Challenging the Public Stigma of Mental Illness: A Meta-Analysis of Outcome Studies. Psychiatric Services, 63(10), 963-973. http://dx.doi.org/10.1176/appi.ps.201100529
Corrigan, P., Schmidt, A., Bink, A., Nieweglowski, K., Al-Khouja, M., Qin, S., & Discont, S. (2016). Changing public stigma with continuum beliefs. Journal Of Mental Health, 1-8. http://dx.doi.org/10.1080/09638237.2016.1207224
Corrigan, P., Thompson, V., Lambert, D., Sangster, Y., Noel, J., & Campbell, J. (2003). Perceptions of Discrimination Among Persons With Serious Mental Illness. Psychiatric Services, 54(8), 1105-1110. http://dx.doi.org/10.1176/appi.ps.54.8.1105
Coulter, A., Entwistle, V., Eccles, A., Ryan, S., Shepperd, S., & Perera, R. (2015). Personalised care planning for adults with chronic or long-term health conditions. Cochrane Database Of Systematic Reviews. http://dx.doi.org/10.1002/14651858.cd010523.pub2
Crabtree, B., & DiCicco-Bloom, B. (2006). The qualitative research interview. Medical Education, 40(4), 314-321. http://dx.doi.org/10.1111/j.1365-2929.2006.02418.x
Crawford, M. (2002). Systematic review of involving patients in the planning and development of health care. BMJ, 325(7375), 1263-1263. http://dx.doi.org/10.1136/bmj.325.7375.1263
Creswell, J. (2008). Research design: Qualitative, quantitative, and mixed methods approaches (3rd ed.). Thousand Oaks, CA: Sage Publications.
Cridland, E., Jones, S., Caputi, P., & Magee, C. (2014). Qualitative research with families living with autism spectrum disorder: Recommendations for conducting semistructured interviews. Journal Of Intellectual And Developmental Disability, 40(1), 78-91. http://dx.doi.org/10.3109/13668250.2014.964191
CRISP, A., Gelder, Rix, Meltzer, & Roawlands. (2000). Stigmatisation of people with mental illnesses. The British Journal Of Psychiatry, 177(1), 4-7. http://dx.doi.org/10.1192/bjp.177.1.4
Dalakar, J., & Procter. (2003). Poverty in the United States 2002 (poverty in the United States). United States Government Printing.
Dardas, L., & Simmons, L. (2015). The stigma of mental illness in Arab families: a concept analysis. Journal Of Psychiatric And Mental Health Nursing, 22(9), 668-679. http://dx.doi.org/10.1111/jpm.12237
D’Cruz, H., Gillingham, P., & Melendez, S. (2005). Reflexivity, its Meanings and Relevance for Social Work: A Critical Review of the Literature. British Journal Of Social Work, 37(1), 73-90. http://dx.doi.org/10.1093/bjsw/bcl001
de Freitas, C. (2013). Aiming for inclusion: A case study of motivations for involvement in mental health-care governance by ethnic minority users. Health Expectations, 18(5), 1093-1104. http://dx.doi.org/10.1111/hex.12082
de Jong, J., Reis, R., Jordans, M., Sivayokan, S., Vallipuram, A., Tol, W., & Thomas, F. (2016). Emic perspectives on the impact of armed conflict on children’s mental health and psychosocial well-being: Applying a social ecological framework of resilience in northern Sri Lanka. Peace And Conflict: Journal Of Peace Psychology, 22(3), 246-253. http://dx.doi.org/10.1037/pac0000172
de Visser, R., Scanlon, T., Cooper, M., Sundin, J., Mohebati, L., Taylor, K., & Memon, A. (2016). Perceived barriers to accessing mental health services among black and minority ethnic (BME) communities: A qualitative study in southeast England. BMJ Open, 6(11), e012337. http://dx.doi.org/10.1136/bmjopen-2016-012337
de Wit, M., Tuinebreijer, W., van Brussel, G., & Selten, J. (2010). Ethnic differences in risk of acute compulsory admission in Amsterdam, 1996–2005. Social Psychiatry And Psychiatric Epidemiology, 47(1), 111-118. http://dx.doi.org/10.1007/s00127-010-0312-1
Denzel, A., van Esch, A., Harte, J., & Scherder, E. (2016). Ethnic variations in psychotic disorders in the criminal justice system: A systematic review. Aggression And Violent Behavior, 29, 20-29. http://dx.doi.org/10.1016/j.avb.2016.05.006
Diana J. Burgess, Yingmei Ding, Margaret Hargreaves, Michelle van Ryn, & Sean Phelan. (2008). The Association between Perceived Discrimination and Underutilization of Needed Medical and Mental Health Care in a Multi-Ethnic Community Sample. Journal Of Health Care For The Poor And Underserved, 19(3), 894-911. http://dx.doi.org/10.1353/hpu.0.0063
DiCicco-Bloom, B., & Crabtree, B. (2006). The qualitative research interview. Medical Education, 40(4), 314-321. http://dx.doi.org/10.1111/j.1365-2929.2006.02418.x
Dinos, S. (2004). Stigma: The feelings and experiences of 46 people with mental illness: Qualitative study. The British Journal Of Psychiatry, 184(2), 176-181. http://dx.doi.org/10.1192/bjp.184.2.176
Donner, B., Mutter, R., & Scior, K. (2010). Mainstream In-Patient Mental Health Care for People with Intellectual Disabilities: Service User, Carer and Provider Experiences. Journal Of Applied Research In Intellectual Disabilities, 23(3), 214-225. http://dx.doi.org/10.1111/j.1468-3148.2009.00527.x
Dowrick, C., Gask, L., Aseem, S., Edge, D., Peters, S., & Edwards, S. et al. (2011). Access to primary mental health care for hard-to-reach groups: From ‘silent suffering’ to ‘making it work’. Social Science & Medicine, 72(5), 763-772. http://dx.doi.org/10.1016/j.socscimed.2010.11.027
Drapalski, A., Lucksted, A., Perrin, P., Aakre, J., Brown, C., DeForge, B., & Boyd, J. (2013). A Model of Internalized Stigma and Its Effects on People With Mental Illness. Psychiatric Services, 64(3), 264-269. http://dx.doi.org/10.1176/appi.ps.001322012
Duffin, C. (2008). Talk it through. Nursing Standard, 23(5), 22-23. http://dx.doi.org/10.7748/ns.23.5.22.s26
Duval, S., Jarvis, P., Msc, C., Ba, M., & Saltus, R. (2013). Count me in published version Aug 2013. Retrieved from https://www.diversecymru.org.uk/wp-content/uploads/Count-Me-In_published-version-Aug-2013.pdf
Ennis, L., & Wykes, T. (2013). Impact of patient involvement in mental health research: longitudinal study. The British Journal Of Psychiatry, 203(5), 381-386. http://dx.doi.org/10.1192/bjp.bp.112.119818
Esquilin, M., Nadal, K., Holder, A., Bucceri, J., Torino, G., Capodilupo, C., & Sue, D. (2007). Racial microaggressions in everyday life: Implications for clinical practice. American Psychologist, 62(4), 271-286. http://dx.doi.org/10.1037/0003-066x.62.4.271
Evandrou, M., Falkingham, J., Feng, Z., & Vlachantoni, A. (2016). Ethnic inequalities in limiting health and self-reported health in later life revisited. Journal Of Epidemiology And Community Health, 70(7), 653-662. http://dx.doi.org/10.1136/jech-2015-206074
Evans-Lacko, S., Henderson, C., Thornicroft, G., Nellums, L., Rose, D., & Shefer, G. (2012). ‘Our community is the worst’: The influence of cultural beliefs on stigma, relationships with family and help-seeking in three ethnic communities in London. International Journal Of Social Psychiatry, 59(6), 535-544. http://dx.doi.org/10.1177/0020764012443759
FEDER, G., MOLE, F., PRIEBE, S., HULL, S., STANSFELD, S., & BHUI, K. (2003). Ethnic variations in pathways to and use of specialist mental health services in the UK: Systematic review. The British Journal Of Psychiatry, 182(2), 105-116. http://dx.doi.org/10.1192/bjp.182.2.105
Galletly, C., & Burton, C. (2011). Improving Medical Student Attitudes Towards People with Schizophrenia. Australian & New Zealand Journal Of Psychiatry, 45(6), 473-476. http://dx.doi.org/10.3109/00048674.2011.541419
Galvin, J., Suominen, E., Morgan, C., O’Connell, E., & Smith, A. (2015). Mental health nursing students’ experiences of stress during training: a thematic analysis of qualitative interviews. Journal Of Psychiatric And Mental Health Nursing, 22(10), 773-783. http://dx.doi.org/10.1111/jpm.12273
Goffman, E. (1963). Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, N.J., Prentice Hall.
Gone, J., & Trimble, J. (2012). American Indian and Alaska Native Mental Health: Diverse Perspectives on Enduring Disparities. Annual Review Of Clinical Psychology, 8(1), 131-160. http://dx.doi.org/10.1146/annurev-clinpsy-032511-143127
Gray, A. (2002). Stigma in psychiatry. JRSM, 95(2), 72-76. http://dx.doi.org/10.1258/jrsm.95.2.72
Gulliver, P., Peck, E., & Towell, D. (2002). Evaluation of the Integration of Health and Social Services in Somerset: Part I — Final Results. Journal Of Integrated Care, 10(2), 32-37. http://dx.doi.org/10.1108/14769018200200018
Halbert, C., Armstrong, K., Gandy, O., & Shaker, L. (2006). Racial Differences in Trust in Health Care Providers. Archives Of Internal Medicine, 166(8), 896. http://dx.doi.org/10.1001/archinte.166.8.896
Hanely, J., & Brown, A. (2013). Cultural Variations in Interpretation of Postnatal Illness: Jinn Possession Amongst Muslim Communities. Community Mental Health Journal, 50(3), 348-353. http://dx.doi.org/10.1007/s10597-013-9640-4
Harding, S., & Balarajan, R. (2000). Limiting Long-term Illness Among Black Caribbeans, Black Africans, Indians, Pakistanis, Bangladeshis and Chinese Born in the UK. Ethnicity & Health, 5(1), 41-46. http://dx.doi.org/10.1080/13557850050007338
Harris, K., Edlund, M., & Larson, S. (2005). Racial and Ethnic Differences in the Mental Health Problems and Use of Mental Health Care. Medical Care, 43(8), 775-784. http://dx.doi.org/10.1097/01.mlr.0000170405.66264.23
HARRISON, J., PETRUCKEVITCH, A., REEVES, R., COOK, A., SCOBIE, S., & HAWE, E. et al. (2007). Ethnic variations in the experiences of mental health service users in England: Results of a national patient survey programme. The British Journal Of Psychiatry, 191(4), 304-312. http://dx.doi.org/10.1192/bjp.bp.106.032417
Hatch, S., Gazard, B., Williams, D., Frissa, S., Goodwin, L., & Hotopf, M. (2016). Discrimination and common mental disorder among migrant and ethnic groups: findings from a South East London Community sample. Social Psychiatry And Psychiatric Epidemiology, 51(5), 689-701. http://dx.doi.org/10.1007/s00127-016-1191-x
Henderson, C., O’Reilly, C., Shidhaye, R., Koschorke, M., Rose, D., & Doherty, M. et al. (2015). Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet. http://dx.doi.org/10.1016/s0140-6736(15)00298-6
Henderson, R., Williams, P., Gabbidon, J., Farrelly, S., Schauman, O., & Hatch, S. et al. (2014). Mistrust of mental health services: ethnicity, hospital admission and unfair treatment. Epidemiology And Psychiatric Sciences, 24(03), 258-265. http://dx.doi.org/10.1017/s2045796014000158
Hibbard, J., & Greene, J. (2013). What The Evidence Shows About Patient Activation: Better Health Outcomes And Care Experiences; Fewer Data On Costs. Health Affairs, 32(2), 207-214. http://dx.doi.org/10.1377/hlthaff.2012.1061
Hoek, H., Mackenbach, J., Laan, W., Susser, E., Selten, J., & Veling, W. (2007). Discrimination and the incidence of psychotic disorders among ethnic minorities in The Netherlands. International Journal Of Epidemiology, 36(4), 761-768. http://dx.doi.org/10.1093/ije/dym085
Holland, J., & Edwards, R. (2013). What Is Qualitative Interviewing? (1st ed.). Bloomsbury Publishing.
Hotopf, M., Goodwin, L., Frissa, S., Williams, D., Gazard, B., & Hatch, S. (2016). Discrimination and common mental disorder among migrant and ethnic groups: Findings from a south East London community sample. Social Psychiatry And Psychiatric Epidemiology, 51(5), 689-701. http://dx.doi.org/10.1007/s00127-016-1191-x
HOUSE, A., & SIMPSON, E. (2003). User and carer involvement in mental health services: From rhetoric to science. The British Journal Of Psychiatry, 183(2), 89-91. http://dx.doi.org/10.1192/bjp.183.2.89
Hunkins-Hutchison, E., Wilson, N., Quinn, N., Mirza, N., Newbigging, K., Gervais, M., & Knifton, L. (2009). Community conversation: Addressing mental health stigma with ethnic minority communities. Social Psychiatry And Psychiatric Epidemiology, 45(4), 497-504. http://dx.doi.org/10.1007/s00127-009-0095-4
Ibrahim, N., & Edgley, A. (2015). Embedding Researcher’s Reflexive Accounts within the Analysis of a Semi-Structured Qualitative Interview. The Qualitative Report, 20(10), 1671-1681. Retrieved from http://nsuworks.nova.edu/tqr/vol20/iss10/9
Islam, F., & Campbell, R. (2012). “Satan Has Afflicted Me!” Jinn-Possession and Mental Illness in the Qur’an. Journal Of Religion And Health, 53(1), 229-243. http://dx.doi.org/10.1007/s10943-012-9626-5
Islam, Z., Rabiee, F., & Singh, S. (2015). Black and Minority Ethnic Groups’ Perception and Experience of Early Intervention in Psychosis Services in the United Kingdom. Journal Of Cross-Cultural Psychology, 46(5), 737-753. http://dx.doi.org/10.1177/0022022115575737
Jamshed, S. (2014). Qualitative research method-interviewing and observation. Journal Of Basic And Clinical Pharmacy, 5(4), 87. http://dx.doi.org/10.4103/0976-0105.141942
Jenkins, R., Mubbashar, M., Rana, M., Saeed, K., & Karim, S. (2004). Pakistan mental health country profile. International Review Of Psychiatry, 16(1-2), 83-92. http://dx.doi.org/10.1080/09540260310001635131
Jennifer Alvidrez, Lonnie R. Snowden, & Dawn M. Kaiser. (2008). The Experience of Stigma among Black Mental Health Consumers. Journal Of Health Care For The Poor And Underserved, 19(3), 874-893. http://dx.doi.org/10.1353/hpu.0.0058
Jones-Berry, S. (2017). Child mental health needs ‘putting strain on services’. Nursing Standard, 31(23), 9-9. http://dx.doi.org/10.7748/ns.31.23.9.s7
JORM, A. (2000). Mental health literacy: Public knowledge and beliefs about mental disorders. The British Journal Of Psychiatry, 177(5), 396-401. http://dx.doi.org/10.1192/bjp.177.5.396
Kaiser, D., Snowden, L., & Alvidrez, J. (2008). The experience of stigma among black mental health consumers. Journal Of Health Care For The Poor And Underserved, 19(3), 874-893. http://dx.doi.org/10.1353/hpu.0.0058
Kales, H. (2000). Race, psychiatric diagnosis, and mental health care utilization in older patients. American Journal Of Geriatric Psychiatry, 8(4), 301-309. http://dx.doi.org/10.1176/appi.ajgp.8.4.301
Karim, S., Saeed, K., Rana, M., Mubbashar, M., & Jenkins, R. (2004). Pakistan mental health country profile. International Review Of Psychiatry, 16(1-2), 83-92. http://dx.doi.org/10.1080/09540260310001635131
Kartje, G., Schwab, M., O’Brien, T., Alsbiei, T., Tsai, S., & Papadopoulos, C. (2002). Functional recovery and neuroanatomical plasticity following middle cerebral artery occlusion and IN-1 antibody treatment in the adult rat. Annals Of Neurology, 51(4), 433-441. http://dx.doi.org/10.1002/ana.10144
Keefe, K., Nelson, T., & Cardemil, E. (2015). Racial and ethnic disparities in depression treatment. Current Opinion In Psychology, 4, 37-42. http://dx.doi.org/10.1016/j.copsyc.2015.01.021
Kitayama, S., & Markus, H. (1998). The cultural psychology of personality. Journal Of Cross-Cultural Psychology, 29(1), 63-87. http://dx.doi.org/10.1177/0022022198291004
Kleinman, A., Chieu, M., Lee, M., & Lee, S. (2005). Experience of social stigma by people with schizophrenia in Hong Kong. The British Journal Of Psychiatry, 186(2), 153-157. http://dx.doi.org/10.1192/bjp.186.2.153
Knifton, L. (2012). Understanding and addressing the stigma of mental illness with ethnic minority communities. Health Sociology Review, 21(3), 287-298. http://dx.doi.org/10.5172/hesr.2012.21.3.287
Knifton, L., Gervais, M., Newbigging, K., Mirza, N., Quinn, N., Wilson, N., & Hunkins-Hutchison, E. (2009). Community conversation: addressing mental health stigma with ethnic minority communities. Social Psychiatry And Psychiatric Epidemiology, 45(4), 497-504. http://dx.doi.org/10.1007/s00127-009-0095-4
Kovandžić, M., Chew-Graham, C., Reeve, J., Edwards, S., Peters, S., & Edge, D. et al. (2011). Access to primary mental health care for hard-to-reach groups: From ‘silent suffering’ to ‘making it work’. Social Science & Medicine, 72(5), 763-772. http://dx.doi.org/10.1016/j.socscimed.2010.11.027
Kulkarni, M., Gone, J., & Pole, N. (2008). Posttraumatic stress disorder among Ethnoracial minorities in the United States. Clinical Psychology: Science And Practice, 15(1), 35-61. http://dx.doi.org/10.1111/j.1468-2850.2008.00109.x
Lancet, T. (2016). The health crisis of mental health stigma. The Lancet, 387(10023), 1027. http://dx.doi.org/10.1016/s0140-6736(16)00687-5
Larson, S., Edlund, M., & Harris, K. (2005). Racial and ethnic differences in the mental health problems and use of mental health care. Medical Care, 43(8), 775-784. http://dx.doi.org/10.1097/01.mlr.0000170405.66264.23
Lê Cook, B., McGuire, T., Lock, K., & Zaslavsky, A. (2010). Comparing Methods of Racial and Ethnic Disparities Measurement across Different Settings of Mental Health Care. Health Services Research, 45(3), 825-847. http://dx.doi.org/10.1111/j.1475-6773.2010.01100.x
Lee, S., Lee, M., Chieu, M., & Kleinman, A. (2005). Experience of social stigma by people with schizophrenia in Hong Kong. The British Journal Of Psychiatry, 186(2), 153-157. http://dx.doi.org/10.1192/bjp.186.2.153
Link, B., Vega, E., Alvarado, R., Thornicroft, G., & Yang, L. (2014). Recent advances in cross-cultural measurement in psychiatric epidemiology: Utilizing ‘what matters most’ to identify culture-specific aspects of stigma. International Journal Of Epidemiology, 43(2), 494-510. http://dx.doi.org/10.1093/ije/dyu039
Manderscheid, R., Ryff, C., Freeman, E., McKnight-Eily, L., Dhingra, S., & Strine, T. (2010). Evolving Definitions of Mental Illness and Wellness. Preventing Chronic Disease. Public Health Research, Practice And Policy, 7(1), A19. Retrieved from https://www.cdc.gov/pcd/
Memon, A., Taylor, K., Mohebati, L., Sundin, J., Cooper, M., Scanlon, T., & de Visser, R. (2016). Perceived barriers to accessing mental health services among black and minority ethnic (BME) communities: a qualitative study in Southeast England. BMJ Open, 6(11), e012337. http://dx.doi.org/10.1136/bmjopen-2016-012337
Miranda, J., McGuire, T., & Cook, B. (2007). Measuring trends in mental health care disparities, 2000 2004. Psychiatric Services, 58(12), 1533-1540. http://dx.doi.org/10.1176/appi.ps.58.12.1533
Mulder, C., van Baars, A., de Vries, S., & Vinkers, D. (2009). Ethnicity and dangerousness criteria for court ordered admission to a psychiatric hospital. Social Psychiatry And Psychiatric Epidemiology, 45(2), 221-224. http://dx.doi.org/10.1007/s00127-009-0058-9
National institute of mental health. (2003). Choice Reviews Online, 40(12), 40Sup-0580-40Sup-0580. http://dx.doi.org/10.5860/choice.40sup-0580
Nazroo, J. (2003). The Structuring of Ethnic Inequalities in Health: Economic Position, Racial Discrimination, and Racism. American Journal Of Public Health, 93(2), 277-284. http://dx.doi.org/10.2105/ajph.93.2.277
Östman, M., & Kjellin, L. (2005). Relatives of psychiatric inpatients – do physical violence and suicide attempts of patients influence family burden and participation in care?. Nordic Journal Of Psychiatry, 59(1), 7-11. http://dx.doi.org/10.1080/08039480510018850
Papadopoulos, C., Foster, J., & Caldwell, K. (2012). ‘Individualism-Collectivism’ as an Explanatory Device for Mental Illness Stigma. Community Mental Health Journal, 49(3), 270-280. http://dx.doi.org/10.1007/s10597-012-9534-x
Papadopoulos, C., Tsai, S., Alsbiei, T., O’Brien, T., Schwab, M., & Kartje, G. (2002). Functional recovery and neuroanatomical plasticity following middle cerebral artery occlusion and IN-1 antibody treatment in the adult rat. Annals Of Neurology, 51(4), 433-441. http://dx.doi.org/10.1002/ana.10144
Pettigrew, T., & Tropp, L. (2006). A meta-analytic test of intergroup contact theory. Journal Of Personality And Social Psychology, 90(5), 751-783. http://dx.doi.org/10.1037/0022-3514.90.5.751
Phelan, S., Medasani, K., Slopen, N., Goldman, H., Lurie, B., & Corrigan, P. (2005). How adolescents perceive the stigma of mental illness and alcohol abuse. Psychiatric Services, 56(5), 544-550. http://dx.doi.org/10.1176/appi.ps.56.5.544
Phelan, S., van Ryn, M., Hargreaves, M., Ding, Y., & Burgess, D. (2008). The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. Journal Of Health Care For The Poor And Underserved, 19(3), 894-911. http://dx.doi.org/10.1353/hpu.0.0063
Pole, N., Gone, J., & Kulkarni, M. (2008). Posttraumatic Stress Disorder Among Ethnoracial Minorities in the United States. Clinical Psychology: Science And Practice, 15(1), 35-61. http://dx.doi.org/10.1111/j.1468-2850.2008.00109.x
Polit-O’Hara, D., & Beck, C. (2006). Essentials of nursing research (1st ed.). Philadelphia: Lippincott Williams & Wilkins.
RALEIGH, V., IRONS, R., HAWE, E., SCOBIE, S., COOK, A., & REEVES, R. et al. (2007). Ethnic variations in the experiences of mental health service users in England: Results of a national patient survey programme. The British Journal Of Psychiatry, 191(4), 304-312. http://dx.doi.org/10.1192/bjp.bp.106.032417
Rehman, H., & Owen, D. (2013). MENTAL HEALTH SURVEY OF ETHNIC MINORITIES. time-to-change.org.uk. Retrieved 4 May 2017, from https://www.time-to-change.org.uk/sites/default/files/TTC_Final%20Report_ETHNOS_summary_0.pdf
Ritchie, J. (2014). Qualitative research practice (1st ed.). Los Angeles, Calif.: SAGE.
Rosenheck, R., Ighodaro, A., Leddy, M., Ofori-Atta, A., Neto, H., & Cavalcanti, M. et al. (2016). Witchcraft and Biopsychosocial causes of mental illness. The Journal Of Nervous And Mental Disease, 204(3), 169-174. http://dx.doi.org/10.1097/nmd.0000000000000422
Rubin, H., & Rubin, I. (2012). Qualitative interviewing (1st ed.). Thousand Oaks, Calif.: SAGE.
Rüsch, N., Angermeyer, M., & Corrigan, P. (2005). Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry, 20(8), 529-539. http://dx.doi.org/10.1016/j.eurpsy.2005.04.004
Rüsch, N., Jones, N., Schmidt, A., Bink, A., & Corrigan, P. (2015). What is the impact of self-stigma? Loss of self-respect and the “why try” effect. Journal Of Mental Health, 25(1), 10-15. http://dx.doi.org/10.3109/09638237.2015.1021902
Rüsch, N., Rafacz, J., Michaels, P., Morris, S., & Corrigan, P. (2012). Challenging the public stigma of mental illness: A Meta-Analysis of outcome studies. Psychiatric Services, 63(10), 963-973. http://dx.doi.org/10.1176/appi.ps.201100529
Saltus, R., Downes, C., Jarvis, P., & Duval, S. (2013). Inpatients from black and minority ethnic backgrounds in mental health services in Wales: a secondary analysis of the Count Me In census, 2005–2010. Diversity And Equality In Health And Care, 10, 165-76.
Sartorius, N., Kassam, A., Rose, D., & Thornicroft, G. (2007). Stigma: Ignorance, prejudice or discrimination?. The British Journal Of Psychiatry, 190(3), 192-193. http://dx.doi.org/10.1192/bjp.bp.106.025791
Scherder, E., Harte, J., van Esch, A., & Denzel, A. (2016). Ethnic variations in psychotic disorders in the criminal justice system: A systematic review. Aggression And Violent Behavior, 29, 20-29. http://dx.doi.org/10.1016/j.avb.2016.05.006
Schwartz, R., & Blankenship, D. (2014). Racial disparities in psychotic disorder diagnosis: A review of empirical literature. World Journal Of Psychiatry, 4(4), 133. http://dx.doi.org/10.5498/wjp.v4.i4.133
Scior, K., Mutter, R., & Donner, B. (2010). Mainstream in-patient mental health care for people with intellectual disabilities: Service user, Carer and provider experiences. Journal Of Applied Research In Intellectual Disabilities, 23(3), 214-225. http://dx.doi.org/10.1111/j.1468-3148.2009.00527.x
Scottham, K., Sellers, R., & Nguyên, H. (2008). A measure of racial identity in African American adolescents: The development of the Multidimensional Inventory of Black Identity–Teen. Cultural Diversity And Ethnic Minority Psychology, 14(4), 297-306. http://dx.doi.org/10.1037/1099-9809.14.4.297
Sells, M., Larson, J., Corrigan, P., & Watson, A. (2006). Self-stigma in people with mental illness. Schizophrenia Bulletin, 33(6), 1312-1318. http://dx.doi.org/10.1093/schbul/sbl076
Selten, J., van Brussel, G., Tuinebreijer, W., & de Wit, M. (2010). Ethnic differences in risk of acute compulsory admission in Amsterdam, 1996–2005. Social Psychiatry And Psychiatric Epidemiology, 47(1), 111-118. http://dx.doi.org/10.1007/s00127-010-0312-1
Shaw, R. (2010). Embedding Reflexivity Within Experiential Qualitative Psychology. Qualitative Research In Psychology, 7(3), 233-243. http://dx.doi.org/10.1080/14780880802699092
Shefer, G., Rose, D., Nellums, L., Thornicroft, G., Henderson, C., & Evans-Lacko, S. (2013). ‘Our community is the worst’: The influence of cultural beliefs on stigma, relationships with family and help-seeking in three ethnic communities in London. International Journal Of Social Psychiatry, 59(6), 535-544. http://dx.doi.org/10.1177/0020764012443759
Shinebourne, P., & Smith, J. (2010). The communicative power of metaphors: An analysis and interpretation of metaphors in accounts of the experience of addiction. Psychology And Psychotherapy: Theory, Research And Practice, 83(1), 59-73. http://dx.doi.org/10.1348/147608309×468077
Simmons, L., & Dardas, L. (2015). The stigma of mental illness in Arab families: A concept analysis. Journal Of Psychiatric And Mental Health Nursing, 22(9), 668-679. http://dx.doi.org/10.1111/jpm.12237
Simpson, E. (2002). Involving users in the delivery and evaluation of mental health services: systematic review. BMJ, 325(7375), 1265-1265. http://dx.doi.org/10.1136/bmj.325.7375.1265
Skoldberg, K., Sköldberg, K., & Alvesson, M. (2009). Reflexive methodology: New vistas for qualitative research. Thousand Oaks, CA: SAGE Publications.
Smith, J. (2014). Qualitative psychology (1st ed.). Los Angeles [etc.]: Sage.
Snowden, L., & Yamada, A. (2005). Cultural Differences in Access to Care. Annual Review Of Clinical Psychology, 1(1), 143-166. http://dx.doi.org/10.1146/annurev.clinpsy.1.102803.143846
Strine, T., Dhingra, S., McKnight-Eily, L., Freeman, E., Ryff, C., & Manderscheid, R. (2010). Evolving Definitions of Mental Illness and Wellness. Public Chronic Disease Public Health Research, Practise, And Policy, 7(1), A19.
Stuart, H. (2006). Media portrayal of mental illness and its treatments. CNS Drugs, 20(2), 99-106. http://dx.doi.org/10.2165/00023210-200620020-00002
Sue, D., Capodilupo, C., Torino, G., Bucceri, J., Holder, A., Nadal, K., & Esquilin, M. (2007). Racial microaggressions in everyday life: Implications for clinical practice. American Psychologist, 62(4), 271-286. http://dx.doi.org/10.1037/0003-066x.62.4.271
Sue, S., Zane, N., Nagayama Hall, G., & Berger, L. (2009). The Case for Cultural Competency in Psychotherapeutic Interventions. Annual Review Of Psychology, 60(1), 525-548. http://dx.doi.org/10.1146/annurev.psych.60.110707.163651
Szczepura, A., Ardino, V., Knapp, M., Singh, S., Weich, S., & Johnson, M. et al. (2015). Interventions designed to improve therapeutic communications between black and minority ethnic people and professionals working in psychiatric services: A systematic review of the evidence for their effectiveness. Health Technology Assessment, 19(31), 1-174. http://dx.doi.org/10.3310/hta19310
Szmukler, G., Sutherby, K., Thornicroft, G., Leese, M., Flood, C., & Henderson, C. (2004). Effect of joint crisis plans on use of compulsory treatment in psychiatry: Single blind randomised controlled trial. BMJ, 329(7458), 136-0. http://dx.doi.org/10.1136/bmj.38155.585046.63
Tansella, M., & Thornicroft, G. (2005). Growing recognition of the importance of service user involvement in mental health service planning and evaluation. Epidemiologia E Psichiatria Sociale, 14(01), 1-3. http://dx.doi.org/10.1017/s1121189x00001858
The criminal justice system. (2007). Nacro Black Communities. Retrieved from http://www.ohrn.nhs.uk/resource/policy/Nacroblackcommunities.pdf
Thomas, S., Blackburn, E., Lin, J., Taylor, R., Lincoln, K., & Nuru-Jeter, A. et al. (2016). Discrimination, mental health, and leukocyte telomere length among African American men. Psychoneuroendocrinology, 63, 10-16. http://dx.doi.org/10.1016/j.psyneuen.2015.09.001
Thornicroft, G. (2007). Shunned: Discrimination against people with mental illness (1st ed.). OXFORD: Oxford University Press.
Thornicroft, G., & Tansella, M. (2005). Growing recognition of the importance of service user involvement in mental health service planning and evaluation. Epidemiologia E Psichiatria Sociale, 14(01), 1-3. http://dx.doi.org/10.1017/s1121189x00001858
Thornicroft, G., Mehta, N., Clement, S., Evans-Lacko, S., Doherty, M., & Rose, D. et al. (2016). Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet, 387(10023), 1123-1132. http://dx.doi.org/10.1016/s0140-6736(15)00298-6
Thornicroft, G., Rose, D., Kassam, A., & Sartorius, N. (2007). Stigma: ignorance, prejudice or discrimination?. The British Journal Of Psychiatry, 190(3), 192-193. http://dx.doi.org/10.1192/bjp.bp.106.025791
Tilley, S., & Powick, K. (2002). Distanced Data: Transcribing Other People’s Research Tapes. Canadian Journal Of Education / Revue Canadienne De L’éducation, 27(2/3), 291. http://dx.doi.org/10.2307/1602225
Tongco, M. (2007). Purposive sampling as a tool for informant selection. Ethnobotany Research And Applications, 5, 147. http://dx.doi.org/10.17348/era.5.0.147-158
Tongco, M. (2007). Purposive Sampling as a Tool for Informant Selection. Ethnobotany Research And Applications, 5, 147. http://dx.doi.org/10.17348/era.5.0.147-158
Trimble, J., & Gone, J. (2012). American Indian and Alaska native mental health: Diverse perspectives on enduring disparities. Annual Review Of Clinical Psychology, 8(1), 131-160. http://dx.doi.org/10.1146/annurev-clinpsy-032511-143127
Tropp, L., & Pettigrew, T. (2006). A meta-analytic test of intergroup contact theory. Journal Of Personality And Social Psychology, 90(5), 751-783. http://dx.doi.org/10.1037/0022-3514.90.5.751
Vinkers, D., de Vries, S., van Baars, A., & Mulder, C. (2009). Ethnicity and dangerousness criteria for court ordered admission to a psychiatric hospital. Social Psychiatry And Psychiatric Epidemiology, 45(2), 221-224. http://dx.doi.org/10.1007/s00127-009-0058-9
Wahl, O. (1999). Mental health consumers’ experience of stigma. Schizophrenia Bulletin, 25(3), 467-478. http://dx.doi.org/10.1093/oxfordjournals.schbul.a033394
Walsh, R. (2003). The methods of reflexivity. The Humanistic Psychologist, 31(4), 51-66. http://dx.doi.org/10.1080/08873267.2003.9986934
Watson, A., & Corrigan, P. (2002). The paradox of self-stigma and mental illness. Clinical Psychology: Science And Practice, 9(1), 35-53. http://dx.doi.org/10.1093/clipsy.9.1.35
Watson, A., & Corrigan, P. (2004). Stigma and public education about mental illness. Psychiatric Services, 55(7), 834-a-835. http://dx.doi.org/10.1176/appi.ps.55.7.834-a
Wengraf, T. (2011). Qualitative research interviewing (1st ed.). London [u.a.]: Sage.
Whitley, R. (2016). Ethno-Racial variation in recovery from severe mental illness: A qualitative comparison. The Canadian Journal Of Psychiatry, 61(6), 340-347. http://dx.doi.org/10.1177/0706743716643740
W. J., Nicholson, K. L., Dance, M. E., Morgan, R. W., & Foley, P. L. (2010). Animal models of substance abuse and addiction: implications for science, animal welfare, and society. Comparative medicine, 60(3), 177-188.
WHO | Mental health: a state of well-being. (2017). Who.int. Retrieved 8 April 2017, from http://www.who.int/features/factfiles/mental_health/en/
Yamada, A., & Snowden, L. (2005). Cultural differences in access to care. Annual Review Of Clinical Psychology, 1(1), 143-166. http://dx.doi.org/10.1146/annurev.clinpsy.1.102803.143846
Zaslavsky, A., Lock, K., McGuire, T., & Lê Cook, B. (2010). Comparing methods of racial and ethnic disparities measurement across different settings of mental health care. Health Services Research, 45(3), 825-847. http://dx.doi.org/10.1111/j.1475-6773.2010.01100.x
Appendices
Appendix A
Interview Guide
- To begin with, I would like you to know that this entirely voluntary and kept anonymously. This interview is not to make you feel awkward in any negative type of way or form. I hope you will enjoy this interview. This is also part of my research project where results will remain solely there. Firstly, your personal experiences, what do you know about mental health?
- Do you feel it is major problem for society that can’t be rectified?
SOCIAL PROBLEMS
- Have you ever been bullied or know someone who has been bullied?
- To what extent do you feel that this has impacted you OR your experience in____?
- Have you ever attempted to speak to professionals or access services available to you?
- How did you feel after your experience? Were you satisfied or feel it helped?
- If no, why? What do you find difficult in trying to get help from specialists?
ACADEMIC ISSUES
- Throughout your education life, have you struggled to deal with exam and assignment deadlines? In what way?
- What have you done to adapt to this?
- How did you cope with balancing different modules all at the same time?
- Did past teachers try to diagnose you for acting out or misbehavior? How did you feel about this?
- How have you found it trying to achieve high grades in your studies compared to your courses in college/sixth-form?
- How easy/ difficult have you found access to tutors/lecturers/module leaders for support?
- Do you feel you’re targeted or labeled by teachers?
- What mistreatment have you encountered during education?
FINANCIAL DIFFICULTIES
- Have you ever been emotionally distressed because of your previous work or current work in terms of occupation?
- How have you found balancing work and having a positive mind frame?
- Have you been affected by your job security?
- If so, how do you deal with rising anxieties?
- Do you feel you get a lack of support from well-being services at work?
- Lack of empathy for home issues whilst at work?
RELIGIOUS INFLUENCE
- If you don’t mind me asking, do you follow a religion?
- Does your religion affect your perception of mental health?
- If so, how?
- What are some of the beliefs your religion speaks about in regards to mental and emotional issues someone faces?
- How would someone from your ethnic background normally behave around someone with a mental illness such as schizophrenia?
CULTURE IMPACT
- Why do you think people are more stigmatized here than in your native country?
- Do you feel your parents and country of origin’s culture has influenced you?
- Do you believe your cultural influences have stayed with you in regards to your views about mental health?
MENTAL HEALTH STIGMA
- Can you share a time when a person or group of people unintentionally upset you, perhaps due to their own lack of awareness of mental health truths?
- Why do you think there is a rise of BME people being admitted to mental health services through CJS (police, courts, prisons)?
- Do you feel BME people face police brutality or targeting??
- If so, how?
- What have your experiences so far led you to believe about mental health stigma?
- Do you feel people do not care what BME people say in regards to their emotions?
- Statistics show BME groups are overrepresented in mental health, what are your views about this?
- What would you suggest to change this?
- Have you ever attempted to access mental health services?
- How has that experience changed your perception of mental illness?
- Why do you think getting help for mental illness is so difficult for so many individuals from the BME community?
- What challenges do you think individuals with a mental illness face while they are trying to recover?
- What suggestions would you propose to improve access to mental health services by the BME community?
- Also what suggestion would you propose for treatments?
- That’s literally everything I wanted to speak about, do you have any thoughts or wanted to speak about anything I’ve asked you?
Appendix B
PARTICIPANT CONSENT FORM
–
THIS CONSENT FORM MUST BE SIGNED BY ALL PARTICIPANTS BEFORE THEY TAKE PART IN THE STUDY AND THESE FORMS WILL BE RETAINED SECURELY BY THE UNIVERSITY FOR 5 YEARS.
Division of Psychology
Researcher: Ashley K. Atuahene
Research Project: BME Perspective: The Stigma Behind BME Groups And Mental Health
Forename: ………………………………………………………………………………………………………………….
Surname: ……………………………………………………………………………………………………………………
Signature of Participant: …………………………………………………………………………………………….
Signature of Researcher: …………………………………………………………………………………………….
Date: …………………………………………………………………………………………………………………………..
The researcher has fully explained the research to me and my participation within this project. I have been given the opportunity to ask any questions.
I understand that I do not have to answer any questions I do not wish to answer or any discussion I do not feel comfortable with.
I realise that I may stop taking part in the study at any time without giving a reason and without causing any problems.
I have been given information with the researcher’s name and email address if I require any more information.
I understand that the discussion will be audio-recorded and that only the researcher will hear this recorded version.
I understand that all conversations that happen between me and the researcher should be kept private. In full agreement with the researcher, we will both therefore not share any of what is said with the researcher outside of this interview out of respect for me, whom has taken part.
I give my permission for the things I say in the discussion to be used in the researchers final report, under another name or using my initials to protect my identity.
I hereby give my consent to take part in this study.
Appendix C
PARTICIPANT INFORMATION SHEET
BME PERSPECTIVE: THE STIGMA BEHIND BME GROUPS AND MENTAL HEALTH
Division of Psychology
I am a final year undergraduate student studying Psychology (BSc) at Birmingham City University (BCU). My research project focuses on exploring the stigma behind BME groups and mental health. I am keen on learning about some of your opinions and knowledge regarding mental health and how it affects BME people around you.
A one-to-one interview would be conducted by myself, the interviewer and involve you, the participant as the interviewee. This would last for approximately 30 minutes. An informal discussion will take place regarding your experiences and understandings of how BME individuals are affected by mental health. I hope you will find this an enjoyable experience. With your consent, the interview would, be audio recorded, and will be written by me personally. I will ensure to retain strict confidentiality regarding this information.
This is an entirely voluntary participation where you would be able to leave from the project from any given time, without giving reasons, prior to, and during, the interview. Additionally, you would have the opportunity to withdraw all or part of your interview material from the study for up to three months after the interview has taken place. All information you provide in an interview will not be spoken of outside this research. Any identifying information such as your name will be changed to an alternative name or your initials given to any of your data used in publications arising from this research.
Thank you very much for your time and kindly considering to take part. If you have any queries, or wish to know more, please take a look at my contact details for further information.
Head Researcher:
Email:
Supervisor:
Email:
Appendix D
Division of Psychology
Debrief
Past research has focused on stigma and mental health but not from BME perspectives. Black minorities are underrepresented in prior research and the effects of stigma in these communities have been neglected. There has been a disproportionate level of evidence that point to why this has escalated during last few decades. Hence, my goal is seek how BME groups deal with stigma around mental health in their daily lives.
Thank you very much for your participation. I kindly appreciate you for considering taking part in this study. Your views will be kept confidential and will only be used anonymously for research purposes. If you would like to speak to the BCU mental health and well being services after this interview will be available through: 0121 331 7777 or www.bcu.ac.uk/askus.
If you have any further questions please do not hesitate to contact:
Head Researcher:
Email:
Supervisor:
Email:
Appendix E
Appendix F
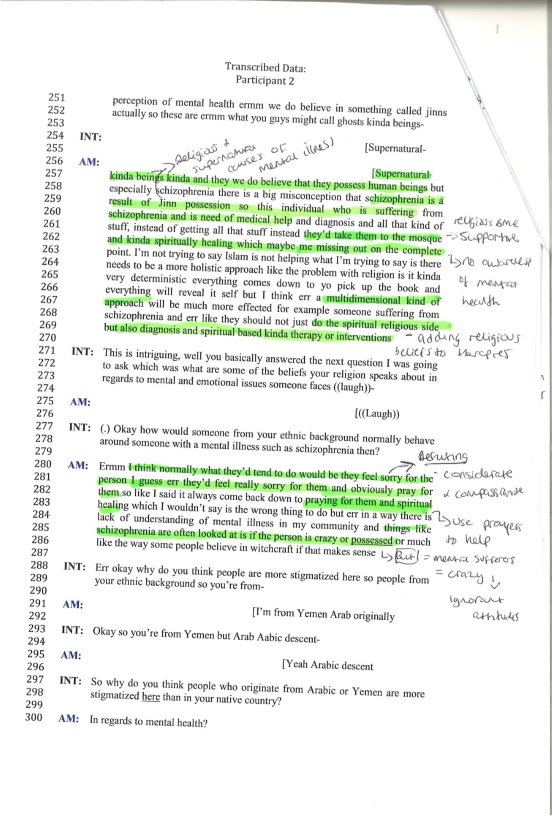
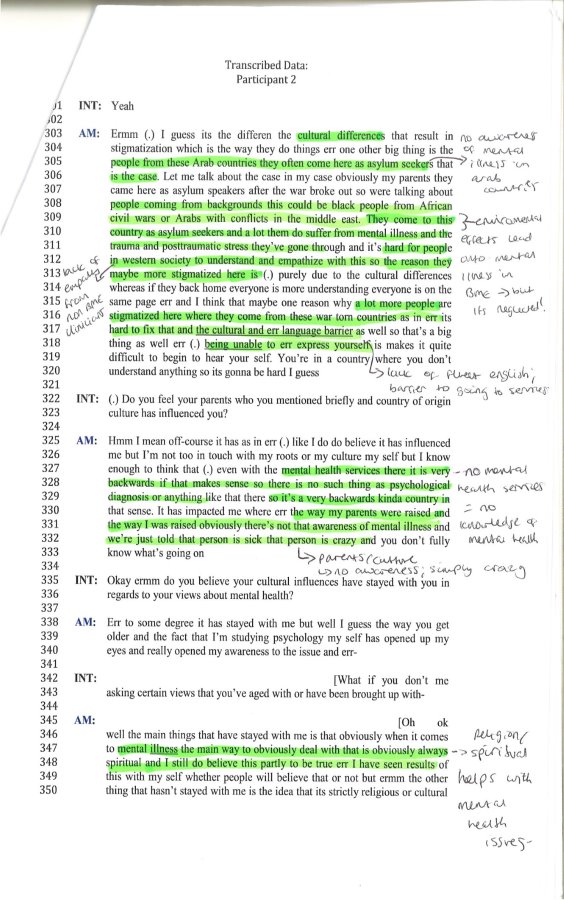
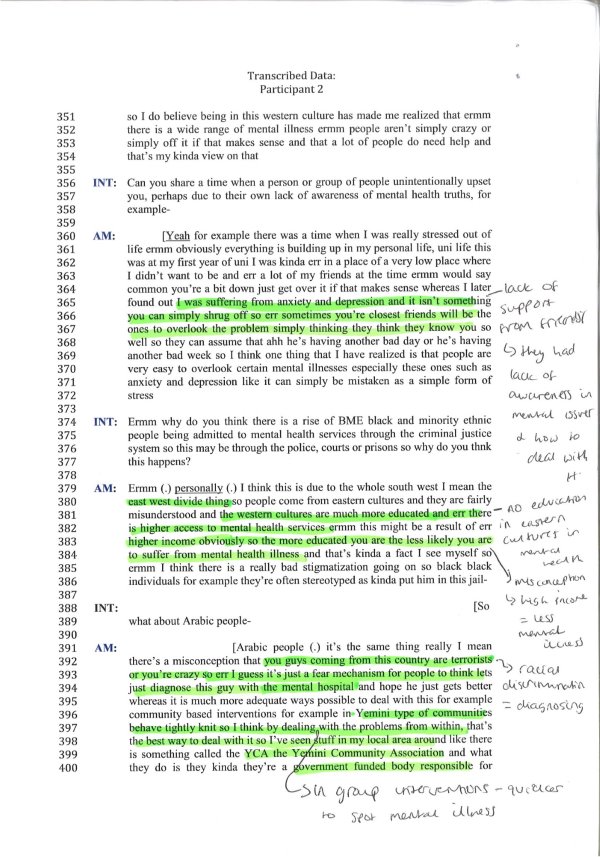
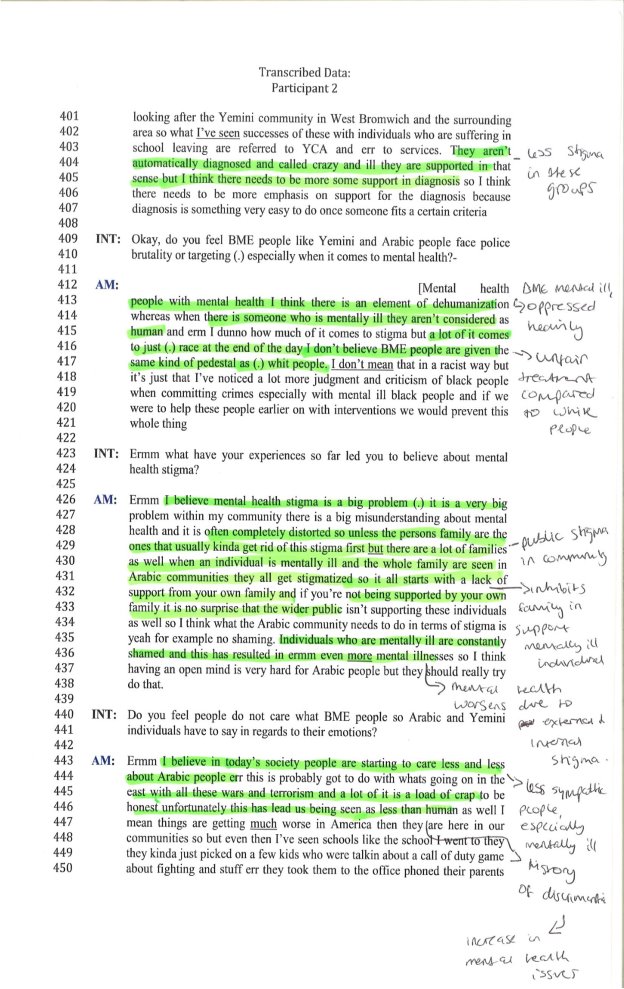
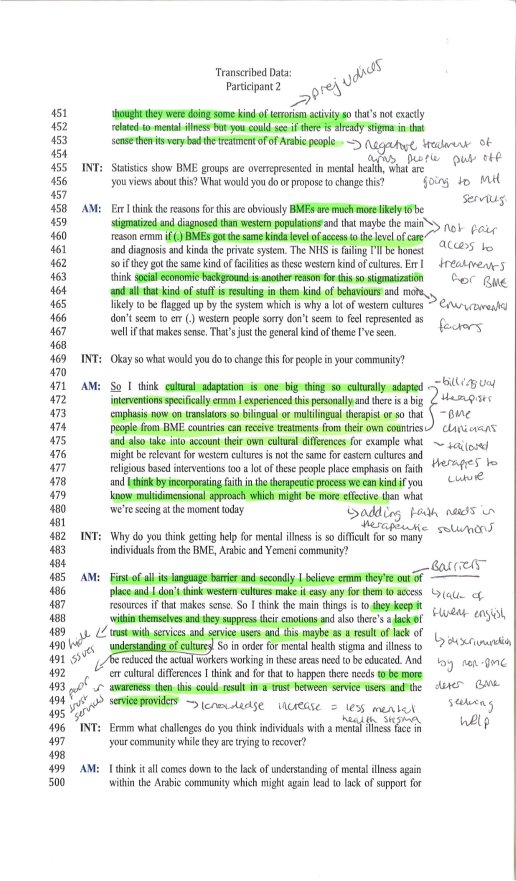
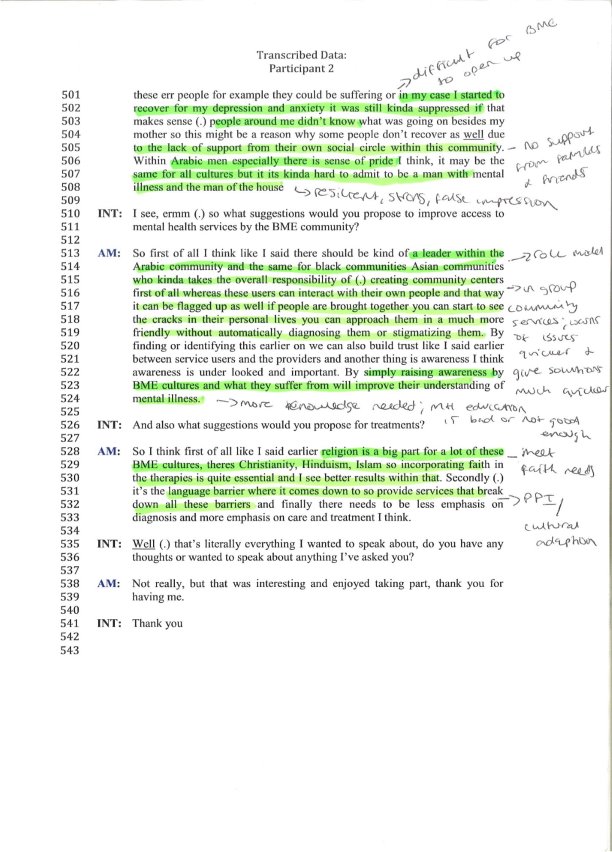
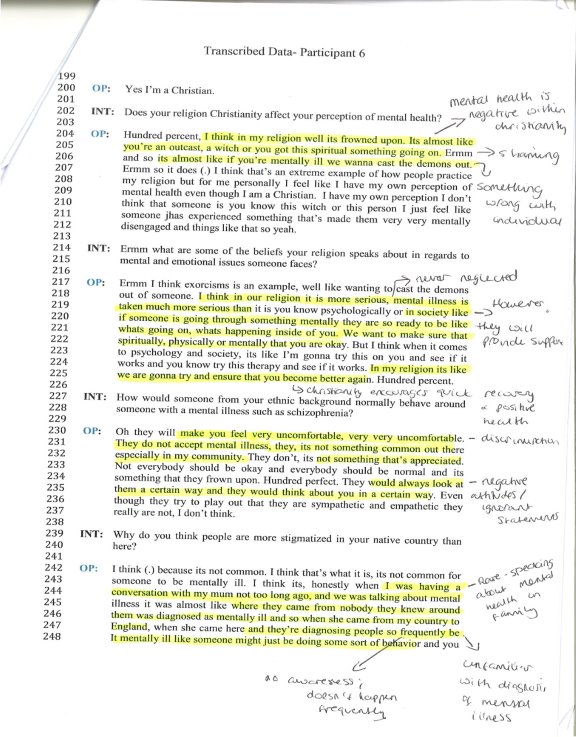
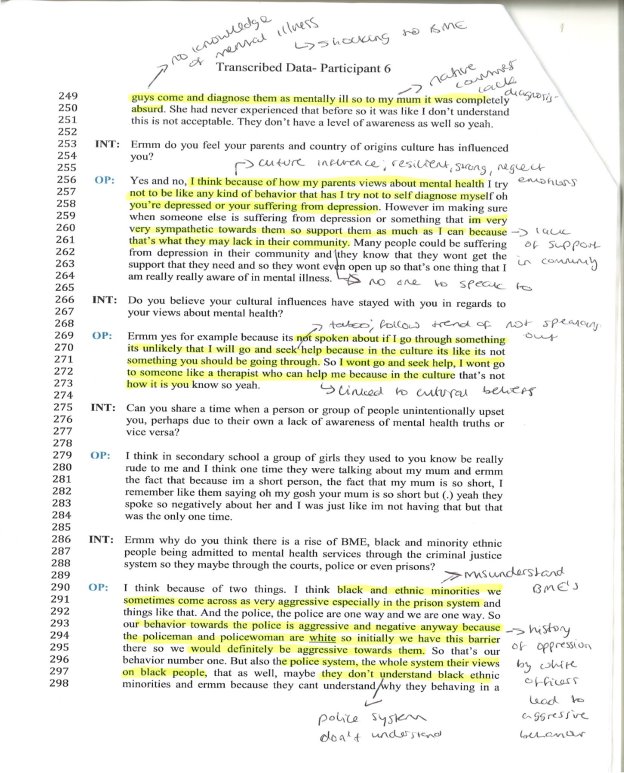
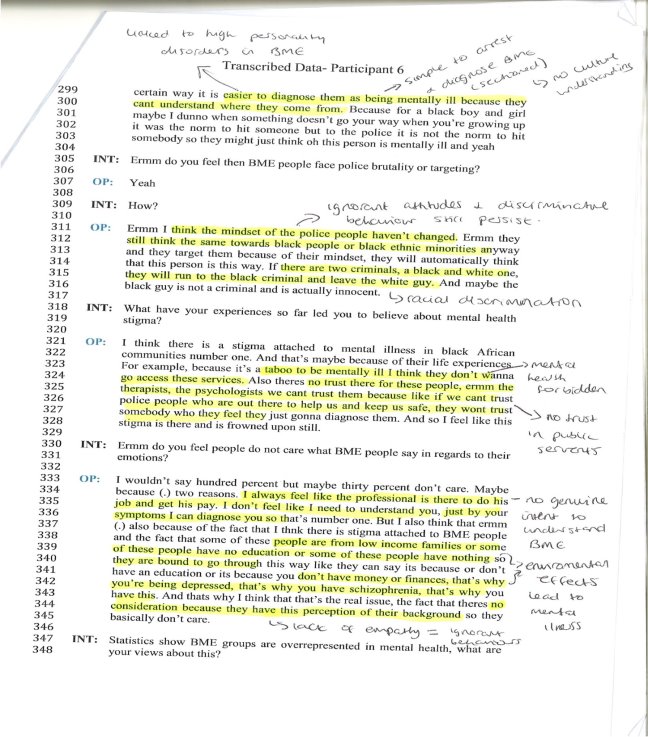
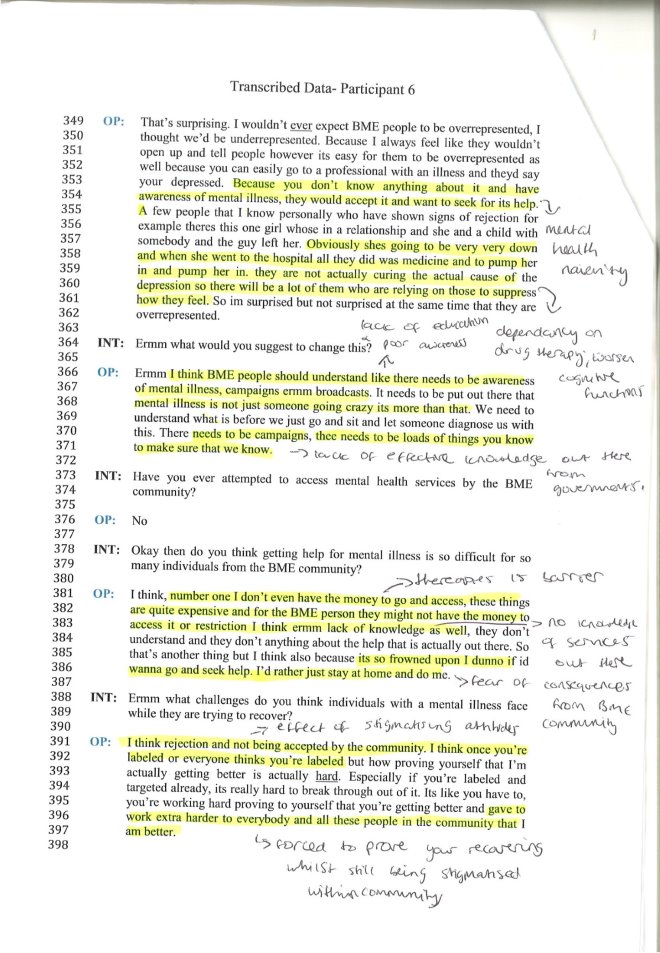
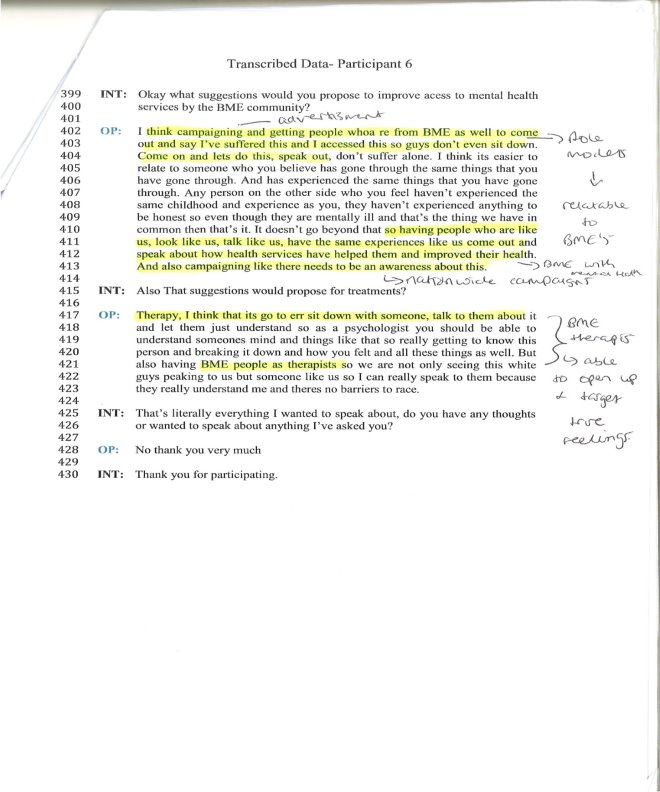
Appendix G
Log Sheet
| Session 1 – Issues discussed | Advice given: | Action to be taken: |
| Proposal Topic
|
Key authors in research topic area were suggested. Discussed appropriate methodology and to improve on writing skills. Student wants to aim for a 1st so advice was tailored to writing high calibre piece of research. | Take a look at Thornicroft; start basis of research from here and discover what stigma is.
Start using crib sheets to effectively appraise theories, studies and methodologies.
|
|
Date: 07/10/2016 (20 minutes) |
Signature of supervisor:
|
Signature of
student: Atuahene.A.K.Ashley |
| Session 2 – Issues discussed | Advice given: | Action to be taken: |
| Proposal Formative Feedback | More expansion in paragraphs needed. A lot of ambiguous words and phrases. Lack of references and use of third person throughout. | Reword sentences that lack clarity
Proofread so there is flow in writing
|
|
Date: 10/11/2016 (20 minutes) |
Signature of supervisor:
|
Signature of
student: Atuahene.A.K.Ashley |
Appendix H
UCEEL Copyright Waiver
Student Name: Ashley Kwabena Atuahene
Project/Thesis Title: BME Perspective: The Stigma Behind BME Groups And Mental Health
Course: Psychology
Student Agreement
1. I confirm that Birmingham City University can electronically archive and make accessible the project / thesis described above via the UCEEL Electronic Library system. I retain all other ownership rights to the copyright of the document / project work described above.
2. I confirm the above project / thesis is a true and unaltered representation of the project / thesis as submitted to Birmingham City University course tutors and examiners.
3. I confirm that the above project / thesis includes material copied from a source (e.g. a book) where ownership of the copyright does not belong to myself.
If the project / thesis doesn’t include such materialplease supply the following details:
a) Page reference / item reference:
b) I have obtained and attached a written permission statement from the owner(s) of each third party copyrighted matter included in my project / thesis
No
(If No, I understand the electronic copy of my project / thesis available on UCEEL will omit these sections from view)
Signature: __________________________________________________________
Print Name: __________________________________________________________
Date: 28/04/2017 __________________________________________________________
N.B. If you are at anytime in consultation with a publisher regarding this work you will need to declare the copy held on UCEEL. Some publishers may regard the UCEEL copy as constituting prior publication. The copy can be removed from UCEEL if it becomes an obstacle to future commercial publication.
Official Use only
ORION unique number: ________________ Date added to the system: ________________
IS228a/Oct07
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Mental Health"
Mental Health relates to the emotional and psychological state that an individual is in. Mental Health can have a positive or negative impact on our behaviour, decision-making, and actions, as well as our general health and well-being.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:





